 About Author:
About Author:
Kambham venkateswarlu
Graduate student
Sri Lakshmi Narasimha College of Pharmacy, Palluru,
Chittoor District, Andhra Pradesh-517132, India.
k.v.reddy9441701016@gmail.com
ABSTRACT:
Brugada syndrome is a genetic cause of sudden cardiac arrest characterized by abnormal electrocardiographic (ECG) pattern in the right precordial leads either at rest or after provocation. In this condition, sudden death may occur due to polymorphic ventricular tachycardia or ventricular fibrillation. In approximately 30% of patients, sudden cardiac arrest is the initial clinical manifestation of Brugada syndrome.
Brugada syndrome (BrS) is a genetic cause of sudden cardiac arrest (SCA). In this condition, SCA occurs due to the development of either polymorphic ventricular tachycardia (VT) or ventricular fibrillation (VF). In approximately 30% of patients, SCA is the initial clinical manifestation of BrS. When VT or VF occurs, it tends to be in the evening hours. This is thought to occur because of circadian rhythm. Patients with BrS do not have structural heart disease on echocardiogram, stress testing, or cardiac catheterization. However, a standard electrocardiogram (ECG) usually shows the characteristic abnormality.
[adsense:336x280:8701650588]
Reference Id: PHARMATUTOR-ART-1604
INTRODUCTION:
The syndrome of right bundle branch block, persistent ST segment elevation and sudden death was described in 1992 as a new entity causing unexpected sudden cardiac death (SCD). The original description of eight patients was followed by case reports and subsequently by numerous publications focusing on the clinical characteristics of greater populations of patients, and publications defining the genetic, molecular and cellular aspects of this disease that became known as Brugada syndrome. The number of scientific publications dealing with the syndrome has increased substantially in the last years, and continues to do so , reaching an average of 20 publications per month in the first semester of 2009. The description of this syndrome became one of the landmarks in the integration of cardiology, rhythmology, electrophysiology, genetics, epidemiology and many other medical disciplines in the fight against cardiac diseases, and in particular sudden unexpected cardiac death in the young. This paper reviews the past and current knowledge concerning the clinical, genetic and molecular features of Brugada syndrome.
What is Brugada syndrome?
This is an inherited arrhythmia that causes the bottom chambers of the heart (the ventricles) to beat so fast that they can prevent the blood from circulating efficiently in the body. When this situation occurs (called ventricular fibrillation), the individual will faint and may die in a few minutes if the heart is not reset. While this is a disease that usually affects people in their 30's, it has actually been described at all ages. So it is important to screen everybody in a family. Not everybody who has the disease will have arrhythmias. However, we cannot know yet who will be OK and who will have problems. If you have had fainting spells related to Brugada syndrome, our experience indicates that you are at very high risk of having them again.
[adsense:468x15:2204050025]
How common is Brugada syndrome?
It is very difficult to know because it was only described 10 years ago. It is found all over the world and in some countries in Asia is the most common cause of death in young people after car accidents.
Is there any medication for Brugada syndrome?
Not yet. Brugada syndrome was discovered 10 years ago, and there is no medication to prevent the black outs yet.
Is there anything that resets the heart when it beats too fast?
Yes, there is a special pacemaker, called defibrillator, that when used in patients that have Brugada syndrome and black outs, jump-starts the heart every time it malfunctions. All the patients who have a defibrillator are doing well.
If one of my parents or siblings has Brugada syndrome what do I need to do:
Brugada syndrome may be inherited, that means passed from parents to children. So it is important that you follow some important steps:
· Contact your physician who will probably perform a physical exam and an electrocardiogram. Brugada syndrome can be seen in few occasions right away in the electrocardiogram, but sometimes, to see it, it requires the infusion of a medication.
· If the electrocardiogram shows Brugada syndrome or if you had some signs that your heart malfunctions, like loss of consciousness, fainting, passing out, your physician may advise you to undergo an EP test. This is a test that checks your heart's electrical activity and whether there is any malfunction.
· Because Brugada syndrome is inherited, the physician may request that you give a blood sample to perform genetic analysis in you and your family.
Talking to your physician is the first thing to do and he will advise you.
