Imagine a world in which a vaccine is a cream you rub onto your skin instead of a needle a health care worker pushes into your one of your muscles. Even better, it’s entirely pain-free and not followed by fever, swelling, redness or a sore arm. No standing in a long line to get it. Plus, it’s cheap.
Thanks to Stanford University researchers’ domestication of a bacterial species that hangs out on the skin of close to everyone on Earth, that vision could become a reality.
“We all hate needles everybody does,” said Michael Fischbach, PhD, the Liu (Liao) Family Professor and a professor of bioengineering. “I haven’t found a single person who doesn’t like the idea that it’s possible to replace a shot with a cream.”
The skin is a terrible place to live, according to Fischbach. “It’s incredibly dry, way too salty for most single-celled creatures and there’s not much to eat. I can’t imagine anything would want to live there.”
But a few hardy microbes call it home. Among them is Staphylococcus epidermidis, a generally harmless skin-colonizing bacterial species.
“These bugs reside on every hair follicle of virtually every person on the planet,” Fischbach said.
Immunologists have perhaps neglected our skin-colonizing bacteria, Fischbach said, because they don’t seem to contribute much to our well-being. “We’ve just assumed there’s not much going on there.”
That turns out to be wrong. In recent years, Fischbach and his colleagues have discovered that the immune system mounts a much more aggressive response against S. epidermidis than anyone expected.
In a study published Dec. 11 in Nature, Fischbach and his colleagues zeroed in on a key aspect of the immune response — the production of antibodies. These specialized proteins can stick to specific biochemical features of invading microbes, often preventing them from getting inside of cells or traveling unmolested through the bloodstream to places they should not go. Individual antibodies are extremely picky about what they stick to. Each antibody molecule typically targets a particular biochemical feature belonging to a single microbial species or strain.
Fischbach and postdoctoral scholar Djenet Bousbaine, PhD, respectively the study’s senior and lead author, and their colleagues wanted to know: Would the immune system of a mouse, whose skin isn’t normally colonized by S. epidermidis, mount an antibody response to that microorganism if it were to turn up there?
(Antibody) levels without a cause?
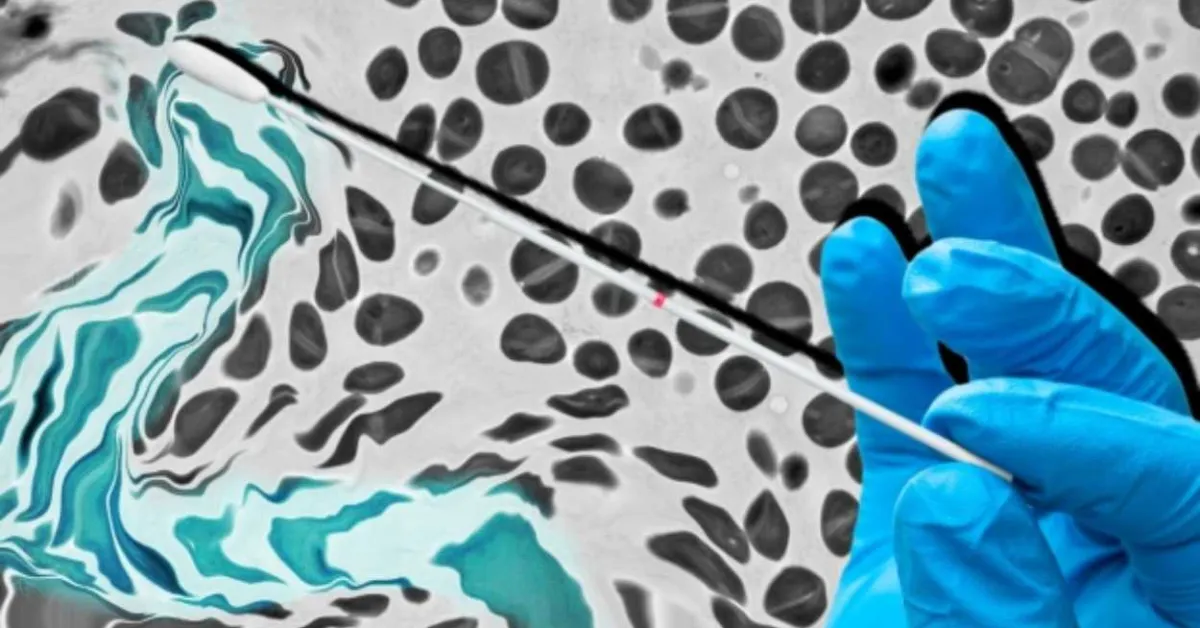
The initial experiments, performed by Bousbaine, were simple: Dip a cotton swab into a vial containing S. epidermidis. Rub the swab gently on the head of a normal mouse — no need to shave, rinse or wash its fur — and put the mouse back in its cage. Draw blood at defined time points over the next six weeks, asking: Has this mouse’s immune system produced any antibodies that bind to S. epidermidis?
The mice’s antibody response to S. epidermidis was “a shocker,” Fischbach said. “Those antibodies’ levels increased slowly, then some more — and then even more.” At six weeks, they’d reached a higher concentration than one would expect from a regular vaccination — and they stayed at those levels.
“It’s as if the mice had been vaccinated,” Fischbach said. Their antibody response was just as strong and specific as if it had been reacting to a pathogen.
“The same thing appears to be occurring naturally in humans,” Fischbach said. “We got blood from human donors and found that their circulating levels of antibodies directed at S. epidermidis were as high as anything we get routinely vaccinated against.”
That’s puzzling, he said: “Our ferocious immune response to these commensal bacteria loitering on the far side of that all-important anti-microbial barrier we call our skin seems to have no purpose.”
What’s going on? It could boil down to a line scrawled by early-20th-century poet Robert Frost: “Good fences make good neighbors.” Most people have thought that fence was the skin, Fischbach said. But it’s far from perfect. Without help from the immune system, it would be breached very quickly.
“The best fence is those antibodies. They’re the immune system’s way of protecting us from the inevitable cuts, scrapes, nicks and scratches we accumulate in our daily existence,” he said.
While the antibody response to an infectious pathogen begins only after the pathogen invades the body, the response to S. epidermidis happens preemptively, before there’s any problem. That way, the immune system can respond if necessary — say, when there’s a skin break and the normally harmless bug climbs in and tries to thumb a ride through our bloodstream.
Engineering a living vaccine
Step by step, Fischbach’s team turned S. epidermidis into a living, plug-and-play vaccine that can be applied topically. They learned that the part of S. epidermidis most responsible for tripping off a powerful immune response is a protein called Aap. This great, treelike structure, five times the size of an average protein, protrudes from the bacterial cell wall. They think it might expose some of its outermost chunks to sentinel cells of the immune system that periodically crawl through the skin, sample hair follicles, snatch snippets of whatever is flapping in Aap’s “foliage,” and spirit them back inside to show to other immune cells responsible for cooking up an appropriate antibody response aiming at that item.
(Fischbach is a co-author of a study led by Yasmine Belkaid, PhD, director of the Pasteur Institute and a co-author of the Fischbach team’s study, which will appear in the same issue of Nature. This companion study identifies the sentinel immune cells, called Langerhans cells, that alert the rest of the immune system to the presence of S. epidermidis on the skin.)
Aap induces a jump in not only blood-borne antibodies known to immunologists as IgG, but also other antibodies, called IgA, that home in on the mucosal linings of our nostrils and lungs.
“We’re eliciting IgA in mice’s nostrils,” Fischbach said. “Respiratory pathogens responsible for the common cold, flu and COVID-19 tend to get inside our bodies through our nostrils. Normal vaccines can’t prevent this. They go to work only once the pathogen gets into the blood. It would be much better to stop it from getting in in the first place.”
Having identified Aap as the antibodies’ main target, the scientists looked for a way to put it to work.
“Djenet did some clever engineering,” Fischbach said. “She substituted the gene encoding a piece of tetanus toxin for the gene fragment encoding a component that normally gets displayed in this giant treelike protein’s foliage. Now it’s this fragment — a harmless chunk of a highly toxic bacterial protein — that’s waving in the breeze.” Would the mice’s immune systems “see” it and develop a specific antibody response to it?
The investigators repeated the dip-then-swab experiment, this time using either unaltered S. epidermidis or bioengineered S. epidermidis encoding the tetanus toxin fragment. They administered several applications over six weeks. The mice swabbed with bioengineered S. epidermidis, but not the others, developed extremely high levels of antibodies targeting tetanus toxin. When the researchers then injected the mice with lethal doses of tetanus toxin, mice given natural S. epidermidis all succumbed; the mice that received the modified version remained symptom-free.
A similar experiment, in which the researchers snapped the gene for diphtheria toxin instead of the one for tetanus toxin into the Aap “cassette player,” likewise induced massive antibody concentrations targeting the diphtheria toxin.
The scientists eventually found they could still get life-saving antibody responses in mice after only two or three applications.
They also showed, by colonizing very young mice with S. epidermidis, that the bacteria’s prior presence on these mice’s skin (as is typical in humans but not mice) didn’t interfere with the experimental treatment’s ability to spur a potent antibody response. This implies, Fischbach said, that our species’ virtually 100% skin colonization by S. epidermidis should pose no problem to the construct’s use in people.
Look, ma, no limits
In a change of tactics, the researchers generated the tetanus-toxin fragment in a bioreactor, then chemically stapled it to Aap so it dotted S. epidermidis’s surface. To Fischbach’s surprise, this turned out to generate a surprisingly powerful antibody response. Fischbach had initially reasoned that the surface-stapled toxin’s abundance would get ever more diluted with each bacterial division, gradually muting the immune response. Just the opposite occurred. Topical application of this bug generated enough antibodies to protect mice from six times the lethal dose of tetanus toxin.
“We know it works in mice,” Fischbach said. “Next, we need to show it works in monkeys. That’s what we’re going to do.” If things go well, he expects to see this vaccination approach enter clinical trials within two or three years.
“We think this will work for viruses, bacteria, fungi and one-celled parasites,” he said. “Most vaccines have ingredients that stimulate an inflammatory response and make you feel a little sick. These bugs don’t do that. We expect that you wouldn’t experience any inflammation at all.”