 About Authors:
About Authors:
Sachin Saxena*1,Pankaj Sharma1 ,Nimisha2
1-M Pharm (Pharmaceutics) , Amity Univerity,Lucknow
2-Lecturer,
Amity University,
Lucknow
Abstract:
Rapid developments in the field of molecular biology and gene technology resulted in generation of many macromolecular drugs including peptides, proteins, polysaccharides and nucleic acids in great number possessing superior pharmacological efficacy with site specificity and devoid of unwanted and toxic effects. However, the main impediment for the oral delivery of these drugs as potential therapeutic agents is their extensive presystemic metabolism, instability in acidic environment resulting into inadequate and erratic oral absorption. Parentral route of administration is the only established route that overcomes all these drawbacks associated with these orally less/inefficient drugs but, these formulations are costly, have least patient compliance, require repeated administration, in addition to the other hazardous effects associated with this route. Buccal drug delivery leads direct access to the systemic circulation through the internal jugular vein bypasses drugs from the hepatic first pass metabolism leading to high bioavailability. Buccal route is an attractive route of administration for systemic drug delivery. Buccal bioadhesive films, releasing topical drugs in the oral cavity at a slow and predetermined rate, provide distinct advantages over traditional dosage forms for treatment of many diseases.
[adsense:336x280:8701650588]
Reference ID: PHARMATUTOR-ART-1207
INTRODUCTION
Amongst the various routes of drug delivery, oral route is perhaps the most preferred to the patient and the clinician alike. However, peroral administration of drugs has disadvantages such as hepatic first pass metabolism and enzymatic degradation within the GI tract, that prohibit oral administration of certain classes of drugs especially peptides and proteins. Consequently, other absorptive mucosae are considered as potential sites for drug administration. Transmucosal routes of drug delivery (i.e., the mucosal linings of the nasal, rectal, vaginal, ocular, and oral cavity) offer distinct advantages over peroral administration for systemic drug delivery. These advantages include possible bypass of first pass effect, avoidance of presystemic elimination within the GI tract, and, depending on the particular drug, a better enzymatic flora for drug absorption.
Amongst the various routes of administration tried so far in the novel drug delivery systems, localized drug delivery to tissues of the oral cavity has been investigated for the treatment of periodontal disease, bacterial and fungal infection. Over the decades mucoadhesion has become popular for its potential to optimize localized drug delivery, by retaining a dosage form at the site of action (e.g. within the gastrointestinal tract) or systemic delivery by retaining the formulation in intimate contact with the absorption site (e.g. buccal cavity). Well defined bioadhesion is the ability of a material (synthetic or biological) to adhere to a biological tissue for an extended period of time. The biological surface can be epithelial tissue or it can be the mucus coat on the surface of a tissue. If adhesion is to a mucous coat, the phenomenon is referred to as mucoadhesion.
The use of mucoadhesive polymers in buccal drug delivery has a greater application. Various mucoadhesive devices, including tablets, films, patches, disks, strips, ointments and gels, have recently been developed. However, buccal patch offer greater flexibility and comfort than the other devices. In addition, a patch can circumvent the problem of the relatively short residence time of oral gels on mucosa, since the gels are easily washed away by saliva.
Buccal route of drug delivery provides the direct access to the systemic circulation through the jugular vein bypassing the first pass hepatic metabolism leading to high bioavailability. Other advantages such as excellent accessibility, low enzymatic activity, suitability for drugs or excipients that mildly and reversibly damage or irritate the mucosa, painless administration, easy withdrawal, facility to include permeation enhancer/ enzyme inhibitor or pH modifier in the formulation, versatility in designing as multidirectional or unidirectionalrelease system for local or systemic action
ADVANTAGES OF BUCCAL PATCHES-
1. The oral mucosa has a rich blood supply. Drugs are absorbed from the oral cavity through the oral mucosa, and transported through the deep lingual or facial vein, internal jugular vein and braciocephalic vein into the systemic circulation.
2. Buccal administration, the drug gains direct entry into the systemic circulation thereby bypassing the first pass effect. Contact with the digestive fluids of gastrointestinal tract is avoided which might be unsuitable for stability of many drugs like insulin or other proteins, peptides and steroids. In addition, the rate of drug absorption is not influenced by food or gastric emptying rate.
3. The area of buccal membrane is sufficiently large to allow a delivery system to be placed at different occasions, additionally; there are two areas of buccal membranes per mouth, which would allow buccal drug delivery systems to be placed, alternatively on the left and right buccal membranes.
4. Buccal patch has been well known for its good accessibility to the membranes that line the oral cavity, which makes application painless and with comfort.
5. Patients can control the period of administration or terminate delivery in case of emergencies. The buccal drug delivery systems easily administered into the buccal cavity. The novel buccal dosage forms exhibits better patient compliance.
Novel buccal dosage forms
The novel type buccal dosage forms include buccal adhesive tablets, patches, films, semisolids (ointments and gels) and powders.
A. Buccal mucoadhesive tablets
Buccal mucoadhesive tablets are dry dosage forms that have to be moistened prior to placing in contact with buccal mucosa. Example: a double layer tablet, consisting of adhesive matrix layer of hydroxy propyl cellulose and polyacrylic acid with an inner core of cocoa butter containing insulin and a penetration enhancer (sodium glycocholate).
B. Patches and Films
Buccal patches consists of two laminates, with an aqueous solution of the adhesive polymer being cast onto an impermeable backing sheet, which is then cut into the required oval shape. A novel mucosal adhesive film called “Zilactin” – consisting of an alcoholic solution of hydroxy propyl cellulose and three organic acids. The film which is applied to the oral mucosal can be retained in place for at least 12 hours even when it is challenged with fluids.
C. Semisolid Preparations (Ointments and Gels)
Bioadhesive gels or ointments have less patient acceptability than solid bioadhesive dosage forms, and most of the dosage forms are used only for localized drug therapy within the oral cavity. One of the original oral mucoadhesive delivery systems –“orabase”– consists of finely ground pectin, gelatin and sodium carboxy methyl cellulose dispersed in a poly (ethylene) and a mineral oil gel base, which can be maintained at its site of application for 15-150 minutes.
D. Powders
Hydroxpropyl cellulose and beclomethasone in powder form when sprayed onto the oral mucosa of rats, a significant increase in the residence time relative to an oral solution is seen, and 2.5% of beclomethasone is retained on buccal mucosa for over 4 hours.
BUCCAL DRUG DELIVERY SYSTEM
A delivery system designed to deliver drugs systemically or locally via buccal mucosa. Buccal delivery refers to the drug release which can occur when a dosage form is placed in the outer vestibule between the buccal mucosa and gingival.
MECHANISM OF BUCCAL ABSORPTION-
Buccal drug absorption occurs by passive diffusion of the nonionized species, a process governed primarily by a concentration gradient, through the intercellular spaces of the epithelium. The passive transport of non-ionic species across the lipid membrane of the buccal cavity is the primary transport mechanism. The buccal mucosa has been said to be a lipoidal barrier to the passage of drugs, as is the case with many other mucosal membrane and the more lipophilic the drug molecule, the more readily it is absorbed[4]. The dynamics of buccal absorption of drugs could be adequately described by first order rate process. Several potential barriers to buccal drug absorption have been identified. Dearden and Tomlison (1971) pointed out that salivary secretion alters the buccal absorption kinetics from drug solution by changing the concentration of drug in the mouth. The linear relationship between salivary secretion and time is given as follows:
Where,
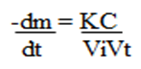
M - Mass of drug in mouth at time t
K - Proportionality constant
C - Concentration of drug in mouth at time
Vi - The volume of solution put into mouth cavity and Vt - Salivary secretion rate
FACTORS AFFECTING BUCCAL ABSORPTION
The oral cavity is a complex environment for drug delivery as there are many interdependent and independent factors which reduce the absorbable concentration at the site of absorption.
1.Membrane Factors
This involves degree of keratinization, surface area available for absorption, mucus layer of salivary pellicle, intercellular lipids of epithelium, basement membrane and lamina propria. In addition, the absorptive membrane thickness, blood supply/ lymph drainage, cell renewal and enzyme content will all contribute to reducing the rate and amount of drug entering the systemic circulation.
2. Environmental Factors
A. Saliva: The thin film of saliva coats throughout the lining of buccal mucosa and is called salivary pellicle or film. The thickness of salivary film is 0.07 to 0.10 mm. The thickness, composition and movement of this film affect the rate of buccal absorption.
B. Salivary glands: The minor salivary glands are located in epithelial or deep epithelial region of buccal mucosa. They constantly secrete mucus on surface of buccal mucosa. Although, mucus helps to retain mucoadhesive dosage forms, it is potential barrier to drug penetration.
C. Movement of buccal tissues: Buccal region of oral cavity shows less active movements. The mucoadhesive polymers are to be incorporated to keep dosage form at buccal region for long periods to withstand tissue movements during talking and if possible during eating food or swallowing.
COMPOSITION OF BUCCAL PATCHES
A. Active ingredient.
B. Polymers (adhesive layer): Hydroxy ethylcellulose, hydroxypropyl cellulose, polyvinyl pyrrolidone, polyvinyl alcohol, carbopol and other mucoadhesive polymers.
C. Diluents: Lactose DC is selected as diluent for its high aqueous solubility, its flavouring characteristics, and its physico-mechanical properties, which make it suitable for direct compression. other example : microcrystalline starch and starch.
D. Sweetening agents: Sucralose, aspartame, mannitol, etc. E. Flavouring agents: Menthol, vanillin, clove oil, etc.
F. Backing layer: Ethyl cellulose, etc.
G. Penetration enhancer: Cyano acrylate, etc.
H. Plasticizers: PEG-100, 400, propylene glycol, etc.
METHOD OF PREPARATION
Two methods are used to prepare adhesive patches.
1. Solvent casting
In this method, all patch excipients including the drug co-dispersed in an organic solvent and coated onto a sheet of release liner. After solvent evaporation a thin layer of the protective backing material is laminated onto the sheet of coated release liner to form a laminate that is die-cut to form patches of the desired size and geometry.
2. Direct milling
In this, patches are manufactured without the use of solvents. Drug and excipients are mechanically mixed by direct milling or by kneading, usually without the presence of any liquids. After the mixing process, the resultant material is rolled on a release liner until the desired thickness is achieved. The backing material is then laminated as previously described. While there are only minor or even no differences in patch performance between patches fabricated by the two processes, the solvent-free process is preferred because there is no possibility of residual solvents and no associated solvent-related health issues.
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
EVALUATIONS OF BUCCAL PATCH
1. Surface pH
Buccal patches are left to swell for 2 hr on the surface of an agar plate. The surface pH is measured by means of a pH paper placed on the surface of the swollen patch
2. Thickness measurements
The thickness of each film is measured at five different locations (centre and four corners) using an electronic digital micrometer
3. Swelling study
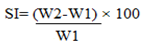
Buccal patches are weighed individually (designated as W1), and placed separately in 2% agar gel plates, incubated at 37°C ± 1°C, and examined for any physical changes. At regular 1-hour time intervals until 3 hours, patches are removed from the gel plates and excess surface water is removed carefully using the filter paper [11]. The swollen patches are then reweighed (W2) and the swelling index (SI) is calculated using the following formula.
4.Thermal analysis study
Thermal analysis study is performed using differential scanning calorimeter (DSC).
5. Morphological characterization
Morphological characters are studied by using scanning electron microscope (SEM).
