About Authors: Ajay Kumar Pathak,
Analytical Science Division,
Shriram Institute for Industrial Research,
19 University Road, Delhi, 110007
Introduction
The plant kingdom comprises many species of plants containing substances of medicinal value, which are yet to be explored. A large number of plants are constantly being screened for their possible medicinal value.[12] The use of plant extracts in traditional medicine has been going on from ancient time.[13] Herbalism and folk medicine, both ancient and modern, have been the source of much useful therapy.[14-16] In the recent years, the development of resistance of pathogens against antibiotics has become a difficult issue caused by the indiscriminate use of modern antibiotics.[17-23] Therefore, the demand for new and effective antimicrobial agents with broad spectrum activities from natural sources are increasing day by day. Infectious diseases account for approximately one-half of all deaths in tropical countries. The use of and search for drugs and dietary supplements derived from plants have accelerated in recent years. Ethnopharmacologists, botanists, microbiologists, and natural-products chemists are combing the Earth for phytochemicals and "leads" which could be developed for treatment of infectious diseases. While 25 to 50% of current pharmaceuticals are derived from plants, none are used as antimicrobials.
Traditional healers have long used plants to prevent or cure infectious conditions; Western medicine is trying to duplicate their successes. Plants are rich in a wide variety of secondary metabolites, such as tannins, terpenoids, alkaloids, and flavonoids, which have been found in vitro to have antimicrobial properties. In industrialized nations, despite the progress made in the understanding of microbiology and their control, incidents of epidemics due to drug resistant microorganisms and the emergence of hitherto unknown disease-causing microbes, pose enormous public health concerns. Historically, plants have provided a good source of anti-infective agents; emetine, quinine, and berberine remain highly effective instruments in the fight against microbial infections. Phytomedicines derived from plants have shown great promise in the treatment of infectious diseases including opportunistic AIDS infections. Plants containing protoberberines and related alkaloids, picralima-type indole alkaloids and garcinia biflavonones used in traditional African system of medicine, have been found to be active against a wide variety of micro-organisms. The profile of known drugs like Hydrastis canadensis (goldenseal), Garcinia kola (bitter kola), Polygonum sp., Aframomum melegueta (grains of paradise) will be used to illustrate the enormous potential of anti-infective agents from higher plants.
[adsense:336x280:8701650588]
Reference ID: PHARMATUTOR-ART-1092
In the past few decades, a worldwide increase in the incidence of fungal infections has been observed as well as a rise in the resistance of some species of fungus to different fungicidals used in medicinal practice. Fungi are one of the most neglected pathogens, as demonstrated by the fact that the amphotericin B, a polyene antibiotic discovered as long ago as 1956, is still used as a “gold standard” for antifungal therapy [24]. The last two decades have witnessed a dramatic rise in the incidence of life threatening systemic fungal infections. The challenge has been to develop effective strategies for the treatment of candidiasis and other fungal diseases, considering the increase in opportunistic fungal infections in human immunodeficiency virus-positive patients and in others who are immunocompromised due to cancer chemotherapy and the indiscriminate use of antibiotics. The majority of clinically used antifungals have various drawbacks in terms of toxicity, efficacy and cost, and their frequent use has led to the emergence of resistant strains. Additionally, in recent years public pressure to reduce the use of synthetic fungicides in agriculture has increased. Concerns have been raised about both the environmental impact and the potential health risk related to the use of these compounds.
Hence, there is a great demand for novel antifungals belonging to a wide range of structural classes, selectively acting on new targets with fewer side effects. One approach might be the testing of plants traditionally used for their antifungal activities as potential sources for drug development. Medicinal plants are not only important to the millions of people for whom traditional medicine is the only opportunity for health care and to those who use plants for various purposes in their daily lives, but also as a source of new pharmaceuticals. Natural products, either as pure compounds or as standardized plant extracts, provide unlimited opportunities for new drug leads because of the matched less availability of chemical diversity. Since many of the compounds are currently available as unregulated botanical preparations and their use by the public is increasing rapidly, clinicians need to consider the consequences of patients self-medicating with these preparations.
[adsense:468x15:2204050025]
Antibiotics belong to the broader group of antimicrobial compounds, used to treat infections caused by microorganisms, including fungi and protozoa. (Gr. anti, "against"; bios, "life") An antibiotic is a chemical substance produced by one organism that is destructive to another. The word antibiotic came from the word antibiosis a term coined in 1889 by Louis Pasteur's pupil Paul Vuillemin which means a process by which life could be used to destroy life. With advances in medicinal chemistry, most antibiotics are now semi synthetic—modified chemically from original compounds found in nature,[1] as is the case with beta-lactams (which include the penicillins, produced by fungi in the genus Penicillium, the cephalosporins, and the carbapenems). Some antibiotics are still produced and isolated from living organisms, such as the aminoglycosides, and others have been created through purely synthetic means: the sulfonamides, the quinolones, and the oxazolidinones. In addition to this origin-based classification into natural, semi synthetic, and synthetic, antibiotics may be divided into two broad groups according to their effect on microorganisms: those that kill bacteria are bactericidal agents, while those that only impair bacterial growth are known as bacteriostatic agents.