DIAGNOSIS:
The diagnosis of the syndrome is easily obtained by electrocardiography as long as the patient presents the typical electrocardiographic pattern and there is a history of aborted sudden death or syncope caused by a polymorphic ventricular tachycardia. It is difficult to forget such a typical electrocardiogram. The ST segment elevation in V1 to V3 with the right bundle branch block pattern is characteristic. The ST changes are different from the ones observed in acute septal ischemia, pericarditis, and ventricular aneurysm and in some normal variants like early repolarization. There are though, electrocardiograms which are not as characteristic (picture 6), and they are only recognized by a physician who is thinking of the syndrome. There are also many patients with a normal electrocardiogram in whom the syndrome can only be recognized a posteriori when the typical pattern appears in a follow-up electrocardiogram or after the administration of ajmaline, procainamide or flecainide (picture 2).
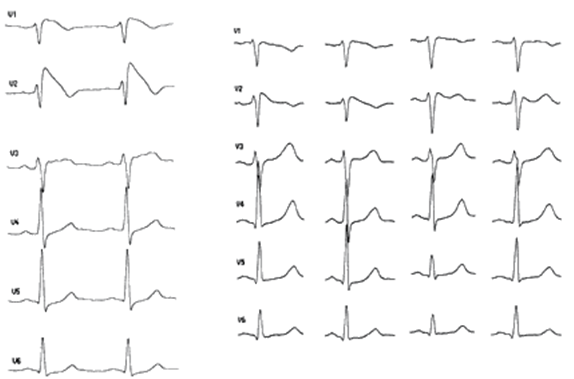
Fig: 1
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
Six precordial leads showing spontaneous changes of the electrocardiogram in five different days. Note that the panel in the right shows a less typical electrocardiogram. This pattern has been called saddle-back by the Japanese investigators.
It is possible that the electrocardiographic patterns are different depending on the genetic abnormality. This is the case in other genetic diseases like the long QT syndrome. The mutations that have been discovered in two families give proof of this fact: their electrocardiograms are similar, but not identical (picture 8). Even though in both cases the affected gene was the same, the exact mutation was different. It will be necessary to identify more mutations and make close genotype-phenotype correlation to establish the links. However, we cannot forget the great variability of the electrocardiogram in this syndrome, something which will certainly not facilitate analysis.
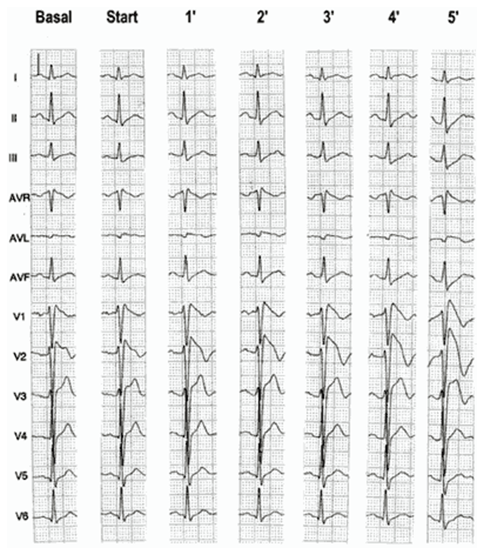
Fig: 2
12-lead ECG during administration of ajmaline (50 mg in 5 min). Note the progressive appearance of the ST elevation in V1-V3.
Additional diagnostic problems are caused by the changes in the electrocardiogram induced by the autonomous system and by antiarrhythmic drugs. The study by Miyazaki et al was the first one to show the variability of the electrocardiographic pattern in the syndrome. Despite the fact that the syndrome was initially described as a persistent electrocardiographic pattern, it was soon recognized that the electrocardiogram is variable over time, depending on the autonomic interaction and the administration of antiarrhythmic drugs. Adrenergic stimulation decreases the ST segment elevation, while vagal stimulation worsens it. The administration of class Ia, Ic and III drugs increases the ST segment elevation, and also fever. Exercise decreases ST segment elevation in some patients but increases it in others (after exercise when the body temperature has risen). The changes in heart rate induced by atrial pacing are accompanied by changes in the degree of ST segment elevation. When the heart rate decreases, the ST segment elevation increases and when the heart rate increases the ST segment elevation decreases. However, the contrary can also be observed.