6. Water absorption capacity test
Circular Patches, with a surface area of 2.3 cm2 are allowed to swell on the surface of agar plates prepared in simulated saliva (2.38 g Na2HPO4, 0.19 gKH2PO4, and 8 g NaCl per litter of distilled water adjusted with phosphoric acid to pH 6.7), and kept in an incubator maintained at 37°C ± 0.5°C. At various time intervals (0.25, 0.5, 1, 2, 3, and 4 hours), samples are weighed (wet weight) and then left to dry for 7 days in a desiccator over anhydrous calcium chloride at room temperature then the final constant weights are recorded. Water uptake (%) is calculated using the following equation
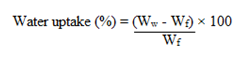
Where, Ww is the wet weight and Wf is the final weight. The swelling of each film is measured
7. Ex-vivo bioadhesion test
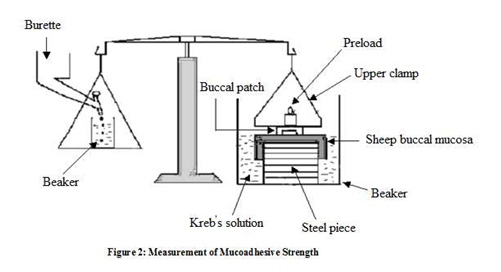
The fresh sheep mouth separated and washed with phosphate buffer (pH 6.8). A piece of gingival mucosa is tied in the open mouth of a glass vial, filled with phosphate buffer (pH 6.8). This glass vial is tightly fitted into a glass beaker filled with phosphate buffer (pH 6.8, 37°C ± 1°C) so it just touched the mucosal surface. The patch is stuck to the lower side of a rubber stopper with cyano acrylate adhesive. Two pans of the balance are balanced with a 5-g weight. The 5-g weight is removed from the left hand side pan, which loaded the pan attached with the patch over the mucosa. The balance is kept in this position for 5 minutes of contact time. The water is added slowly at 100 drops/min to the right-hand side pan until the patch detached from the mucosal surface. The weight, in grams, required to detach the patch from the mucosal surface provided the measure of mucoadhesive strength (Figure 2).
8. In vitro drug release
The United States Pharmacopeia (USP) XXIII-B rotating paddle method is used to study the drug release from the bilayered and multilayered patches. The dissolution medium consisted of phosphate buffer pH 6.8. The release is performed at 37°C ± 0.5°C, with a rotation speed of 50 rpm. The backing layer of buccal patch is attached to the glass disk with instant adhesive material. The disk is allocated to the bottom of the dissolution vessel. Samples (5 ml) are withdrawn at predetermined time intervals and replaced with fresh medium. The samples filtered through whatman filter paper and analyzed for drug content after appropriate dilution. The in- vitro buccal permeation through the buccal mucosa (sheep and rabbit) is performed using Keshary-Chien/Franz type glass diffusion cell at 37°C± 0.2°C. Fresh buccal mucosa is mounted between the donor and receptor compartments. The buccal patch is placed with the core facing the mucosa and the compartments clamped together. The donor compartment is filled with buffer (Figure 3).
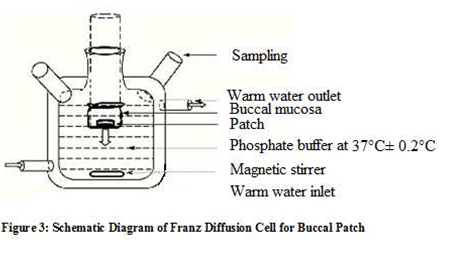
9. Permeation study of buccal patch
The receptor compartment is filled with phosphate buffer pH 6.8, and the hydrodynamics in the receptor compartment is maintained by stirring with a magnetic bead at 50 rpm. Samples are withdrawn at predetermined time intervals and analyzed for drug content
10. Ex-vivo mucoadhesion time
The ex-vivo mucoadhesion time performed after application of the buccal patch on freshly cut buccal mucosa (sheep and rabbit). The fresh buccal mucosa is tied on the glass slide, and a mucoadhesive patch is wetted with 1 drop of phosphate buffer pH 6.8 and pasted to the buccal mucosa by applying a light force with a fingertip for 30 seconds. The glass slide is then put in the beaker, which is filled with 200 ml of the phosphate buffer pH 6.8, is kept at 37°C ± 1°C. After 2 minutes, a 50-rpm stirring rate is applied to simulate the buccal cavity environment, and patch adhesion is monitored for 12 hours. The time for changes in colour, shape, collapsing of the patch, and drug content is noted.