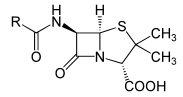 Penicillin, the first natural antibiotic discovered by Alexander Fleming in 1928. Many cures for infectious diseases prior to the beginning of the twentieth century were based on medicinal folklore. Cures for infection in ancient Chinese medicine using plants with antibiotic-like properties began to be described over 2,500 years ago.[2][3] Many other ancient cultures, including the ancient Egyptians, ancient Greeks and medieval Arabs already used molds and plants to treat infections.[4][5]
Penicillin, the first natural antibiotic discovered by Alexander Fleming in 1928. Many cures for infectious diseases prior to the beginning of the twentieth century were based on medicinal folklore. Cures for infection in ancient Chinese medicine using plants with antibiotic-like properties began to be described over 2,500 years ago.[2][3] Many other ancient cultures, including the ancient Egyptians, ancient Greeks and medieval Arabs already used molds and plants to treat infections.[4][5]
The emergence of antibiotic resistance is an evolutionary process that is based on selection for organisms that have enhanced ability to survive doses of antibiotics that would have previously been lethal.[6] Antibiotics like Penicillin and Erythromycin which used to be one-time miracle cures are now less effective because bacteria have become more resistant.[7] Antibiotics themselves act as a selective pressure which allows the growth of resistant bacteria within a population and inhibits susceptible bacteria.[8] Antibiotic selection of pre-existing antibiotic resistant mutants within bacterial populations was demonstrated in 1943 by the Luria-Delbrück experiment.[9] Survival of bacteria often results from an inheritable resistance.[10] Any antibiotic resistance may impose a biological cost and the spread of antibiotic resistant bacteria may be hampered by the reduced fitness associated with the resistance which proves disadvantageous for survival of the bacteria when antibiotic is not present. Additional mutations, however, may compensate for this fitness cost and aids the survival of these bacteria.[11]
Diseases caused by microbial infection:
Fungal diseases cause minor skin diseases. Fungi can also infect deeper tissue and cause septicemia, which are infections of the blood that enable the disease to spread throughout the body. Some fungi live on humans and only cause disease in people with poor immune systems. Fungi exist in two forms: molds and yeasts. Yeasts are commonly found in the vaginal area of the body and work in conjunction with the immune system to fight bacterial infections. Systemic infections from fungi are serious diseases, especially if septicemia develops. Spores inhaled from mold cause respiratory illnesses. Severe allergic reactions from spores inhaled lead to inflammatory responses from the immune system, making it difficult for the patient to breathe. In immunocompetent persons, candidiasis is usually a very localized infection of the skin or mucosal membranes, including the oral cavity (thrush), the pharynx or esophagus, the gastrointestinal tract, the urinary bladder, or the genitalia (vagina, penis).Candidiasis is a very common cause of vaginal irritation, or vaginitis, and can also occur on the male genitals. In immunocompromised patients, Candida infections can affect the esophagus with the potential of becoming systemic, causing a much more serious condition, a fungemia Called candidemia. Light micrograph shows a section of a human lung tisse (blue) embedded with Aspergillus (dark brown). Aspergillosis is caused by the inhalation of fungal spores, which are usually present in the air. In healthy people, the immune system destroys the spores before they cause any harm. In those with a weakened immune system, however, the infection is potentially fatal.[38]
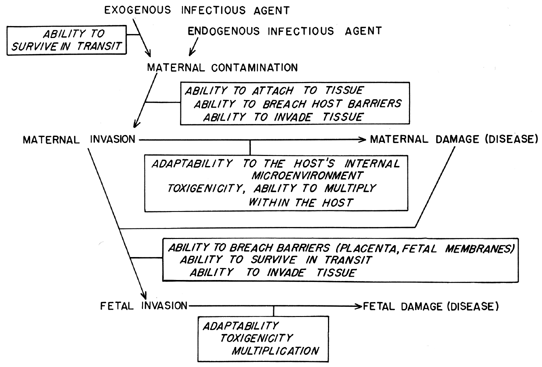
Fig. 1. Overview of infectious disease in pregnancy.
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org
Subscribe to Pharmatutor Job Alerts by Email
Fungal and Bacterial infection in humans and plants