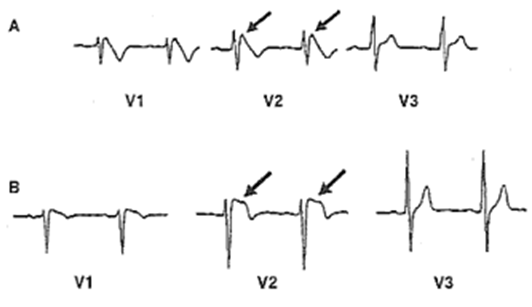
Fig: 3
Leads V1 to V3 are shown from two patients with two different mutations in the sodium channel. It is possible that the electrocardiogram varies depending upon the type of mutation.
Patients with syncope of unknown cause must be challenged with antiarrhythmic drugs in order to exclude the possibility of this syndrome as a cause of ventricular arrhythmias and syncope.
ORIGIN OF THE ELECTROCARDIOGRAM AND VENTRICULAR ARRHYTHMIAS:
It is unclear whether the right bundle branch block in this syndrome is real or whether it represents an early repolarization of right ventricular epicardium. The clinical and electrophysiologic data suggest that both possibilities exist. Some electrocardiograms clearly show a right bundle branch block after normalization of the ST segment (picture 9, panel C). There is frequently a prolongation of the H-V interval in these patients, which supports an abnormality of the conduction system. On the other hand, we can find electrocardiograms without right bundle branch block after normalization of the ST segment elevation (picture 10). Moreover, not all the patients have a prolongation of the H-V interval.
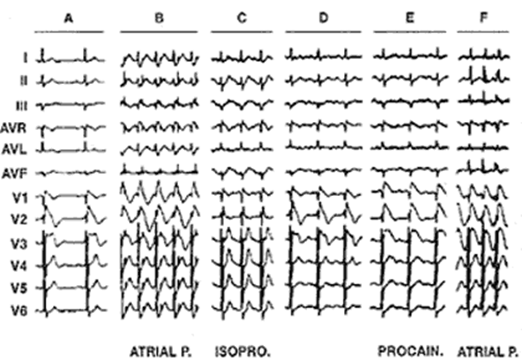
Fig: 4
Modulation of the electrocardiogram by atrial pacing, isoproterenol and procainamide. Note the right bundle branch block in panel the third panel (ISOPRO) after the ST elevation has been normalized by isoproterenol.
Approximately 10% of patients with this syndrome suffer from paroxysmal atrial fibrillation. It is possible that similar genetic defects alter atrial and ventricular electrophysiology in some patients.
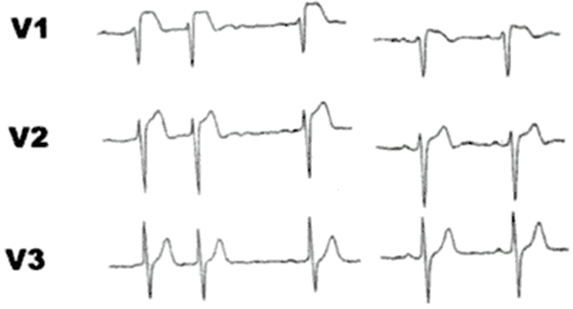
Fig: 5
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
In contrast to picture 9, this patient shows no right bundle branch block when the electrocardiogram normalizes during followup.
The polymorphic ventricular tachycardia can be often reproduced by programmed electrical stimulation of the heart in these patients, suggesting a re-entrant mechanism. Phase 2 re-entry is believed to undelie ventricular arrhythmias in this syndrome.
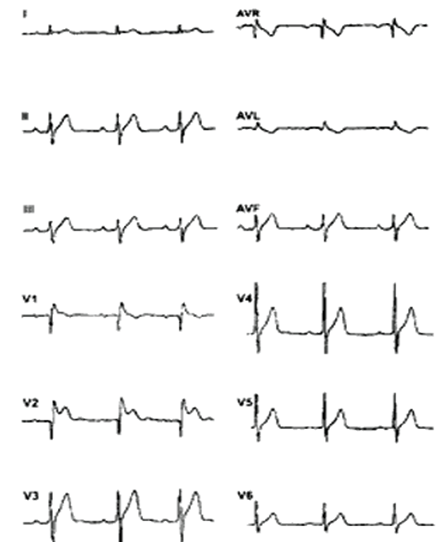
Fig: 6
RELATION WITH OTHER SYNDROMES:
There exist a lot of concern about a possible relation between the syndrome under discussion and other syndromes, particularly right ventricular dysplasia. The recent discovery of the genetic abnormalities of Brugada syndrome in the gene SCN5A located in chromosome 3 should be sufficient to finish this discussion, because the loci so far described in right ventricular dysplasia are located in other chromosomes.
In spite of these considerations, of course it is perfectly possible that some patients manifest two different diseases at the same time, and also there exists electrocardiograms that look similar to Brugada syndrome, but are not caused by the disease (pseudo-Brugada syndrome). Ikeguchi and co-workers (personal communication) have studied a patient with Wolff-Parkinson-White syndrome who was successfully treated by means of radiofrequency catheter ablation. The patient died suddenly two years after ablation. Analysis of the electrocardiograms of this case shows that he also suffered from Brugada syndrome. Thus, he had two syndromes at the same time. It is not unthinkable, therefore, that some patients may suffer from right ventricular dysplasia and Brugada syndrome simultaneously.
Other diseases may result in electrocardiographic manifestations similar to Brugada syndrome. For instance, it is interesting to observe the pictures published from Buenos Aires in 1982 (picture 14). In patients with Chagas' disease Chiale et al. showed that the intravenous administration of ajmaline was of value to uncover latent conduction disturbances, but also what they called "latent disease". In patients with positive serology severe conduction disturbances occurred in one third after the administration of intravenous ajmaline. In 8% of patients they observed the appearance of ventricular arrhythmias and in 7% elevation of the ST segment in the right precordial leads (picture 14). The question arises of the relation between Chagas' disease and Brugada syndrome in these patients. Chiale and co-workers actually considered the ajmaline challenge as a non-specific test capable of detecting myocardial damage. On the light of the recent discovery of the genetic defect underlying Brugada syndrome, the question also arises about the possible occurrence of damage to the sodium channel by Chagas' disease. Although there exist major differences between Chagas' disease and Brugada syndrome, the final common pathway leading to sudden death may be the same: damage to the sodium channel (infectious and inmunologic in Chagas' disease, genetic in Brugada syndrome) with conduction and repolarisation disturbances leading to electrical chaos and ventricular fibrillation.
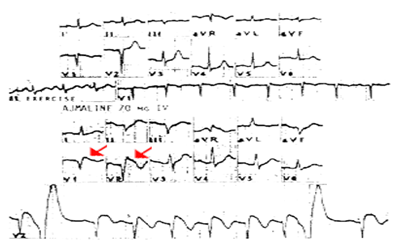
Fig: 7
Effects of ajmaline in a patient with Chagas' disease. Ajmaline produces ST segment elevation in the right precordial leads (arrows). It is not clear whether this patient suffered from two diseases at the same time or whether Chagas' disease causes the same abnormalities as Brugada.
Other conditions may result in electrocardiograms simulating Brugada syndrome: Steinert's disease (picture 15), pectus excavatum, and mediastinal tumors (Farre J). These should be excluded before diagnosing Brugada syndrome.
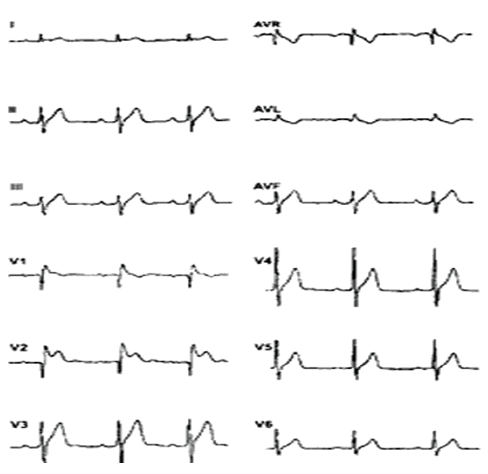
Fig: 8
Electrocardiogram of a patient with Steinert's disease.Some disease may result in electrocardiographic patterns resembling Brugada syndrome. However, the differences are usually evident,both clinically and electrocardiographically. On this electrocardiogram we do not observe the typical ST segment elevation in leads V1 to V3 although the right bundle branch block is evident.
