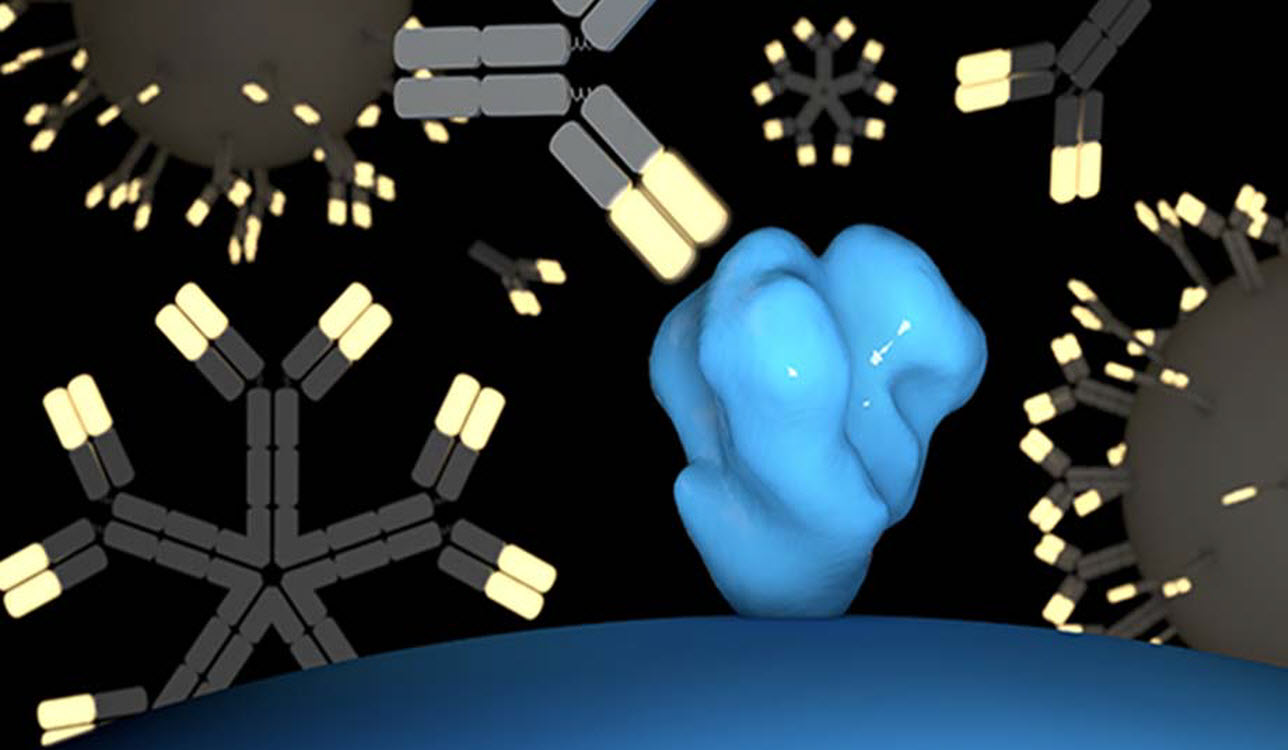
Antibodies from engineered B cells approach an HIV particle (shown in blue) to disable it. In a new study, scientists found that gene-edited B cells can generate durable protective antibody responses against HIV when activated with a vaccine. (Illustration courtesy of the Voss laboratory at Scripps Research.)
Unlike so many other deadly viruses, HIV still lacks a vaccine. The virus—which continues to infect millions around the world—has proven especially tricky to prevent with conventional antibodies, in part because it evolves so rapidly in the body. Any solution would require coaxing the body into producing a special type of antibody that can act broadly to defeat multiple strains of the virus at once.
This week, scientists at Scripps Research moved closer to attaining that holy grail of HIV research with a new vaccine approach that would rely on genetically engineered immune cells from the patient’s body.
In experiments involving mice, the approach successfully induced broadly neutralizing antibodies—also called bnabs—that can prevent HIV infection, says principal investigator James Voss, PhD, of Scripps Research. The study appears in Nature Communications.
Voss and his team showed in 2019 that it was possible to reprogram the antibody genes of the immune system’s B cells using CRISPR so the cells would produce the same broadly neutralizing HIV antibodies that have been found in rare HIV patients.
The new study shows that such engineered B cells, after being reintroduced to the body, can multiply in response to a vaccination—and mature into memory cells and plasma cells that produce high levels of protective antibodies for long periods of time in the body. The team also demonstrated that the engineered genes can be improved to make antibodies that are even more effective against the virus, using a process that normally occurs in B cells that are responding to immunization.
“This is the first time it has been shown that modified B cells can create a durable engineered antibody response in a relevant animal model,” Voss explains.
He hopes that his vaccine approach may someday prevent new HIV infections and possibly offer a functional cure to those who already have HIV/AIDS. The virus is still prevalent throughout the world, with an estimated 38 million people with the disease in 2019.
Voss notes that in humans, the starting cells to create the vaccine could be obtained easily from a simple blood draw, then engineered in the lab before being reintroduced to the patient. He and his team—including first author Deli Huang, PhD, Jenny Tran, PhD, Alex Olson, PhD, and graduate student Mary Tenuta—are now exploring ways to improve the technology so that it would be accessible to the greatest number of people. Because the approach relies on delivering genes to a patient’s own immune cells, this could be a significant challenge.
“People think of cell therapies as being very expensive,” Voss says. “We’re doing a lot of work towards trying to make the technology affordable as a preventative HIV vaccine or functional cure that would replace daily antiviral therapy.”
The study, “Vaccine elicitation of HIV broadly neutralizing antibodies from engineered B cells,” was authored by Deli Huang, Jenny Tuyet Tran, Alex Olson, Thomas Vollbrecht, Mary Tenuta, Mariia Guryleva, Roberta Fuller, Torben Schiffner, Justin Abadejos, Lauren Couvrette, Tanya Blane, Karen Saye, Wenjuan Li, Elise Landais, Alicia Gonzalez-Martin, William Schief, Ben Murrell, Dennis Burton, David Nemazee and James Voss.













