 About Authors:
About Authors:
Kritika Rastogi, U.K. Singh, A.K. Chaturvedi
Kharvel Subharti College of Pharmacy, (swami vivekanand subharti university) subhartipuram,
N.H-58, Meerut By Pass Road, Meerut, Uttar pradesh-250001,India.
*kritikarastogi6@gmail.com
Abstract
Insulin remains the most effective and durable hypoglycemic agent for the treatment of diabetes. Insulin is a major protein hormone secreted by beta –cells of the pancreas and is important for the control of diabetes. Insulin has an important place in drug therapies for insulin dependent diabetes mellitus (type I) and for many patients with non-insulin-dependent diabetes mellitus (type II). It would be highly advantageous if insulin could be administered orally, because the oral delivery of insulin can mimic the physiological fate of insulin and may provide better glucose homeostasis. The desire to deliver protein and peptide biopharmaceuticals conveniently and effectively has led to the intense investigation of targeted delivery systems. The goal of oral insulin delivery devices is to protect the sensitive drug from proteolytic degradation in the stomach and upper portion of the small intestine.
[adsense:336x280:8701650588]
Reference Id: PHARMATUTOR-ART-1710
Introduction
Insulin is a hormone with intensive effects on both metabolism and several other body systems (eg; vascular compliance). Insulin causes most of the body's cells to take up glucose from the blood (including liver, muscle and fat tissue cells), storing it as glycogen in the liver and muscle and stops use of fat as an energy source. When insulin is absent (or low), glucose is not taken up by most body cells and the body begins to use fat as an energy source (i.e. transfer of lipids from adipose tissue to the liver for mobilization as an energy source). As its level is a central metabolic control mechanism, its status is also used as a control signal to other body systems (such as amino acid uptake by body cells). It has several other anabolic effects throughout the body. When control of insulin levels fails, diabetes mellitus results.(1,2)
Insulin is used medically to treat some forms of diabetes mellitus. Patients with Type 1 diabetes mellitus depend on external insulin (most commonly injected subcutaneously) for their survival because the hormone is no longer produced internally. Patients with Type 2 diabetes mellitus are insulin resistant, have relatively low insulin production, or both; some patients with Type 2diabetes may eventually require insulin when other medications fail to control blood glucose levels adequately.
Diabetes develops due to a diminished production of insulin (in type 1) or resistance to its effects (in type 2 and gestational). Both lead to hyperglycemia, which largely causes the acute signs of diabetes: excessive urine production, resulting compensatory thirst and increased fluid intake, blurred vision, unexplained weight loss, lethargy and changes in energy metabolism. Monogenic forms, e.g. MODY, constitute 1-5 % of all cases. Diabetes affects a large percentage of population around the world and has assumed epidemic dimensions.The current estimate of the number of diabetic patients in the world is 171.2 million (2.8%) in the year 2000 and predicted to be 366.2 million (4.4%) by the year 2030.
Type 2 diabetes is the main type of diabetes mellitus rather typeI diabetic occurs 5-10% only. The patients requiring insulin may have to take more than 60,000 injections throughout their life. Compliance is currently a major drawback in current diabetes delivery devices, with several patients suffering from Type 2 diabetes irregularly following or, in some cases, even discontinuing their insulin therapy due to pain or fear of injections.
Through more convenient drug delivery methods, pharmaceutical companies, regulatory bodies and other government institutions can introduce better diabetes care and reduce costs related to diabetic complications caused by “poor compliance."
At present, several methods of non-invasive insulin delivery, including oral, transdermal, nanotechnology based and gene therapy-based ones, are under research. Efforts are also on to develop a diabetes vaccine. One of the most promising modes of delivery under investigation is that of inhaled insulin .(3)
[adsense:468x15:2204050025]
Structure of Insulin
Like most of the other hormones, insulin is a protein comprising of 2 polypeptide chains A (with 21 amino acid residues) and B (with 30 amino acid residues) [Fig. 1]. Chains A and B are linked by disulphide bridges. In addition A-chain contains an intra-chain disulphide bridge linking residue 6 and 11. The structure of insulin is shown in the fi gure 1 below. C-chain, which connects A and B chains is liberated along with insulin after breakdown of proinsulin.
Insulin monomers aggregate to form dimers and hexamers .(4)
Zn hexamer is composed of three insulin dimmers associated in threefold symmetrical pattern.

Fig.1 structure of insulin
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
Insulin secretion
Insulin is secreted from the beta cells in response to various stimuli like glucose, arginine, sulphonylureas though physiologically glucose is the major determinant.Various neural, endocrine and pharmacological agents can also exert stimulatory effect. Glucose is taken up by beta cells through GLUT-2 receptors.
After entering the beta cell, glucose is oxidized by glucokinase, which acts as a glucose sensor. Glucose concentration below 90 mg/dl do not cause any insulin release. At such substimulatory glucose concentrations, K+ efflux through open KATP channels keeps the ß cell membrane at a negative potential at which voltage-gated Ca2+ channels are closed. As there is increase in plasma glucose, glucose uptake and metabolism by the ß cell is enhanced.
Rise in ATP concentration result in closure of KATP channels, leading to a membrane depolarization, opening of voltage-gated Ca2+ channels, Ca2+ influx, a rise in intracellular calcium concentration, and ultimately exocytosis of insulin granules.
Structurally, the pancreatic KATP channel consists of two unrelated subunits: a sulfonylurea receptor (the SUR1 isoform) and a potassium channel subunit (Kir6.2) that forms the central ion-conducting pathway (Fig 2).

Fig.2 secretion of insulin
The mature KATP channel exists as an octamer of Kir6.2 and SUR1 subunits in a 4:4 stoichiometry (Fig 2). A subunit specific site specific to pancreatic KATP channel, confers glimepiride an advantage over the other sulfonylurea secretagogues(5).
Sulfonylurea, and non-sulphonylurea drugs act as insulin secretogogues by closing KATP channels bypassing the ß cell metabolism. Diazoxide is a K channel opener and inhibits insulin secretion, independent of blood glucose levels(6).
Challenges to oral insulin delivery
Generally, peptides and proteins such as insulin cannot be administered via the oral route due to rapid enzymatic degradation in the stomach, inactivation and digestion by proteolytic enzymes in the intestinal lumen, and poor permeability across intestinal epithelium because of its high molecular weight and of lipophilicity(7,8,9) .
The oral bioavailability of most peptides and proteins therefore is less than 1%. The challenge here is to improve the bioavailability to anywhere between 30 – 50% (10).
* Enzymatic barrier
The harsh environment of the gastrointestinal tract (GIT) causes insulin to undergo degradation. This is because digestive processes are designed to breakdown proteins and peptides without any discrimination(11). Insulin therefore undergoes enzymatic degradation by pepsin and pancreatic proteolytic enzymes such as trypsin and a-chymotrypsin (12,13).
Overall, insulin is subjected to acid- catalyzed degradation in the stomach, luminal degradation in the intestine and intracellular degradation. The cytosolic enzyme that degrades insulin is insulin-degrading enzyme (IDE) (14).Insulin is however not subject to proteolytic breakdown by brush border enzymes (15). Insulin can be presented for absorption only if the enzyme attack is either reduced or defeated.
* Intestinal transport of insulin
Another major barrier to the absorption of hydrophilic macromolecules like insulin is that they cannot diffuse across epithelial cells through lipid- bilayer cell membranes to the blood stream(16). In other words, insulin has low permeability through the intestinal mucosa(17). There is no evidence of active transport for insulin(18).
It has been found however that insulin delivery to the mid- jejunum protects insulin from gastric and pancreatic enzymes and release from the dosage form is enhanced by intestinal microflora(18,19).
Various strategies have been tried out to enhance the absorption of insulin in the intestinal mucosa and in some cases; they have proven successful in overcoming this barrier.
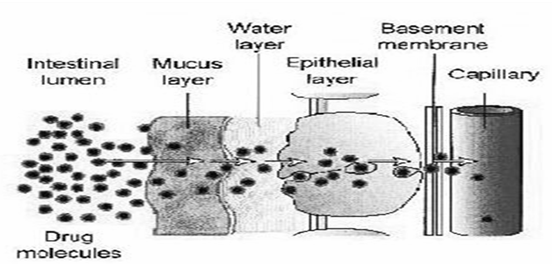
Fig-3 Barriers to absorption of drug in the intestine
* Dosage form Stability
The activity of proteins depends on the three- dimensional molecular structure. During dosage form development, proteins might be subject to physical and chemical degradation. Physical degradation involves modification of the native structure to a higher order structure while chemical degradation involving bond cleavage results in the formation of a new product .
Proteins must be characterized for change in conformation, size, shape, surface properties, and bioactivity upon formulation processing. Changes in conformation, size, shape can be observed by use of spectrophotometric techniques, X-ray diffraction, differential scanning calorimetery, light scattering, electrophoresis, and gel filtration (20).
The need for oral insulin
Resistance to injectable insulin has been identified as a major reason for clinical inertia and lack of achievement of target glycemic goals. Physicians as well as patients fear the complexity of insulin regimes, the risk of hypoglycemia, and the chances of weight gain, as well as the necessity of a needle prick, with insulin therapy.
Insulin is perceived to have a high index of intrusion as the conventional insulins need to be given prior to meals (21). Patients anticipate the early development of an oral insulin, as it will be easy to administer, have a lower index of intrusion, be more convenient, and have more compliance or adherence from the patient, and finally lead to better glycemic control, and thus, prevention of complications of diabetes (22).
Oral insulin may improve b-cell function by providing b-cell rest (23), and may help in preventing diabetes via induction of ‘oral tolerance’ or immuno modulation (24, 25). Oral insulin is able to achieve a high porto-systemic gradient, as it is delivered to the liver from the gastrointestinal tract. This reduces systemic insulin exposure and may obviate the excessive weight gain sometimes seen with subcutaneous insulin. Oral insulin may also be able to correct the blunting of first-phase release of insulin (26), which is difficult with conventional subcutaneous insulins.
Potential problems with oral insulin
While oral insulin may have physiological advantages, it may raise problems inherent to oral medication in general. For instance, the rate and extent of absorption of an oral drug are often affected by food and may differ if the drug is administered shortly before a meal or after a meal (fed conditions) as compared to administration under fasting conditions.
The optimal timing for oral insulin ingestion depends at least in part on the technology used for drug delivery and will need to be determined for each oral insulin in development. The food effect is likely to determine how the oral insulin will be used and for what indication.
One other issue is that all the polypeptide and protein delivery platforms developed thus far have relatively low bioavailability. Low bioavailability is a harbinger of significant inter- and intrasubject variability.
A way to reduce variability is to increase the amount of insulin in the dosage form. Until recently such a proposition was impractical for insulin because of commercial considerations.
At the present time, however, the supply of insulin and its price can support such a strategy. Low bioavailability also implies that most of the insulin ingested is not absorbed and remains in the gastrointestinal tract. It is most likely that insulin retained in the gastrointestinal tract will be degraded by peptidases and proteases.
Nevertheless, a concern that will need to be addressed in long-term safety studies is whether insulin, a known mitogen implicated in an increased risk of several cancers, including colon cancer, will increase the incidence of cancer when given orally.Finally, while insulin per se may not be toxic, the chemical compounds employed in the various delivery systems as excipients or absorption promoters need to be deemed safe and effective in long-term toxicological and clinical studies(27-29).
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
Approaches of oral insulin
A. Attempted Oral Insulin Delivery Systems
Most peptides are not bioavailable from the GIT after oral administration (30). Therefore successful oral insulin delivery involves overcoming the enzymatic and physical barriers and taking steps to conserve bioactivity during formulation processing . In developing oral protein delivery systems with high bioavailability, three practical approaches might be most helpful: (31)
1. Modification of physicochemical properties such as lipophilicity and enzyme susceptiblity.
2. Addition of novel function to macromolecules.
3. Use of improved carrier systems.
The various oral delivery systems which have been attempted to deliver insulin orally either singly or in a synergistic approach can be categorized as follows:
Enzyme Inhibitors
Insulin is degraded in the GIT by pepsin and other proteolytic enzymes. Enzyme inhibitors slow the rate of degradation of insulin which increases the amount of insulin available for absorption.
The earliest studies involving enzyme inhibitors were carried out with sodium cholate along with aprotinin which improved insulin absorption in rats (32).
In one study, polymers cross-linked with azoaromatic groups formed an impervious film to protect insulin from digestion in the stomach and small intestine (33). The use of enzyme inhibitors in long-term therapy however remains questionable because of possible absorption of unwanted proteins, disturbance of digestion of nutritive proteins and stimulation of protease secretion (34).
Penetration Enhancers
Hydrophilic molecules like insulin are adsorbed to the apical membrane and are internalized by endocytosis . Another theory suggests absorption via paracellular transport. Tight junctions between each of the cells in the epithelium prevent water and aqueous soluble compounds from moving past those cells.
Hence, approaches for modulating tight-junction permeability to increase paracellular transport have been studied (35). A number of absorption enhancers are available that cause these tight junctions to open transiently allowing water-soluble proteins to pass.
Absorption may be enhanced when the product is formulated with acceptable safe excipients (36). These include substances like bile salts, surfactants, trisodium citrates, chelating agents like EDTA, labrasol (37).
The drawbacks with penetration enhancers include lack of specificity, i.e., they allow all content of the intestinal tracts including toxins and pathogens the same access to the systemic bloodstream, and risk to mucous membranes by surfactants and damage of cell membrane by chelators . Mucoadhesive polymers have been proven to be safe and efficient intestinal permeation enhancers for the absorption of protein drugs (38).
Chemical modifications
Modifying the chemical structure of a peptide or protein is another approach to enhance bioavailability by increasing its stability against possible enzymatic degradation or its membrane permeation.
However, this approach is more applicable to peptides rather than proteins because of the structural complexity of proteins. For example, substitution of D-amino acids for L-amino acids in the primary structure can improve the enzymatic stability of peptides.
A diacyl derivative of insulin maintains its biological activity and also increases absorption from the intestine (39).
B. Carrier Systems
Hydrogels
These are cross-linked networks of hydrophilic polymers, which are able to absorb large amounts of water and swell, while maintaining their three- dimensional structure .Complexation hydrogels are suitable candidates for oral delivery of proteins and peptides due to their abilities to respond to changes in pH in the GI tract and provide protection to the drugs from the harsh environment of the GI tract (40).
Liposomes
Insulin-entrapped liposomes cause dose-dependent hypoglycemia. Researcher have prepared liposomes with varying composition by two methods: solvent evaporation hydration and solvent spherule evaporation. Liposomes containing lecithin 100 mg, cholesterol 20 mg, insulin150 units, and Tween 1% v/v were found to be most effective.
The effect of insulin-liposome was prolonged in diabetes-induced rabbits than that of normal rabbits. The pharmacodynamics of the insulin-liposome system was comparable with the action of 1 U/kg of insulin administered subcutaneously (41).
Erythrocytes
Human red blood cells have been developed as oral carrier systems for human insulin. In a study by Al- Achi et al., male Wistar rats were made diabetic by a single intraperitoneal injection of streptozocin (100 mg/kg) . Rats received orally one of the following (100 U, 2 mL): an insulin solution, a ghosts-insulin suspension, a vesicles- insulin suspension, a liposomes-ghosts-insulin suspension, or a liposomes-vesicles-insulin suspension.
Free-carrier suspensions or sodium chloride solution (0.9%) were given orally as controls. Blood glucose concentration was determined just before administration and at 1, 2,3,4,5,6, and 7 h post administration. Results showed that all treatment groups, except liposomes-ghosts- insulin, were significantly different statistically from their respective controls (i.e., the free carriers)(42).
Nanospheres
Damge et al. prepared insulin-loaded nanospheres by polymerization of isobutyl cyanoacrylate (IBCA) in an acidic medium. These nanospheres displayed a mean size of 145 nm and an association rate of 1 U of insulin per milligram of polymer.
These nanospheres were dispersed in an oily medium (Miglyol 812) containing surfactant(Polox-amer 188 and deoxycholic acid) and evaluated for in vitro and in vivo degradation. No degradationdue to proteolytic enzyme was observed in vitro. When these nanospheres (100 U per kilogram of body weight) were administered perorally in streptozotocin-induced diabetic rats, a 50% decrease in fasted glucose levels from the second hour up to 10-13 days was observed.
This effect was shorter (2 days) or absent when nanospheres were dispersed in water. Using 14C labeled nanospheres loaded with ( 125I) insulin, it was found that nanospheres increased the uptake of (125I) insulin or its metabolites in the gastrointestinal tract, blood, and liver while the excretion was delayed when compared to (125I) insulin nonassociated to nanospheres (43).
Nanocubicles
A liquid formula that can be easily dispersed in water to produce particles named "Nanocubicles" was developed by Chung et al. These nanocubicles containing insulin were administered to fasted streptozotocininduced diabetic rats.
For comparison, an aqueous solution of insulin in water was also administered. Nanocubicles without insulin and insulin in phosphate buffer saline (PBS) were administered as controls. Blood glucose concentration and insulin concentration were measured 1, 2, 3, 4, and 6 h after the administration of the insulin formulations.
In vitro experiments showed that the particles were taken up by the Caco-2 cells at a high ratio. It was observed in these studies that the serum glucose concentration was controlled for more than 6 h after oral insulin administration but returned to the basal concentration in 3 h when 1 IU/kg of insulin was injected, intravenously (44).
Other Approaches
Tablets
Thiolated chitosan insulin tablets:
The efficacy of orally administered insulin has also been improved using thiolated chitosan. 2-Iminothiolane was covalently linked to chitosan and the resulting chitosan-TBA (chitosan-4-thiobutylamidine) conjugate exhibited 453.5 ± 64.1 µmol thiol groups per gram of polymer (A.H. Krauland et al., 2004).
Two enzyme inhibitors Bowman-Birk-Inhibitor (BBI) and Elastatinal were covalently linked to chitosan. Chitosan-TBA conjugate (5 mg), insulin (2.75 mg), the permeation mediator reducer glutathione (0.75 mg), and the two inhibitor conjugates (in each case 0.75 mg) were compressed to make chitosan-TBA-insulin tablets. Control tablets were also prepared using chitosan and insulin. Chitosan-TBA-insulin tablets showed a controlled release of insulin over 8 h.
In vitro mucoadhesion studies showed that the mucoadhesive/cohesive properties of chitosan were at least 60-fold improved by the immobilization of thiol groups on the polymer.
Microemulsions
water-in-oil microemulsions in which the aqueous phase is insulin and oil phase is lecithin, non- esterified fatty acids and cholesterol in critical proportions.
In vivo studies showed substantial reduction in blood glucose. Recent studies have focused on enteric-coated dry emulsion formulations prepared from solid-in-oil-in-water emulsions. These responded to changes in external environment suggesting potential application for oral insulin delivery.
Oral insulin pills
Insulin administration in the form of a pill has always been an attractive concept in research. Due to numerous limitations of this mode of insulin administration, efficacy has been hard to administration, efficacy has been hard to demonstrate. Research has focused on overcoming
these limitations by stabilising the degradation, improving the permeability, and adding absorption promoters to protect the insulin as it passes through the stomach.
Oral spray
An alternative to injected insulin that is currently being explored by researchers is a mouth spray containing insulin that would be absorbed through the lining of the mouth and throat. The liquid formulation allows the insulin to be absorbed by the mucus membranes in the cheeks, tongue, and throat. The benefit from oral spray is identical to an insulin injection in its ability to lower blood glucose levels.
Pulmonary or inhaled insulin
The inhaled insulin system delivers a dose of insulin, either in liquid or dry powder form, through the mouth, directly into the lungs, where it enters the blood circulation as rapid-acting insulin. With inhaled insulin, the highly permeable alveolar epithelium and large surface area of the lungs provide an effective, efficient portal for macromolecular delivery.
