About Auhtor:
Avula Parthasarthi Yadav*,
Krishna Theja Pharmacy College,
Jawaharlal Nehru University, Anantapur.
*parthu298@gmail.com
1. Introduction
Currently natural products are gaining popularity to combat various physiological threats including oxidative stress, cardiovascular complexities, cancer insurgence, and immune dysfunction. The use of traditional remedies may be encountered more frequently due to an array of scientific evidence in their favor1. It has been well established that nutrition plays an important role in the etiology of hyperlipidimia, atherosclerosis and other coronary heart disease (CHD) complications like myocardial infarction1.
The etiology and pathogencity of coronary heart diseases lie in the casual relationship between the development of atherosclerosis, elevated plasma lipid percentage cholesterol levels in blood and plasma, genetic makeup, endicrinological aberration, immunologic and autonomic factors, blood flow and coagulation2.
[adsense:336x280:8701650588]
REFERENCE ID: PHARMATUTOR-ART-1699
WHO (world health organization), indicates that coronary heart disease (CHD) alone accounts for more than half of the total mortalities associated with cardiovascular diseases3. Several well-recognized risk factors contribute to the development of CHD include hypertension, smoking, diabetes, hyperlipidemia, current cigarette smoking4.
To reduce the rate of mortality, it is therapeutically recommended to undergo diet or/and drug therapy to lower lipid levels within the normal range. Therapy of hyperlipidemia merits the consideration in the established atherosclerotic state2.
Allopathic hyperlipidemic drugs are available at large in the market but the side effects and contraindications of these drugs have marred their popularity5. The herbal hypolipidemics have gained importance to fill the lacunae created by the allopathic drugs. A number of plants have been found to be useful in hyperlipidemia. Condiments like garlic, onion and coriander used in day to day preparation of food in Indian kitchens have been identified as hypolipidemics in Ayurveda6.
The various parts of the plant Gmelina Arborea Roxb are widely used in diarrhoea, anti-pyretic, thirst, anaemia, leprosy, ulcers, consumption, strangury, vaginal discharges, and hyperlipidemic. Chemically plant is reported to contain Flavonoids, glycosides, steroids, fatty acids, fixed oils and waxes and small quantity of alkaloids. The literature survey offered no scientific claim on anti hyperlipidemic activity of Gmelina arborea Roxb.
2. Review of literature
1. Antihyperlipidemic activity of Bauhinia purpurea extracts in hypercholesterolemia albino rats.B.V.S. Lakshmi, N.Neelima, N.Kasthuri, V.Umarani, M. Sudhakar Department of Pharmacology, Malla Reddy College of Pharmacy, Bauhinia purpurea is a flowering plant. In the present study the ethanol extract of unripe pods and leaves of Bauhinia purpurea was evaluated for antihyperlipidemic activity in cholesterol high fat diet induced hyperlipidemia. The present work indicated that Bauhinia purpurea extracts significantly suppressed the CHFD induced hyperlipidemia in rats, suggesting the antihyperlipidemic and antiatherogenic potential of the extracts 80.
2. Antidiabetic and Antihyperlipidemic activity of roots of Boerhaavia diffusa on Streptozotocin induced diabetic rats. Krishna Murti, Vijay Lambole, Mayank Panchal, Upendra Kumar.Dept. of Pharmacology, Dr.K.N.Modi Institute of Pharmaceutical Education & Research Centre, Dept. of Pharmacology, Vidyabharti Trust College of Pharmacy. The present study was aimed to evaluate the anti diabetic - activity potential of Boerhaavia Diffusa roots against streptozotocin induced experimental rats. Glibenclamide was used as a standard drug. There was significant reduction in Total cholesterol, LDL cholesterol, VLDL cholesterol and improvement in HDL cholesterol in diabetic rats. These results indicated that Boerhaavia Diffusa possesses a hypoglycemic and antihyperlipidemic effect 81.
3. Anti-hyperlipidemic activity of methanol extracts of three plants of Amaranthus in triton-WR 1339 induced hyperlipidemic rats. K Girija, K Lakshman Department of Pharmacognosy, PES College of Pharmacy. To investigate the anti hyperlipidemic activity of methanolic extract of leaves of three plant of amaranthus. It is shows a significant antihyperlipidemic effect 82.
4. Investigation of hypoglycemic, hypolipidemic and antioxidant activities of aqueous extract of Terminalia paniculata bark in diabetic rats Subramaniam Ramachandran, Aiyalu Rajasekaran, KT Manisenthilkumar, Department of Pharmacology, KMCH College of Pharmacy, to investigate hypolipidemic, hypoglycemic and antioxidant activity of aquous extracts of terminalia paniculata. Diabetes was induced by giving injection of STZ. Present study results in diabetic conform that aquous extract of terminalia paniculata poossesses significant hypoglycemic, hypolipidemic and antioxidant activities83.
5. Antihyperlipidemic activity of Cinnamomum tamala Nees. on high cholesterol diet induced hyperlipidemia Varsha Dhulasavant, Shubhangi Shinde, Mangesh Pawar and N.S. Naikwade Department of Pharmacology, Appasaheb Birnale College of Pharmacy, Sangli, (MH)-India. The present study was designed to investigate the hypolipidemic effect of Cinnamomum tamala Nees. Leaves extracts in high cholesterol diet induced hyperlipidemia. Whereas significant (p<0.01) increases in the level of HDL-C 84.
6. Antihyperlipidemic studies on leaf extract of erythrina indica lam. Kamalraj R Bio Analytical Department, Quest Life Sciences, Chennai, Tamilnadu, India. The results are compared to that of standard drug, simvastatin 5mg/kg. So the present study supports the earlier claims of the plant in obesity 85.
7. Cardioprotective, antioxidant activities and phytochemical analysis by GC-MS of Gmelina arborea (GA) in Doxorubicin-induced myocardial necrosis in Albino rats. T.Vijay, M.S. Dhana Rajan, K.Sarumathy, S.Palani and K. Sakthivel. Doxorubicin (DOX) is a widely used cancer chemotherapeutic agent. It generates free oxygen radicals that result in serious dose-limiting cardiotoxicity. GA protects against DOX-induced cardiotoxicity in rats. The study can be attributed, at least in part, to GA’s antioxidant activity 86.
8. Screening of anti-diabetic activity of bark extracts of gmelina arborea in streptozotacin induced diabetic rats. Pattanayak. P, Parhi P.K, Mishra S. K, Khandei. Department of Pharmacognosy, Indiragandhi Institute of Pharmaceutical sciences, IMT Pharmacy College, Odisha, India.Accepted on: 14-03-2011; Finalized on: 05-06-2011. In the present investigation we have screened the Benzene, chloroform ethanolic, and aqueous extracts of the heart wood bark of the plant Gmelina arborea (family-Verbenaceae) for anti diabetic activity in Streptozotacin (STZ) induced Diabetic rats and emphasized the mechanism of its antidiabetic property. The observed significant antidiabetic activity of the ethanolic extract could be attributed to the increased blood GSH levels reinforcing the role of GSH as free radical scavenger and in the repair of free radical caused biological damage 87.
9. In vitro Antioxidant activity of methanolic extract of stem bark of gmelina arborea roxb. (Verbenaceae) Patil S.M., Kadam V.J. Department of Pharmacology, Bharati Vidyapeeth’s College of Pharmacy, This study the antioxidant activity of methanolic extracts of stem bark of Gmelina arborea Roxb. (Verbenaceae) (MEGA) was studied using various in vitro assays. The results of the study show that MEGA possesses significant free radical scavenging properties and a clear correlation exists between the antioxidant activity and phenolic content 88.
10. Anti Urolithiatic and anti hyperlipidemic activity of Coleus aromaticus an explanation of the underlying mechanisms. Venkatesh, Baburao, Rajesh babu, Dhanalakshmi, Indira priya darshinithe present study, the anti urolithiatic activity of Coleus aromaticus was investigated in ethylene glycol induced urolithiatic rats. Results from these studies support the safe and effective use of C.aromaticus leaves for urolithiasis treatment 89.
11. Effect of exogenous selenium on nicotine induced Hyperlipidemia in rats. Sreekala and M. Indira, Department of Biochemistry, University of Kerala. The effect of two different doses (1 μg Se/Kg and 50 μg Se/Kg Body wt) of selenium on nicotine induced hyperlipidemia was investigated in rats. Results revealed that nicotine intake caused an increase in concentration of cholesterol, triglycerides, free fatty acids, phospholipids and low density lipoprotein compared to control group. Histopathological studies revealed that selenium at a dose of 1 μg was more effective in reducing lipid levels and higher dose of selenium was toxic 90.
12. Evaluation of the antihyperlipidemic, cardioprotective activity of a polyherbal formulation Venu Pamidiboina, Rema Razdan, M.G.HariprasadAtherosclerosis is the leading cause of death in the developed and developing countries like India. It is associated withelevated lipid levels in the blood. Treatment of hyperlipidemia is one of the major approaches towards deceleratingthe atherogenic process. The objective of the study was to evaluate the antihyperlipidemic activity of Antichol,apolyherbal formulation in rats. It also significantly reversed the histopathological changes of heart. Antichol also lowered LPO levels and elevated GSH, SOD and CAT levels in heart homogenate 91.
13. Hyperlipidemia Induced by High Cholesterol Diet Inhibits Heat Shock Response in Rat Hearts, Ferdinandy,We examined whether heat shock response is affected by experimental hyperlipidemia in rat hearts. The HSP70 protein level was not different. This is the first demonstration that hyperlipidemia inhibits cardiac heat shock response. We further conclude that basal HSP70 expression might be down regulated at a posttranscriptional level in hyperlipidemia 92.
14. Ginseng Leaf Extract Prevents High Fat Diet-Induced Hyperglycemia and Hyperlipidemia through AMPK Activation Hai-Dan Yuan, Hai-Yan Quan, and Sung-Hyun Chung. This study evaluated the protective effects of ginseng leaf extract (GLE) against high fat-diet-induced hyperglycemia and hyperlipidemia, and explored the potential mechanism underlying these effects in mice. These results suggest that GLE ameliorates hyperglycemia and hyperlipidemia by inhibiting gluconeogenesis and stimulating lipolysis, respectively, via AMPK activation 93.
[adsense:468x15:2204050025]
2.1. Hyperlipidemia
Hyperlipidemia a broad term, also called hyperlipoproteinemia, is a common disorder in developed countries and is the major cause of coronary heart disease. It results from abnormalities in lipid metabolism or plasma lipid transport or a disorder in the synthesis and degradation of plasma lipoproteins.
The term “dyslipidaemia” now a days is increasingly being used to describe abnormal changes in lipid profile, replacing the old term hyperlipidaemia. Hyperlipidemia means abnormally high levels of fats in the blood. These fats include cholesterol and triglycerides. These are important for our bodies to function but when they are high, they can cause heart disease and stroke.
Hyperlipidemia is manifested as hypercholesterolemia and hypertriglycerolemia. Hypercholesterolemia is the most common hyperlipidemia. The lipids that are involved in hypercholesterolemia are cholesterol, an essential component of cell membrane and a precursor of steroid hormone synthesis and triglycerides, an important energy source. They are transported in blood as lipoproteins. The consequence of hyperlipidaemia is that with time it can cause atherosclerosis, and thus the risk of coronary heart disease and stroke is increased. However, according to the newer scientific view, the cholesterol level alone is not the whole story. The risk of heart disease in future also depends on many other factors that influence the health of a person’s blood vessels and circulation7.
LDL is strongly associated with a higher risk, and HDL is associated with a lower risk, of coronary heart disease (CHD). Lowering lipids through dietary or pharmacological therapy has been shown to decrease the incidence of atherosclerotic events. Since lipid levels have been observed to track into adulthood, adolescents with hyperlipidemia are also at greater CHD risk. The extent of abnormal lipids and other cardiovascular risk factors during childhood and adolescence is related to the severity of atherosclerosis seen in autopsies of young adults.8
Patients with DM are at significantly increased risk of CHD compared with non diabetic patients of similar age. DM patients without known CHD appear to have a risk for first MI similar to the risk for recurrent MI of non-DM patients with CHD and a prior coronary event. Patients with type 2 diabetes commonly have other risk factors (hypertension, high LDL-C, low HDL-C, obesity) that increase risk for cardiac events 9.
High lipid levels can speed up a process called atherosclerosis, or hardening of the arteries. Your arteries are normally smooth and unobstructed on the inside, but as age, a sticky substance called plaque forms in the walls of arteries. Plaque is made of lipids and other materials circulating in blood. As more plaque builds up, arteries can narrow and stiffen. Eventually, enough plaque may build up to reduce blood flow through arteries10.

Hyperlipidemia is typically asymptomatic and is frequently detected during routine screening.
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
Hyperlipidemia often results from delayed or defective clearance, or overproduction of VLDL by the liver, which is subsequently transformed into LDL. Hypercholesterolemia involves defective hepatic and nonhepatic LDL receptors. Excess intake of saturated fats increases the liver's production of VLDL and triglycerides via a molecular mechanism involving protein activators.1 Saturated fats are found in animal products, such as meat, whole milk dairy products (milk, cream, cheese), and butter, and tropical oils (palm, palm kernel, and coconut).
High concentrations of total and LDL cholesterol and low levels of high-density lipoprotein (HDL) cholesterol predict cardiovascular risk in both men and women. High triglyceride levels have been associated with greater risk in women only. The risk of cardiovascular disease increases by an average of 2% for each corresponding 1% rise in total cholesterol. Adolescents with “high” TC or LDL may have a genetic disorder of lipid metabolism such as familial hypercholesterolemia or familial combined hypercholesterolemia. Those with homozygous forms of these disorders can experience myocardial infarction or other events during childhood or early adolescence. Familial hypercholesterolemia is often diagnosed in adolescence and is characterized by high LDL levels that can be refractory to dietary treatment. These patients can present clinically with xanthomas or xanthelasma– cholesterol deposits under the skin on the hands, elbows, knees, heel or eyelids7.
HISTORY:-
The Norwegian physician Dr C. Muller first associated the physical signs, high cholesterol levels and autosomal dominant inheritance in 1938. In the early 1970s and 1980s, the genetic cause for FH was described by Dr Joseph L. Goldstein and Dr Michael S. Brown of Dallas, Texas. Initially, they found increased activity of HMG-CoA reductase, but studies showed that this did not explain the very abnormal cholesterol levels in FH patients. The focus shifted to the binding of LDL to its receptor, and effects of impaired binding on metabolism; this proved to be the underlying mechanism for FH. Subsequently numerous mutations in the protein were directly identified by sequencing. They later won the 1985 Nobel Prize in Medicine for their discovery of the LDL receptor and its impact on lipoprotein metabolism.
Types of Hyperlipidemia:-
Depending on the complexity of the disease, Hyperlipidemia classified into two types.
1) Primary Hyperlipidemia.
2) Secondary / Acquired Hyperlipidemia.
I) Primary Hyperlipidemia11, 12:-
Several genetic conditions are known to responsible for primary Hyperlipidemia, such as lipoprotein lipase deficiency, apolipoprotein C-II deficiency etc...The primary hyperlipidemia may be treated by anti-lipidemic drugs. Primary Hyperlipidemia are again classified into 5 types
1. Type-I Hyperlipidemia:-Severe elevation of CMs with resultant elevation of TGs.
2. Type-II (A) Hyperlipidemia:-Elevations of LDL –C only.
3. Type-II (B) Hyperlipidemia:-Elevations of both LDL-C and TGs.
4. Type-III Hyperlipidemia: - It develops due to defect in VLDL remnant Clearance.
5. Type-IV Hyperlipidemia: - It is characterized by hyper TGs
6. Type-V Hyperlipidemia:-characterized by elevated levels of CMs and VLDL.
II) Secondary Hyperlipidemia:-
In this many factors can influence the level of TGs in circulation like diabetes, obesity etc. Secondary Hyperlipidemia demands treatment of original diseases rather than Hyperlipidemia.
Causes of secondary Hyperlipidemia:-
A.Metabolic influences:-diabetes, obesity, hyperuricemia, glycogen storage disease typeI.
B. Harmonal influences:-insulin, estrogen, thyroxine
C. Nutritional influences:-alcohol, high carbohydrate intake
D. Disease states:-Renal diseases, renal failure, nephritic syndrome
E. Drugs: - Diuretics
Beta-blockers
Glucocorticoids
Estrogen replacement therapy11, 13
There are several secondary causes of abnormal lipids that may occur in adolescence. Children small for gestational age as infants have been shown to have higher levels of cholesterol, especially those who exhibit poor catch-up growth10. The starved state that occurs in anorexia nervosa and the use of anabolic steroids are both associated with abnormal lipids. Certain medications for acne, seizure disorders, immunosuppression, and contraception can adversely affect lipids as can a high carbohydrate diet or a ketogenic diet sometimes prescribed for refractory epilepsy. Adolescents with a history of a transplant also tend to have an abnormal lipoprotein panel despite a TC in the normal range.
Risk factors9:-
Positive risk factors:-
1. Age (males > 45 years, females > 55 years)
2. Family history of premature coronary artery disease; definite myocardial infarction (MI) or sudden death before age 55 in father or other male first-degree relative, or before age 65 in mother or other female first-degree relative
3. Current cigarette smoker
4. Hypertension (systolic blood pressure > 140 mmHg or diastolic blood pressure > 90 mmHg confirmed on more than one occasion, or current therapy with antihypertensive medications)
5. Diabetes mellitus (DM)
6. High-density lipoprotein (HDL)-cholesterol < 40 mg/dl
Negative risk factor:-
Elevated HDL cholesterol, > 60 mg/dl
Etiology 14:-
The etiology can be classified into primary and secondary causes.
Primary causes are due to single or multiple gene mutations resulting in a disturbance of LDL and triglyceride production or clearance. They vary in location of genetic defect, inheritance pattern, prevalence, clinical features, and treatment. At least 18 separate entities have been described. The suspicion for a primary lipid disorder should be especially high in patients with premature atherosclerotic disease, a family history of early atherosclerotic disease, a significantly elevated serum cholesterol level (>240 mg/dl), and physical signs of hyperlipidemia. Primary dyslipidemias are most commonly seen in children and young adults and cause only a small percentage of cases in adults.
Most adult cases of dyslipidemia are secondary in nature. In Western civilizations, sedentary lifestyle and excessive consumption of saturated fats, trans-fatty acids, and cholesterol are the most important secondary causes. Certain medical conditions are commonly associated with dyslipidemia, including chronic renal insufficiency, renal failure, diabetes mellitus, hypothyroidism, cholestatic liver disease, and alcohol dependency. Certain drugs, including high-dose thiazide diuretics, oral estrogens, glucocorticoids, anabolic steroids, and atypical antipsychotics such as olanzapine and clozapine have also been implicated in causing mild-to-moderate degrees of dyslipidemia. Use of atypical antipsychotics, such as olanzapine and clozapine, and of beta-blockers without intrinsic sympathomimetic or alpha-blocking activities is associated with reduced HDL-cholesterol levels.
(Table-1) Etiologies of Hyperlipidemia15:-
|
Phenotype |
Elevated Particles |
Major Lipid Abnormality |
Frequency |
Etiology |
|
I |
Chylomicrons |
TG |
Very rare |
LPL deficiency, apoC-II deficiency, inhibition of LPL (eg, systemic lupus erythematosus) |
|
IIA |
LDL |
LDL-C |
Common |
FH, FCH, polygenic hypercholesterolemia, hypothyroidism, renal disease ,biliary tract disease, diabetes mellitus |
|
IB |
LDL and VLDL |
LDL-C, TG |
Common |
Similar to type IIA HLP |
|
III |
IDL |
TC, TG |
Rare |
ApoE-2 homozygosity (E-2/E-2) plus obesity, diabetes mellitus, renal disease, hypothyroidism, or liver disease |
|
IV |
VLDL |
TG |
Common |
FCH, FH, metabolic/endocrine disease*, renal disease, liver disease, ethanol use/abuse, pregnancy, drug use. |
|
V |
Chylomicrons and VLDL |
TG |
Uncommon |
Usually results from a combination of any two conditions that cause type IV HLP |
Pathophysiology 14:-
Hypercholesterolemia develops as a consequence of abnormal lipoprotein metabolism, mainly reduction of LDL receptor expression or activity, and consequently diminishing hepatic LDL clearance from the plasma. It is a major predisposing risk factor for the development of atherosclerosis. This mechanism is classically seen in familial hypercholesterolemia and when excess saturated fat or cholesterol is ingested. In addition, excessive production of VLDL by the liver, as seen in familial combined hyperlipidemia and insulin resistance states such as abdominal obesity and type 2 diabetes, can also induce hypercholesterolemia or mixed dyslipidemia.
A current theory for the initiating event in atherogenesis is that apoprotein B-100 containing lipoproteins are retained in the subendothelial space, by means of a charge-mediated interaction with extracellular matrix and proteoglycans. This allows reactive oxygen species to modify the surface phospholipids and unesterified cholesterol of the small LDL particles. Circulating LDL can also be taken up into macrophages through unregulated scavenger receptors. As a result of LDL oxidation, isoprostanes are formed. Isoprostanes are chemically stable, free radical-catalyzed products of arachidonic acid, and are structural isomers of conventional prostaglandins. Isoprostane levels are increased in atherosclerotic lesions, but they may also be found as F2 isoprostanes in the urine of asymptomatic patients with hypercholesterolemia.
A strong association exists between elevated plasma concentrations of oxidized LDL and CHD. The mechanisms through which oxidized LDL promotes atherosclerosis are multiple and include damage to the endothelium, induction of growth factors, and recruitment of macrophages and monocytes.
Vasoconstriction in the setting of high levels of oxidized LDL seem to be related to a reduced release of the vasodilator nitric oxide from the damaged endothelial wall as well as increased platelet aggregation and thromboxane release. Smooth muscle proliferation has been linked to the release of cytokines from activated platelets.
The state of hypercholesterolemia leads invariably to an excess accumulation of oxidized LDL within the macrophages, thereby transforming them into "foam" cells. The rupture of these cells can lead to further damage of the vessel wall due to the release of oxygen free radicals, oxidized LDL, and intracellular enzymes.
This is a metabolically complex disease of lipid -lipoprotein metabolism and the exact etiology is not fully appreciated. The familial type in schnauzers may involve defects lipoprotein lipase and/or Apoprotein C-II, a required cofactor for lipoprotein lipase activity. This defect causes a failure to breakdown chylomicronsand VLDL, and results in excessive levels of circulating triglycerides. It is the elevated concentration of triglycerides that is responsible for the clinical signs.
Lipids16:-
Lipids are a group of naturally occurring fatty substances that are present in the blood and tissues of the body. They include cholesterol, cholesterol esters, triglycerides, and phospholipids. Lipids are essential dietary constituents because of their important functions.
Classification of lipids:-
* Fatty acids (palmetic, linoleic, etc)
* Glycerol esters (triglycerides)
* Sterols (cholesterol, hormones, vitamin D)
* Terpenes (vitamin A, E, K)
* Sphingosine derivatives (sphingomyelin)
Lipid functions 79:-
- Provide energy required by the body
- Serve as the major structural components of cell membranes
- Aid in the efficient absorption of fat-soluble vitamins
- Serve as insulating material beneath the skin and around certain organs (e.g. kidneys)
- Serve as biosynthetic precursors (e.g., Cholesterol is a precursor for adrenal and gonadal steroid hormones and hepatic bile acids.)
Lipids are insoluble in blood (plasma), they must be transported to and from the cells by special carriers called lipoproteins. Lipoproteins are spherical particles of high molecular weight. Each lipoprotein particle contains a non-polar core and a hydrophilic surface. The hydrophilic surface makes the lipoprotein soluble in plasma and acts as an interface between the plasma and lipid core. The core consists of hydrophobic lipids, triglycerides and cholesterol esters, surrounded by a hydrophilic surface coat of phospholipids, unesterified cholesterol, and specific proteins termed apolipoproteins or apoproteins. The apolipoproteins provide structural integrity to the lipoproteins and determine the lipoproteins’ metabolic fate by serving as binding sites for receptors and activating enzymes involved in lipid metabolism.
Evaluation of Lipid Levels for People at High Risk for CHD:- (Table-2)
|
|
Total |
|
LDL |
HDL Cholesterol |
|
Desirable levels |
<200 |
<150 |
<130 |
>35 |
|
Borderline risk |
200-239 |
150-200 |
130-159 |
30-35 |
|
High risk |
>240 |
>200 |
>160 |
<30 |
Modestly elevated Lp (a) levels = 20-30 mg/dl
There is a 10-fold risk of heart attack when Lp (a) levels are > 50 mg/dl in people with high cholesterol levels.
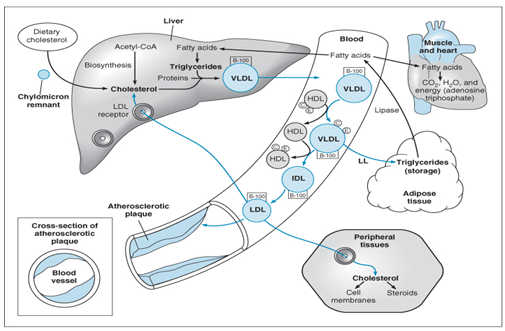
Lipid transport 79:-
Lipids are carried in plasma in lipoproteins after getting associated with several apoproteins plasma lipid concentrations are depended on the concentration of lipoproteins. The core of lipoprotein globules consists of TG and cholesteryl esters. The outer polar layer has phospholipids, free cholesterol and apoproteins. Dietary lipids are absorbed in the intestine with the help of bile acids. Chylomicrons are formed and passed in to lacteals reach blood stream via thoracic duct. Liver secrets very low density lipoproteins containing mainly TG and CHE in to blood. VLDL is acted upon by endothelial lipoprotein lipase in the same way chylomicrons and the fatty acids pass in to adipose tissue and muscle. The remnant called IDL now contains more CHE than TG about half of the IDL is taken back by the liver cells by attachment to another receptor (LDL) while the rest lose the TG and becomes LDL containing only CHE.
Pathways of Lipid Transport 16:-
Cholesterol is absorbed from the intestine and transported to the liver by chylomicron remnants, which are taken up by the lowdensity lipoprotein (LDL)-receptor related protein (LRP). Hepatic cholesterol enters the circulation as very-low-density lipoprotein (VLDL) and is metabolized to remnant lipoproteins after lipoprotein lipase removes triglyceride. The remnant lipoproteins are removed by LDL receptors (LDL-R) or further metabolized to LDL and then removed by these receptors. Cholesterol is transported from peripheral cells to the liver by high-density lipoprotein (HDL). Cholesterol is recycled to LDL and VLDL by cholesterol-ester transport protein (CETP) or is taken up in the liver by hepatic lipase. Cholesterol is excreted in bile. The points in the process that are affected by the five primary lipoprotein disorders and familial hypertriglyceridemia (FHTG), familial combined hyperlipidemia (FCHL), remnant removal disease (RRD, also known as familial dysbetalipoproteinemia), familial hypercholesterolemia (FH), and hypoalphalipoproteinemia shown. The effects of drug therapy can also be understood from these pathways. Statins decrease the synthesis of cholesterol and the secretion of VLDL and increase the activity of LDL receptors. Bile-acid binding resins increase the secretion of bile acids. Nicotinic acid decreases the secretion of VLDL and the formation of LDL and increases the formation of HDL. Fibrates decrease the secretion of VLDL and increase the activity of lipoprotein lipase, thereby increasing the removal of triglycerides.
Enzymes of importance in lipid transport & metabolism17, 18, 19:- (Table-3)
|
Enzymes |
Functions |
|
Lipoprotein lipase |
Hydrolysis of TG rich particles some phospholipase activity activated by APO C-II |
|
Hepatic lipase |
Hydrolysis of Tri-, Di- and mono acyl-glycerol’s, acyl-CoA thioester and phospholipids conversion of HDL2 to HDL1 activated by apoA- II |
|
Pancreatic lipase |
Hydrolysis of FAs at positions 1 and 3 of emulsified TGs in the intestine. |
|
Lecithin cholesterol Acyl transferase LCAT |
Catalysis of lecithin with cholesterol to give lysolecithin and cholesteryl ester activated by apo A-I and apo c -I. |
|
Pancreatic cholsterolesterase |
Esterification of cholesterol in the intestinal lumen |
|
Acyl co A-cholesterol acyl transferase ACAT |
Esterification of cholesterol with in the cells |
|
Cholesterol ester transfer protein CETP |
Transfers esterified cholesterol from HDLs to VLDLs and LDLs. |
|
HMG Co A reductase |
Rate limiting enzyme of cholesterol synthesis |
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
Lipoproteins:-
Lipoproteins are proteins carrying lipids cholesterol is one of the lipids. Long chain fatty acids are also carried by these lipoproteins in the form of TG.

General structure of lipoprotein:- (Figure-5)
There are several forms of lipoproteins, very low density lipoproteins, intermediate density lipoproteins (IDL), low density lipoproteins (LDL), and high density lipoproteins (HDL). Lipoproteins are large globular particles which transport cholesterol and triglycerides in the blood stream. They consist of central core of cholesterol or cholesterol esters encased in a hydrophilic coat of polar substance, i.e. phospholipids, free cholesterol and associated proteins (apoprotein).
Classification of Lipoproteins: - (Table-4)
|
|
Composition |
Density |
Size |
|
Chylomicrons |
TG >> C, CE |
low |
Large |
|
VLDL |
TG > CE |
Higher than chylomicrons |
Smaller than chylomicrons |
|
ILDL |
CE > TG |
higher than VLDL |
smaller than VLDL |
|
LDL |
CE >> TG |
higher than ILDL |
smaller than ILDL |
|
HDL |
CE > TG |
highest |
smallest |
The six major classes of plasma lipoproteins are 17:-
- Chylomicrons: - Particles of the lowest density that appear in the blood shortly after fat has been digested and absorbed from the small intestine. They transport dietary cholesterol and triglycerides to muscles (for energy), to fat tissue (for storage), and to breasts (for milk production).
- Very low-density lipoproteins (VLDL):- Particles synthesized by the liver that transport triglycerides to muscles (for energy) and to fat tissue (for storage).
- Intermediate density lipoproteins (IDL):- Particles formed as the triglyceride portion of the VLDLs are removed. IDLs are either converted to LDLs or directly taken up by the liver.
- Low-density lipoproteins (LDL):- Particles that are the primary plasma carriers of cholesterol. LDL is also known as the "bad cholesterol" because excess LDL cholesterol in the blood with other substances can form plaques that can clog the arteries feeding the heart and brain. The formation of plaques in the arteries is a condition known as atherosclerosis in medical terminology. If a clot forms in the region of the plaque, blood flow to part of the heart muscle can become blocked which can lead to heart attack. If the clot cuts off blood flow to the brain, it can cause a stroke.
- High-density lipoproteins (HDL):- HDL is known as the "good cholesterol" because it mediates the removal of cellular cholesterol. HDL carries cholesterol away from body cells and tissues to the liver for excretion from the body. A high HDL level is associated with a lower risk for coronary heart disease (CHD).
- Lipoprotein (a) (Lp(a)):- Particle similar in composition to LDL but has an additional apoprotein, apo(a), covalently linked to apo B. Lp(a) is called the "deadly cholesterol" because it is 10 times more dangerous than low-density lipoprotein (LDL) and 15 times more potent than total cholesterol. Lp(a) levels are almost exclusively governed by race, ethnicity, and genetics, unlike other blood fats that are governed by age, gender, diet, and other environmental factors. A high level of Lp(a) is a risk factor for developing atherosclerosis prematurely. Patients at high risk for CHD should make major lifestyle changes (exercise routinely, avoid smoking, and monitor their weight, cholesterol, waist size, and calorie intake) to avoid the development of adverse lipid profiles that will magnify the deadly effects of elevated Lp(a) levels.
Obtain Total Cholesterol (TC) and HDL or TC, HDL, TG, LDL 9:-
To risk-stratify patients for targeted intervention versus follow-up screening.
Lipid levels may be obtained in a fasting or nonfasting state. TC levels and HDL-C can be measured in the nonfasting patient.
TG concentrations, however, are affected by recent food intake and will affect the calculation of LDL-C by the Friedewald equation: LDL-C = [TC] - [HDL-C] - [TG/5]. Therefore always order the lipid profile in a fasting state to avoid any errors.
Clinical decisions should be based on two lipid profiles, done 1 to 8 weeks apart, which have an LDL-C or TC difference of < 30 mg/dL.
Recent myocardial infarction, stroke, surgery, trauma, or infection may transiently lower cholesterol levels up to 40 percent. If a lipid profile cannot be obtained immediately (within 12 to 24 hours of the event), one must wait 8 weeks post-event to obtain an accurate reading.
Cholesterol levels increase by as much as 20 to 35 percent during pregnancy and should not be measured until three to four months after delivery.
Chylomicrons:-
These are the largest species of triglyceride rich lipoprotein which are involved in the transportation of dietary fat from intestine to liver.
These are secreted into the lymph. (Fats are broken down into fatty acids in the digestive tract, and then packaged together in groups of three. A triglyceride contains three fatty acids attached to glycerol.).
Fat digesting enzymes break down chylomicrons fairly quickly, so most are gone from the blood after a 12 to 14 hour fast.
VLDL: -
VLDL or "very low-density lipoproteins" involved in transport of endogenous lipids from liver to plasma. Formed in the liver and intestines, VLDL carry about 10 to 15 percent of the cholesterol found in blood.
VLDL delivers cholesterol and triglycerides to cells, which in turn put these lipid products to use.
Lipase Lipase
VLDL --------------> IDL -------------> LDL
Through the action of fat-digesting enzymes, VLDL becomes progressively smaller as it circulates through the bloodstream. VLDL also converts to LDL, which is the chief culprit in atherosclerosis.
Total cholesterol:-
An increasing total cholesterol level is associated with an increased risk of CHD (coronary heart disease).
|
Total cholesterol mg/dl = Abs TC/Abs STD ×200 |
“Desirable" total cholesterol is usually <200>
However, most decisions about treatment are made based upon the level of LDL or HDL cholesterol, rather than total cholesterol. The total cholesterol can be measured any time of day. You don't have to be fasting.
LDL cholesterol:-
The low density lipoprotein (LDL) cholesterol (sometimes called "bad cholesterol") is a more accurate predictor of CHD than total cholesterol.

Figure-6
[LDL-chol] = [Total chol] - [HDL-chol] - ([TG]/5)
Where all concentrations are given in mg/dL.
Higher LDL cholesterol concentrations have been associated with an increased incidence of CHD in a large number of studies. They have longest plasma half-life of about 1.5 days amongst the lipoproteins.
Ideally