11. Measurement of mechanical properties
Mechanical properties of the films (patches) include tensile strength and elongation at break is evaluated using a tensile tester. Film strip with the dimensions of 60 x 10 mm and without any visual defects cut and positioned between two clamps separated by a distance of 3 cm. Clamps designed to secure the patch without crushing it during the test, the lower clamp held stationary and the strips are pulled apart by the upper clamp moving at a rate of 2 mm/sec until the strip break. The force and elongation of the film at the point when the trip break is recorded. The tensile strength and elongation at break values are calculated using the formula.
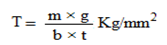
Where,
M - is the mass in gm, g - is the acceleration due to gravity 980 cm/sec 2
B - is the breadth of the specimen in cm
T - is the thickness of specimen in cm.
Tensile strength (kg/mm2) is the force at break (kg) per initial cross- sectional area of the specimen (mm2).
12. Stability study in human saliva
The stability study of optimized bilayered and multilayered patches is performed in human saliva. The human saliva is collected from humans (age 18-50years). Buccal patches are placed in separate petridishes containing 5ml of human saliva and placed in a temperature-controlled oven at 37°C ± 0.2°C for 6 hours. At regular time intervals (0, 1, 2, 3, and 6 hours), the dose formulations with better bioavailability are needed. Improved methods of drug release through transmucosal and transdermal methods would be of great significance, as by such routes, the pain factor associated with parenteral routes of drug administration can be totally eliminated. Buccal adhesive systems offer innumerable advantages in terms of accessibility, administration and withdrawal, retentively, low enzymatic activity, economy and high patient compliance. Adhesion of buccal adhesive drug delivery devices to mucosal membranes leads to an increased drug concentration gradient at the absorption site and therefore improved bioavailability of systemically delivered drugs. In addition, buccal adhesive dosage forms have been used to target local disorders at the mucosal surface (e.g., mouth ulcers) to reduce the overall dose required and minimize side effects that may be due to systemic administration of drugs. Researchers are now looking beyond traditional polymer networks to find other innovative drug transport systems. Currently solid dosage forms, liquids and gels applied to oral cavity are commercially successful. The future direction of buccal adhesive drug delivery lies in vaccine formulations and delivery of small proteins/peptides.
CONCLUSION
The buccal mucosa offers several advantages for controlled drug delivery for extended periods of time. The mucosa is well supplied with both vascular and lymphatic drainage and first-pass metabolism in the liver and pre-systemic elimination in the gastrointestinal tract are avoided. The area is well suited for a retentive device and appears to be acceptable to the patient. With the right dosage form design and formulation, the permeability and the local environment of the mucosa can be controlled and manipulated in order to accommodate drug permeation. Buccal drug delivery is a promising area for continued research with the aim of systemic delivery of orally inefficient drugs as well as a feasible and attractive alternative for non-invasive delivery of potent peptide and protein drug molecules. However, the need for safe and effective buccal permeation/absorption enhancers is a crucial component for a prospective future in the area of buccal drug delivery.
REFERENCES
1. Giradkar KP, et al, Design development and in vitro evaluation of bioadhesive dosage form for buccal route, International journal of pharma research & development, 2010, 2.
2. Shidhaye SS, et al, Mucoadhesive bilayered patches for administration of sumatriptan, AAPS pharm sci tech, 2009, 9(3).
3. Amir H, et al, Systemic drug delivery via the buccal mucosal route, Pharmaceutical technology, 2001, 1-27.
4. Pramodkumar TM et al, Oral transmucosal drug delivery systems, Indian drug, 2004, 41(2), 63-12.
5. Edsman K, et al, Pharmaceutical applications of mucoadhesion for the non-oral routes, Journal of pharmacy & pharmacology, 2005, 57, 3-19.
6. Steward A et al, The Effect of Enhancers on the Buccal Absorption of Hybrid (BDBB) Alpha-Interferon, Int.J. Pharm, 104, 1994, 145–149.
7. Aungst BJ and Rogers NJ, Site Dependence of Absorption- Promoting Actions of Laureth9, Na Salicylate, Na2EDTA, and Aprotinin on Rectal, Nasal, and Buccal Insulin Delivery, Pharm. Res, 1988, 5 (5), 305–308
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE