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
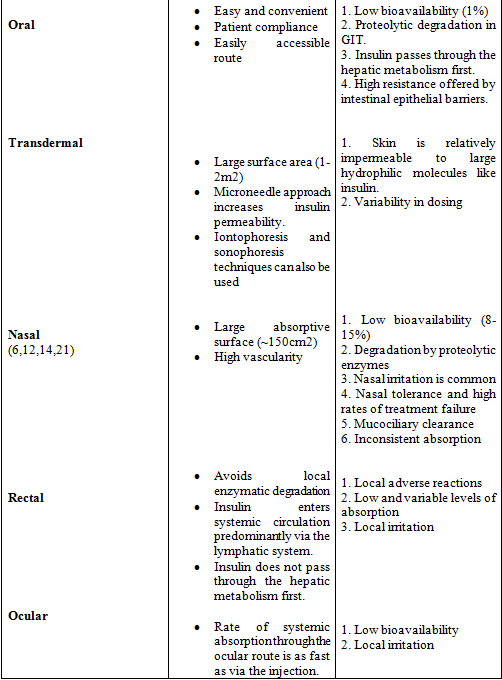
Different Routes Of Administration(45,46,47,48)

Marketed Oral Insulin Products
IN-105 (Biocon, Bangalore)
Biocon is developing the IN-105 conjugated insulin molecule, administered as a tablet. This oral insulin pill has polymers added at specific locations in the B chain of the insulin to prevent insulin from getting destroyed in the stomach (insulin is made up of two polypeptide chains namely, chain-A with 21 amino acids and chain-B with 30 amino acids, which are held together by two disulfide bonds). Biocon's R&D group has successfully developed a carefully selected formulation to give consistent absorption through the intestines, delivering the glucose-lowering effect. In the clinic, this molecule has completed phase I trials and is expected to enter phase II in India later this year to illustrate proof of concept. The encouraging results of the phase Ia and Ib studies represent a pivotal hurdle crossed in the development of IN-105 as a product. IN-105 will enter phase I trials in Europe towards the end of the year.
Oral-lyn (Generex Biotechnology, Canada)
Oral-lyn is the company's proprietary oral insulin spray product. The liquid formulation is absorbed into the body by the lining of the inner mouth using the company's proprietary RapidMist device. Since it is buccally absorbed, no insulin is deposited in the lungs by the Oral-lyn RapidMist. August 2007 saw the commercial launch of Oral-lyn in the Indian market. Generex Biotechnology entered into Master Product Licensing and Distribution Agreement of Oral-lyn with Shreya Life Sciences, the fourth largest distributor of insulin in India. In April 2008, Generex entered into a similar agreement for the distribution of Oral-lyn in China, Hong Kong, and the following additional countries: Indonesia, South Korea, Malaysia, the Philippines, Singapore, Thailand, and Vietnam. Presently, Generex Oral-lyn is in phase III clinical trials at several sites around the world—US, Canada and Ukraine.
Transgene (Biotek, Andhra Pradesh)
Transgene has developed an oral delivery technology which combines several oral delivery approaches into a single drug delivery system. Unique in its approach, this technology involves using biodegradable novel polymeric nanoparticles loaded with insulin as a new carrier to ferry the insulin across the intestinal epithelial tissues. Nanoparticles are solid spherical particles with a size range of 10 and 1,000 nm containing dispersed drugs. Transgene has attempted to improve the intestinal absorption of insulin and other peptides. The technology has been well proven in animal models, and human clinical studies are in progress. Drug companies are obviously interested in the potential of oral insulin to net a massive share of the market, and therefore, investment in research is substantial and ongoing. Biocon, Transgene Biotek and Generex Biotechnology have proven to be insightful in the race to enhance the treatment of diabetes, and are definitely ahead of the pack.
Conclusion
Attempts have been made to achieve oral insulin delivery using various systems. It has been proved that insulin is subjected to acid catalyzed degradation in stomach, luminal degradation in intestine, and intracellular degradation. Scientists have been able to protect the insulin delivery systems from acidic environment of the stomach and target it to the intestine. The maximum bioavailability of the insulin has been reported to be very low because of the poor absorption of insulin from the intestine. Attempts have been made to increase the absorption of insulin from intestine using absorption enhancers such as aprotinin (protease inhibitor), tween, oligoarginine, sodium glycol-cholate, deoxycholic acid, and taurodeoxycholate.
Liposomes, microemulsions, nanocubicles, etc., have been prepared for the oral delivery of insulin. Chitosan-coated microparticles protected insulin from the gastric environment of the body and released it in intestinal pH. Limitations to the delivery of insulin have not resulted in fruitful results to date and there is still a need to prepare newer delivery systems, which can produce dose-dependent and reproducible effects in addition to increased bioavailability.
References:
1. Al-Tabakha, M.M. and A.I. Arida, 2008. Recent challenges in insulin delivery systems: A review. Indian J. Pharm. Sci., 70: 278-86.
2. Diabetes mellitus, Information Available form: wikipedia. org
3. Insulin Delivery Systems Market Analysis, 2007- 2010. information available form:marketresearch. Com
4. Bell G I, Picket RL, Rutter WJ et al. Sequence of the humaninsulin gene. Nature 1980; 284: 26-32.
5. Gribble, F.M., and Reimann, F. 2003. Sulphonylurea action revisited: the post-cloning era. Diabetologia. 46:875-891.
6. Gribble, F., and Ashcroft, F.M. 2000. New windows on the mechanism of action of potassium channel openers [review].Trends Pharmacol. Sci. 21:439-445.
7. Nakamura K, Murray RJ, Joseph JI, Peppas NA, Morishita M, Lowman AM. Oral insulin delivery using P(MAA-g-EG) hydrogels: Effects of network morphology on insulin delivery characteristics J. Cont. Release,95: 589- 599 (2004).
8. Sajeesh S, Sharma CP. Cyclodextrin-insulin complex encapsulated polymethacrylic acid based nanoparticles for oral insulin delivery. Int. J. Pharm. 325(1-2): 147-154 (2006).
9. Jain D, Panda AK, Majumdar DK. Eudragit S100 entrapped insulin microspheres for oral delivery. AAPS PharmSciTech, 6(1), 1-27 (2005).
10. Lee VH. Oral route of peptide and protein drug delivery In Peptide and Protein Drug Delivery, Chapter 16, Marcel Dekker Inc., New York, 1991, 691–738.
11. Tuesca A, Lowman A. The oral delivery of insulin using protein conjugates in complexation hydrogels. Poster presentation, Biomaterials and Drug Delivery Laboratory, Drexel University, (2006).
12. Agarwal V, Khan MA. Current status of the oral delivery of insulin. Pharm. Tech.25(10), 76-90 (2001).
13. Patki VP, Jagasia SH. Progress made in noninvasive insulin delivery. Ind. J. Pharmacol. 28: 143-151 (1996).
14. Chang LL, Stout LE, Wong WD. Immunohistochemical localization of insulin degrading enzyme along the rat intestine, in the human colon adenocarcinoma cell line (Caco- 2) and in human ileum. J. Pharm. Sci. 81:116-119 (1999).
15. Agarwal V, Reddy IK, Khan MA. Polyethylacrylate-based microparticulate of insulin for oral delivery: preparation and in vitro dissolution stability in the presence of enzyme inhibitors.Int. J Pharm.; 225(1-2), 31-39 (2001).
16. Lin YH, Chen CT, Liang HF, Kulkarni AR, Lee PW, Chen CH. Novel nanoparticles for oral insulin delivery via the paracellular pathway. Nanotechnolog,18:105102, 1-10 (2007).
17. Toorisaka E, Hashida M, Kamiya N, Ono H, Kokazu Y, Goto M. An enteric-coated dry emulsion formulation for oral insulin delivery.J. Cont. Release 107: 91-96 (2005).
18. Schilling RJ, Mitra AK. Intestinal mucosal transport of insulin. Int. J. Pharm. 62: 53-64 (1999).
19. Kooshapur H, Chaideh M. Intestinal transport of human insulin in rat.Med. J. Islamic Academy of Science ; 12:1, 5-11 (`1999).
20. Pearlman R, Nguyen TH. "Analysis of Protein Drugs," in Peptide and Protein Drug Delivery, V.H.L. Lee, Marcel Dekker, New York, 1991.
21. Saadine JB, Cadwell B, Gregg EB, et al: Improvement in diabetes processes of care and intermediate outcomes: United States 1988-2002. Ann Intern Med 2006, 144:465-474.
22. Heinemann L, Jacques Y: Oral insulin and buccal insulin: a critical reappraisal. J Diabetes Sci Technol 2009, 3:568-584.
23. Wajchenberg BL: Beta-cell failure in diabetes and preservation by clinical treatment. Endocr Rev 2007, 28:187-218.
24. Skyler JS, Krischer JP, Wolfsdorf J, et al: Effects of oral insulin in relatives of patients with type 1 diabetes: the diabetes prevention trial-type 1. Diabetes Care 2005, 28:1353-1357.
25. Bergerot I, Arreaza GA, Cameron MJ, et al: Insulin B-chain reactive CD4+ regulatory T-cells induced by oral insulin treatment protect from type 1 diabetes by blocking the cytokine secretion and pancreatic infiltration of diabetogenic effector T-cells. Diabetes 1999, 48:1720-1729.
26. Stratton IM, Adler Al, Neil HAW, et al: Association of glycemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ 2000, 405-412.
27. Giovannucci E. Insulin and colon cancer. Cancer Causes Control. 1995;6(2):164-79.
28. Argiles JM, Lopez-Soriano FJ. Insulin and cancer (Review). Int J Oncol. 2001;18(4): 683-7.
29. Ish-Shalom D, Christoffersen CT, Vorwerk P, Sacerdoti-Sierra N, Shymko RM, Naor D, De Meyts P. Mitogenic properties of insulin and insulin analogues mediated by the insulin receptor. Diabetologia. 1997;40 Suppl 2:S25-31.
30. Cho YW, Flynn M. Oral delivery of insulin. Lancet ; 1518-1519 (1989).
31. Morishita M, Goto T, Nakamura K, Lowman AM, Takayama K, Peppas NA. Novel oral insulin delivery systems based on complexation polymer hydrogels: Single and multiple administration studies in type 1 and 2 diabetic rats . J. Cont. release 110:587-594(2006).
32. Ziv E, Lior O, Kidron M. Absorption of protein via the intestinal walls: A quantitative model . Biochem. Pharmacol . 39(7) 1035-1039 (1987).
33. Saffran M, Kumar GS, Savariar C, Burnham JC, Williams F, Neckers DC. A new approach to the oral administration of insulin and other peptide drugs. Science ; 233 (4768) : 1081-4 (1986).
34. Shah RB, Ahsan F, Khan MA. Oral delivery of proteins: Progress and prognostication. Crit. Rev. Ther. Drug Carrier Syst.19(2) : 135-169 (2002).
35. Salamat-Miller N, Johnston TP. Current strategies used to enhance the paracellular transport of therapeutic polypeptides across the intestinal epithelium . Int. J. Pharm . 294: 201-216 (2005).
36. Soltero R, Ekwuribe N. The oral delivery of protein and peptide drugs- A report. Innovat. Pharmaceut. Technol 1: 106-110 (2001).
37. Eaimtrakarn S, Ramaprasad YV, Ohno T, Konishi T, Yoshikawa Y, Shibata N. Absorption-enhancing effect of labrasol on the intestinal absorption of insulin in rats. J. Drug Target.10(3), 255-260(2002).
38. Rieux A, Fievez V, Garinot M, Schneider YJ, Preat V. Nanoparticles as potential oral delivery systems of proteins and vaccines: A mechanistic approach. J. Cont. Release ; 116: 1-6 (2006).
39. Giriraj KG, Giriraj KT. Oral Insulin-Fact or Fiction. Resonance 38- 43 (2003).
40. Yupeng R, Seng LT. Oral GIT – Hydrogel system for treating type 1 diabetes – A Report.
41. Choudhari KB, Labhasetwar V. Liposomes as a Carrier for Oral Administration of Insulin: Effect of Formulation Factors. Microencapsul. 11(3) , 315-325 (1994).
42. Al-Achi A, Greenwood R. Erythrocytes as Oral Delivery Systems for Human Insulin. Drug Dev. Ind. Pharm. 24(1) ,67-72 (1998).
43. Damge C, Vranckx H, Balschmidt P, Couvreur P. Poly (alkyl cyanoacrylate) Nanospheres for Oral Adminiatration of Insulin. J Pharm Sci.86, 1403-1409 (1997).
44. Chung H, Kim J, Um JY, Kwon IC, Jeong SY. Self-Assembled Nanocubicle as a Carrier for Peroral Insulin Delivery. Diabetologia 45(3), 448-451 (2004).
45. Varshosaz J. Insulin delivery system for controlling diabetes. Recent Pat Endocr Metab Immune Drug Discovery 2007; 1: 25-40.
46. Trihan A, Ali A. Recent approaches in insulin delivery. Drug Dev Ind Pharm 1998; 247: 589-597.
47. Sadrzadeh N, Glembourtt MJ, Stevenson CL. Peptide drug delivery strategies for the treatment of diabetes. J Pharm Sci 2007; 968:1925-1954.
48. Ghilzai NMK. New developments in insulin delivery. Drug Dev Ind Pharm 2003; 293:253-265.
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE









