{ DOWNLOAD AS PDF }
ABOUT AUTHORS
Srinivasa Babu Puttagunta, Sowjanya Pulipati, Sai Koushik Oruganti
Vignan Pharmacy College, Vadlamudi, Guntur, Andhra Pradesh
kaushikoruganti555@gmail.com
ABSTRACT
Introduction: Clinical pharmacists work directly with doctors, health professionals and patients to ensure that the medications prescribed for patients contribute to the best possible health outcomes. Therefore, pharmacy students should be given opportunities to learn and practice interpersonal communication skills.
Objectives: This observes opinions the position of the pharmacist preceptor in facilitating improvement of conversation capabilities for students participating in community in community advanced pharmacy practice experiences.
Material and methods: Preceptors need to set a stage to comprise precepting into the workflow and to offer green and effective teaching opportunities. College students ought to go through practical activities like affected person counseling and participating in collaborative work with health care professionals. Preceptors should incorporate the teaching in a lively and demonstrative way for a better impact on their students.
Results and discussion: By following a strategic approach in the methods of teaching the preceptors can effectively and likely enhance the communication skills of the students.
Conclusion: The incorporation of communication skills to pharmacy practice can positively impact the pharmacy site, preceptor, student and more importantly patient.
[adsense:336x280:8701650588]
REFERENCE ID: PHARMATUTOR-ART-2444
|
PharmaTutor (ISSN: 2347 - 7881) Volume 4, Issue 11 Received On: 09/06/2016; Accepted On: 29/06/2016; Published On: 01/11/2016 How to cite this article: Puttagunta SB, Pulipati S, Oruganti SK; Effective precepting to enhance Communication Skills of Pharmacy Students; PharmaTutor; 2016; 4(11); 27-32 |
INTRODUCTION
Pharmacists work directly with doctors, health professionals and patients to ensure that the medications prescribed for sufferers make contributions to the best possible health outcomes. Therefore, pharmacy college students need to be given opportunities to learn and practice interpersonal conversation skills. [1-2]
COMMUNICATION SKILL
The capacity of pharmacist to communicate virtually with patients, physicians and nurses.
POOR COMMUNICATION
Poor communication skill between pharmacist and patient leads to:
-erroneous affected person medicinal drug history
-irrelevant healing decisions
-ends in patient confusion, affected person disinterest and patient non-compliance
Learning Objectives
• Apprehend and internalize that in your function as preceptor, you are a tangible and powerful role version for students.
• Describe four key attributes that lead one to grow to be a powerful preceptor.
• Specify the traits of a premiere gaining knowledge of environment at the experiential exercise web page, and expand practical rotation goals & expectations of college students.
• Compare and specific to the pupil vital formative and summative remarks for the duration of the experiential rotation.
• Examine & take delivery of pertinent constructive critique of the experiential imparting from the students.
• Dedicate yourself to ongoing preceptor improvement & networking possibilities.
Understanding the Preceptor Role: What is a “Preceptor”?
Preceptor: An instructor; a teacher. A professional or professional, inclusive of a physician, who offers practical experience and schooling to a student. A preceptor is a qualified practitioner who offers transitional role support and effective scientific gaining knowledge of for a scholar inside a collegial partnership. A preceptor helps the increase and improvement of a student for a predetermined duration of time with the precise reason of socializing and integrating that student into a new position. A preceptor wears the hat of teacher, coach, mentor, facilitator, and educate. [3-4]
METHODS
Four Keys to Effective Precepting
• Communications & practice
• Skillful teaching
• Motivating the Learner
• Careful evaluation of the Learner
• Explains the basis for movements & choices
• Solutions learner questions clearly & precisely, in non-judgmental way
• Is open to conflicting ideas and opinions
• Communicates clean dreams & rotation targets
• Provide written rotation agenda on day 1
• Evaluation rotation targets on day 1; ask college students for any changes
• Holds realistic expectancies of college students:
• #, kind, best of assignments
• Captures learner’s interest & makes studying amusing!
• Makes the learner experience like a priority
Careful Analysis of the Learner
• Accurately assesses the learner’s knowledge, attitudes and competencies
• Makes use of direct observation of the learner
• Provides frequent and effective remarks to students on rotation
• Plays honest and thoughtful critiques
• Files pupil progress frequently, giving adequate “warning” and opportunity for development if rotation failure is a robust possibility
• If remediation vital, makes use of the assessment/consequences record to gauge scholar overall performance and behavior greater common (than midpoint/final) opinions w/ clear coaching on development.
Skillful Teaching and Practice
Demonstrates skillful interactions with sufferers
Presents powerful role modeling
Gives statistics with employer and readability
Organizes and controls the getting to know enjoy
Offers suitable duty to the learner
Balances scientific and coaching responsibilities
Offers ample gaining knowledge of possibility at the website (carry out interest, be evaluated, see outcomes of interventions/tasks)
Motivating the Learner
• Emphasizes hassle solving
• Promotes active involvement of the learner
• Demonstrates amusement and enthusiasm for patient care and coaching
• Develops a supportive dating with the learner
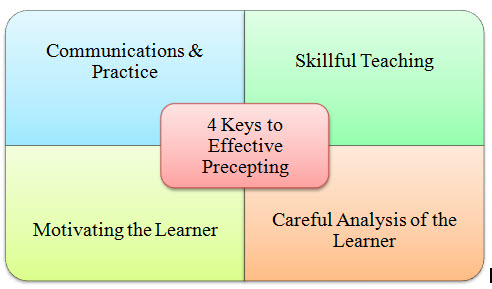
Figure 1 shows the four keys to effective precepting
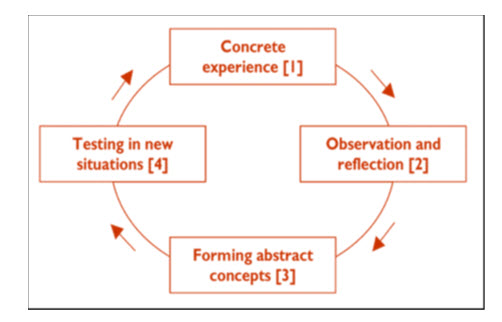
Figure 2 shows the Optimal Experiential Learning Environment
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT editor-in-chief@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
TYPES OF COMMUNICATION [5]
There are two types of communication skill:
NON-VERBAL COMMUNICATION:
VERBAL COMMUNICATION:
NON VERBAL COMMUNICATION:
I. EYE CONTACT:
It indicates confidence, attention and honesty.
II. FACE EXPRESSION:
An important indicator of emotional state.
III. BODY POSTURE:
Message can be conveyed through body posture.
E.g.: Closed body posture: person sitting with his legs and arms crossed in front of their body.
This prevents or hinders the free flow of information.
Open body posture: A relaxed stance with uncrossed legs and arms.
It tends to ease communication.
IV. TONE OF VOICE:
Soften voice etc can also influence the communication.
V. PROXIMITY/CLOSENESS OF POSITION:
The pharmacist and patient must maintain a minimum distance of 45cm.
VI. ANOTHER FORM OF NON-VERBAL MESSAGE:
To convey information through the use of diagrams.
E.g. used in place of medicine labels for illiterate.
May demonstrate how to administer a dosage form such as eye drops.

VERBAL COMMUNICATION SKILL
Essential verbal communication skills include the:
Ability to listen, understand and respond to what people say (active listening)
Ability to interpret the non-verbal communication and respond in a way that encourages continued interaction (evaluation).
Keeping eye contact, nodding, asking questions etc indicate: 2.5.2.1
ATTENTION-tone and modulation of voice, number and placement of pauses
RELIABILTY OF PATIENT PROVIDED INFORMATION
Low level of energy, flat effect, monotone voice:
DEPRESSED.
PAUSES: indicate the person needs time to recall the information or the person is censoring the response or preparing to lie.
OBSERVATION AND ASSESSMENT:
Effective two way communication requires:
- Continual observation
- Assessment of how the person is communicating
Body language and gestures provide important clues for pharmacist, patient and health care professional.
[adsense:468x15:2204050025]
SIT OR STAND AT EYE LEVEL:
Maintain eye contact
Use focussed body posture to convey interest and attentiveness.
OPEN COMMUNICATION:
Sitting or standing at eye level or lower projects a non-threatening, equalising body posture.
Physically be close to patient, family member or healthcare professional
LANGUAGE:
For reliable communication; use a language in which both parties are fluent and comfortable.
Abbreviations and terms used for prescribing medicines represent a specialised type of communication.
Do not produce fear, anxiety in patients by saying medical terms.

Figure 3 shows the various forms of verbal communication
APPLICATIONS
COMMUNICATING WITH THE HEALTH PROFESSIONALS:
Effective communication between pharmacist and physicians, nurses and other pharmacists is essential.
Pharmacist- Physician Communication:
Be prepared with specific questions or facts and recommendations when initiating a patient care-related conversation with physicians.
COMMUNICATION WITH PATIENTS:
I. MEDICATION HISTORY INTERVIEW: are required for making decisions.
The following information is recorded:
1) Currently or recently prescribed medicines.
2) OTC medicines purchased.
3) Vaccinations
4) Alternative or traditional remedies
5) Description of reactions and allergies to medicines.
6) Medicines found to be ineffective.
TEACHING:
-A teacher must be organised and knowledgeable about the subject being taught and must be an excellent communicator.
-Communication is enhanced by good organisational skills.
-Direct questioning and assessment of responses are easy ways to determine the responses of students.
PLATFORM AND POSTER PRESENTATION:
PLATFORM PRESENTATION:
-Pharmacists make platform presentations at local, state and national professional meetings.
POSTER PRESENTATION:
-Unique form of communication in which the information is displayed than oral
-Posters that attract the most attention have clear, descriptive titles and a colourful, neat professional appearance.
-Visual aids like graphs, charts and photographs communicate information effectively.
MEDIA INTERVIEWS:
-Media is an effective form of communication between pharmacist and the public.
-Pharmacists are called by the media to provide background information regarding therapeutic issues such as the marketing of an important new drug, drug related problems or the withdrawal of the drug from market.
MANUSCRIPTS:
-Original research reports, case studies, review articles, editorials and letters to the editor are important communication tools among health professionals.
-Well written manuscripts that meet the needs of the journal’s audience will be published.
GRADE Strategy
• G: Get ready
– Review course syllabi, standardized objectives, evaluation form
– Consider incorporation of site-specific unique opportunities
– Set student expectations (factor in rotation sequencing; prior experiences; IPPE or APPE, etc.)
R: Review Expectations w/ Student
– Meet early (day one) to review objectives
– Determine student’s knowledge, skill level, previous experience (portfolio)
– Review goals (preceptor, program, student)
– Describe feedback/evaluation process
A: Assess
– Observe student in rotation activities
– Record observations frequently
– Provide Timely, Specific Feedback routinely to student
– Include Positives & Negatives
– Include Program Coordinator if needed
– Ask student to self-assess
D: Discuss assessment
– Set Formal Meeting
– Preceptor & Student fill out evaluation form in advance
– Compare evaluations together; rectify differences
– “Formative” feedback: agree upon plan for continuation and improvement
E: End with a Grade
– Schedule formal meeting
– Complete evaluation in advance
– Support evaluation with documentation
– Highlight items to work on in future
– “Summative” grade

Figure 4 shows the GRADE strategy
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT editor-in-chief@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
Case studies to be discussed
Case Study #1:
Lack of Knowledge/Application
• Student is assigned to your advanced pharmacy practice ambulatory care rotation; it is the first APPE rotation of the year and the student has no previous work experience except for 4-week IPPE in community setting.
• During the first week, the student does not know routinely used “top 280” drugs, doses, indications. Student lacks confidence in counseling, and shies away from it. When directly requested to counsel a patient, student did so with great difficulty; you witness several errors in the counseling and step in to correct for the patient. Student is unable to demonstrate use of MDI for asthmatic patient.
• What are your options as primary preceptor??
Case #1: Remediation Options
• Repeat similar rotation experience
• Review certain therapeutics areas (class notes, textbooks, case studies)
• Work (part-time) in pharmacy practice setting
• Read, read, read
• Refer to college counseling for time management skills
Case Study #2: Communications
• A student with previous hospital experience is assigned to your hospital rotation, in which she will be assigned to work with many pharmacists within the facility.
• Several pharmacists report to you that the student basically refuses to follow your hospital policy, citing that it is “all wrong” and that Hospital X teaches us to do it a more efficient way. You are aware of Hospital X’s policies, and have purposefully selected your own methods for your own reasons. The student continues to ruffle feathers of your staff.
• What are your options?
Case #2: Remediation options
• Refer to college counseling for appropriate services (depression, anxiety, coping, time management, eating disorders, etc.)
3.8.4 Case #3: Professionalism
• Student is on your hospital rotation and is overheard by several of the pharmacy staff in the break room as saying that this rotation is “useless –I am counting the days” and “my preceptor is the worst I’ve ever had”. This information is reported to you.
• The nurses on the two units report that your student has been rude in trying to obtain patient charts on their floors.
• What are your options as preceptor?
Case #3: Preceptor Options
• Call the College Experiential Personnel
• Document in writing the specific shortcomings (specific examples of lack of professionalism), and provide this feedback to student promptly
• Devise plan for improvement with specific timeline: by Friday, I expect…
• Provide frequent feedback informally and formally (“midpoint” – can do multiple evals)
• Recognize that it is possible this student will not change his/her ways and will not be able to continue at your site because of inability to behave in a professional manner.
Case #3: remediation options
• Assign student to write paper on professionalism, after researching topic.
CONCLUSION
Communication in various forms is turning into extra important within the evolving technology of pharmacy. The preceptors have a sizeable possibility to strategically include communications training into the advanced pharmacy exercise experience. To make sure the improvement of conversation capabilities in pharmacy college students, preceptors can contain the teaching manner “see one, do one, teach one” into their activities, via following these strategies, preceptors can correctly & definitely effect the verbal exchange talents in their college students.
“Effective precepting bridges the gap of education and practice, knowledge and experience”.
REFERENCES
1. Randy P et al., Improving Communication Skills of Pharmacy Students through Effective Precepting. American Journal of Pharmaceutical Education 2006; 70 (3): 1-12.
2. Davis NM, Cohen MR. Counseling reduces dispensing accidents. Am Pharm. 1992; NS32:22.
3. Herrier RN, Boyce RW. Communicating risk to patients. Am Pharm. 1995; NS35:12-4.
4. Zillich AJ, McDonough RP, Carter BL, Doucette WR. Influential characteristics of physician/pharmacist collaborative relationships. Ann Pharmacother. 2004; 38:764-70.
5. www.nyschp.org/associations/8780/files/Preceptor%20Primer.ppt
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT editor-in-chief@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE