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
EFFECTS OF CHANGESIN HEART RATE AND EXERCISE:
As already discussed in part, this syndrome is characterized by a great variability in the electrocardiographic pattern. The electrocardiogram may be completely abnormal at times, but completely normal at others. This variability has many causes and several explanations. Autonomic changes and body temperature influence the electrocardiogram. So do spontaneous or induced changes in heart rate. An artificial increase in heart rate (by atrial pacing) decreases ST segment elevation, while a decrease in heart rate increases it. These data are again in agreement with the loss of the dome of the action potential at epicardial level as the cause of ST segment elevation. Ito becomes more prominent at slow rates increasing heterogeneity and ST segment elevation. These data are also in agreement with the clinical observations documenting a bradycardia -dependency and a higher incidence of sudden death during sleep in patients with this syndrome.
Normalization of the ST segment during exercise is the most common finding in patients with this syndrome. These are logical findings because both an increase in heart rate and adrenergic stimulation decrease ST segment elevation.
CONCLUSION:
Brugada syndrome registry has allowed recognition of very low risk patients with the syndrome
* Asymptomatic
* Basal normal ECG
* Non-inducible
REFERENCES:
1. Extramiana F, Seitz J, Maison-Blanche P, et al. Quantitative assessment of ST segment elevation in Brugada patients. Heart Rhythm. 2006; 3: 1175-1181.
2. Tatsumi H, Takagi M, Nakagawa E, Yamashita H, Yoshiyama M. Risk stratification in patients with Brugada syndrome: analysis of daily fluctuations in 12-lead electrocardiogram (ECG) and signal-averaged electrocardiogram (SAECG). J Cardiovasc Electrophysiol. 2006; 17: 705-711.
3. Mizumaki K, Fujiki A, Tsuneda T, et al. Vagal activity modulates spontaneous augmentation of ST elevation in the daily life of patients with Brugada syndrome. J Cardiovasc Electrophysiol. 2004; 15: 667-673.
4. Shimizu W. Gender difference and drug challenge in Brugada syndrome. J Cardiovasc Electrophysiol. 2004; 15: 70-71.
5. Gonzalez Rebollo JM, Hernandez MA, Garcia A, Garcia de CA, Mejias A, Moro C. [Recurrent ventricular fibrillation during a febrile illness in a patient with the Brugada syndrome]. Rev Esp Cardiol. 2000; 53: 755-757. Spanish.
6. Porres JM, Brugada J, Urbistondo V, Garcia F, Reviejo K, Marco P. Fever unmasking the Brugada syndrome. Pacing Clin Electrophysiol. 2002; 25: 1646-1648.
7. Pitzalis MV, Anaclerio M, Iacoviello M, et al. QT-interval prolongation in right precordial leads: an additional electrocardiographic hallmark of Brugada syndrome. J Am Coll Cardiol. 2003; 42: 1632-1637.
8. Castro Hevia J, Antzelevitch C, Tornes Bárzaga F, et al. Tpeak- Tend and Tpeak-Tend dispersion as risk factors for ventricular tachycardia/ ventricular fibrillation in patients with the Brugada syndrome. J Am Coll Cardiol. 2006; 47: 1828-1834.
9. Babai Bigi MA, Aslani A, Shahrzad S. aVR sign as a risk factor for life-threatening arrhythmic events in patients with Brugada syndrome. Heart Rhythm. 2007; 4: 1009-1012.
10. Fish JM, Antzelevitch C. Cellular mechanism and arrhythmogenic potential of T-wave alternans in the Brugada syndrome. J Cardiovasc Electrophysiol. 2008; 19: 301-308.
11. Tada T, Kusano KF, Nagase S, et al. The relationship between the magnitude of T wave alternans and amplitude of the corresponding T Wave in patients with Brugada syndrome. J Cardiovasc Electrophysiol. 2008; 19: 56-61.
12. Kyndt F, Probst V, Potet F, et al. Novel SCN5A mutation leading either to isolated cardiac conduction defect or Brugada syndrome in a large French family. Circulation. 2001; 104: 3081- 3086.
13. Smits JP, Eckardt L, Probst V, et al. Genotype-phenotype relationship in Brugada syndrome: electrocardiographic features differentiate SCN5A-related patients from non-SCN5A-related patients. J Am Coll Cardiol. 2002; 40: 350-356.
14. Yokokawa M, Noda T, Okamura H, et al. Comparison of long-term follow-up of electrocardiographic features in Brugada syndrome between the SCN5A-positive probands and the SCN5A-negative probands. Am J Cardiol. 2007; 100: 649- 655.
15. Junttila MJ, Brugada P, Hong K, et al. Differences in 12-lead electrocardiogram between symptomatic and asymptomatic Brugada syndrome patients. J Cardiovasc Electrophysiol. 2008; 19: 380-383.
16. Extramiana F, Seitz J, Maison-Blanche P, et al. Quantitative assessment of ST segment elevation in Brugada patients. Heart Rhythm. 2006; 3: 1175-1181.
17. Tatsumi H, Takagi M, Nakagawa E, Yamashita H, Yoshiyama M. Risk stratification in patients with Brugada syndrome: analysis of daily fluctuations in 12-lead electrocardiogram (ECG) and signal-averaged electrocardiogram (SAECG). J Cardiovasc Electrophysiol. 2006; 17: 705-711.
18. Mizumaki K, Fujiki A, Tsuneda T, et al. Vagal activity modulates spontaneous augmentation of ST elevation in the daily life of patients with Brugada syndrome. J Cardiovasc Electrophysiol. 2004; 15: 667-673.
19. Shimizu W. Gender difference and drug challenge in Brugada syndrome. J Cardiovasc Electrophysiol. 2004; 15: 70-71.
20. Gonzalez Rebollo JM, Hernandez MA, Garcia A, Garcia de CA, Mejias A, Moro C. [Recurrent ventricular fibrillation during a febrile illness in a patient with the Brugada syndrome]. Rev Esp Cardiol. 2000; 53: 755-757. Spanish.
21. Porres JM, Brugada J, Urbistondo V, Garcia F, Reviejo K, Marco P. Fever unmasking the Brugada syndrome. Pacing Clin Electrophysiol. 2002; 25: 1646-1648.
22. Pitzalis MV, Anaclerio M, Iacoviello M, et al. QT-interval prolongation in right precordial leads: an additional electrocardiographic hallmark of Brugada syndrome. J Am Coll Cardiol. 2003; 42: 1632-1637.
23. Castro Hevia J, Antzelevitch C, Tornes Bárzaga F, et al. Tpeak- Tend and Tpeak-Tend dispersion as risk factors for ventricular tachycardia/ ventricular fibrillation in patients with the Brugada syndrome. J Am Coll Cardiol. 2006; 47: 1828-1834.
24. Babai Bigi MA, Aslani A, Shahrzad S. aVR sign as a risk factor for life-threatening arrhythmic events in patients with Brugada syndrome. Heart Rhythm. 2007; 4: 1009-1012.
25. Fish JM, Antzelevitch C. Cellular mechanism and arrhythmogenic potential of T-wave alternans in the Brugada syndrome. J Cardiovasc Electrophysiol. 2008; 19: 301-308.
26. Tada T, Kusano KF, Nagase S, et al. The relationship between the magnitude of T wave alternans and amplitude of the corresponding T Wave in patients with Brugada syndrome. J Cardiovasc Electrophysiol. 2008; 19: 56-61.
27. Kyndt F, Probst V, Potet F, et al. Novel SCN5A mutation leading either to isolated cardiac conduction defect or Brugada syndrome in a large French family. Circulation. 2001; 104: 3081- 3086.
28. Smits JP, Eckardt L, Probst V, et al. Genotype-phenotype relationship in Brugada syndrome: electrocardiographic features differentiate SCN5A-related patients from non-SCN5A-related patients. J Am Coll Cardiol. 2002; 40: 350-356.
29. Yokokawa M, Noda T, Okamura H, et al. Comparison of long-term follow-up of electrocardiographic features in Brugada syndrome between the SCN5A-positive probands and the SCN5A-negative probands. Am J Cardiol. 2007; 100: 649- 655.
30. Junttila MJ, Brugada P, Hong K, et al. Differences in 12-lead electrocardiogram between symptomatic and asymptomatic Brugada syndrome patients. J Cardiovasc Electrophysiol. 2008; 19: 380-383.
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE









