{ DOWNLOAD AS PDF }
About Authors:
M. Manasa Rekha,
Department of Pharmacy Practice,
Annamacharya college of Pharmacy,
Rajampet, Andhra Pradesh, India.
manasarekharoyal@gmail.com
ABSTRACT
Clinical pharmacy is the branch of pharmacy in which pharmacists provide patient care that optimizes the use of medication and promotes health, wellness, and disease prevention. Clinical pharmacists care for patients in all health care settings but the clinical pharmacy movement initially began inside hospitals and clinics. Clinical pharmacists often work in collaboration with physicians, nurse practitioners and other healthcare professionals. The Clinical Pharmacist Stating explicitly that the clinical pharmacist cares for patients in all health care settings emphasizes two points: that clinical pharmacists provide care to their patients and that this practice can occur in any practice setting. The clinical pharmacist’s application of evidence and evolving sciences points out that clinical pharmacy is a scientifically rooted discipline the application of legal, ethical, social, cultural, and economic principles serves to remind us that clinical pharmacy practice also takes into account societal factors that extend beyond science.
[adsense:336x280:8701650588]
REFERENCE ID: PHARMATUTOR-ART-2504
|
PharmaTutor (Print-ISSN: 2394 - 6679; e-ISSN: 2347 - 7881) Volume 5, Issue 7 Received On: 17/03/2017; Accepted On: 01/04/2017; Published On: 01/07/2017 How to cite this article: Rekha MM, Manasa M;A study on role of doctor of pharmacy in identification and reporting of adverse drug reactions in an antiretroviral therapy ward of a teritary care teaching hospital; PharmaTutor; 2017; 5(7); 33-42 |
INTRODUCTION
Clinical pharmacy is the branch of pharmacy in which pharmacists provide patient care that optimizes the use of medication and promotes health, wellness, and disease prevention. Clinical pharmacists care for patients in all health care settings but the clinical pharmacy movement initially began inside hospitals and clinics. Clinical pharmacists often work in collaboration with physicians, nurse practitioners and other healthcare professionals. The Clinical Pharmacist Stating explicitly that the clinical pharmacist cares for patients in all health care settings emphasizes two points: that clinical pharmacists provide care to their patients and that this practice can occur in any practice setting. The clinical pharmacist’s application of evidence and evolving sciences points out that clinical pharmacy is a scientifically rooted discipline the application of legal, ethical, social, cultural, and economic principles serves to remind us that clinical pharmacy practice also takes into account societal factors that extend beyond science.
Adverse Drug Reaction
However according to World Healthcare Organization (WHO) adverse drug reaction (ADR) can be defined as "any response to a drug which is noxious and unintended, and which occurs at doses normally used in man for prophylaxis, diagnosis, or therapy of disease, or for the modification of physiological function."
Adverse Drug Events
The drugs being intensive in physiological/pharmacological actions are capable of causing an injury in some suitable patients in the usual course of treatment and may not happen on all patients like ADRs. Adverse drug events are injuries resulting from the medical management. It can occur in any health care setting, including: inpatient, outpatient and long-term care settings.
Side Effects
Side effects are due to pharmacological interactions with living system in general.The drugs are usually administered to the whole of the body making pharmacological reactions to happen.
Pharmacovigilance
Pharmacovigilance (PV) is defined as the science and activities relating to the detection, assessment, understanding and prevention of adverse effects or any other drug-related problem. WHO established its Programme for International Drug Monitoring in response to the thalidomide disaster detected in 1961.
Aims Of Pharmacovigilance Program
The aim of the pharmacovigilance is to gather evidence and establish the sever ADR resulting from using of drugs for example the drug Nimesulide was approved by regulatory agencies as safe medication for use in management of RA and Analgesics.
Classification of Adverse Drug Reactions
According to Rawlins ADRs can be classified into Type A and Type B. Type A ADRs are dose dependent and predictable from the known pharmacology of the drug. Whereas Type B reactions are not dose dependent and unpredictable. The classification has gradually been extended to Type A-F. Type A: Augmented pharmacologic effects, Type B: Bizarre effects (or idiosyncratic), Type C: Chemical effects, Type D: Delayed effects, Type E: End-of-treatment effects, and Type F: Failure of therapy.
Adverse Drug Reactions Are Needed To Be Monitored
The ADRs effect may have a consequence extending to future human generation by changing the genetic properties.The ADRs are of no use for therapeutic purpose.However the ADR monitoring can give an insight into other possible applications and drug development leading to new drug discovery.The off-label use of medicines can be a useful hint for extending the drug use after getting the approval for the off-label use by regulatory authorities.
Who Can Report The Adverse Drug Reactions
As per the pharmacovigilance program all Health professionals working in the field of delivering the health care (both conventional and unconventional) like physicians, dentists, nurses, pharmacists, can report suspected adverse drug reactions by letter, phone, fax, e-mail, or by personal contact to any of the five adverse drug reaction monitoring centers located across the country.
Whom to Report the Adverse Drug Reactions
The ADRs are of public interest and there is a system of collection, documenting and reporting. The matters of ADRs are of detrimental for a pharmaceutical industry prospect of marketing. Hence an independent public funded national and international pharmacovigilance centers are established.These centers receive the reports of ADRs in format designed by the pharmacovigilance Program. A method for assigning the probability of a reported or suspected ADR (e.g., confirmed or definite, likely, possible, and unlikely) should be developed to categorize each ADR.subjective questions and the professional judgment of a Pharmacist[46] can be used as additional tools to determine the probability of an ADR.
Questions might include the following:
a. Was there a temporal relationship between the onset of drug therapy and the adverse reaction?
b. Was there a dechallenge; i.e., did the signs and symptoms of the adverse reaction subside when the drug was withdrawn?
c. Can signs and symptoms of the adverse reaction be explained by the patient’s disease state?
d. Were there any laboratory tests that provide evidence for the reaction being an ADR?
e. What was the patient’s previous general experience with the drug?
f. Did symptoms return when the agent was readministered?
g.method for ranking ADRs by severity should be established.
h.description of each suspected ADR and the outcomes from the event should be documented in the patient’s medical record.
i.Serious or unexpected ADRs should be reported to the Food and Drug Administration (FDA) or the drug’s manufacturer (or both).a
j.All ADR reports should be reviewed and evaluated by a designated multidisciplinary committee (e.g., a pharmacy and therapeutics committee).
Scales to Assess the Adverse Drug Reactions
The adverse drug reaction scales are to establish a causal relationship between the drug and the adverse event. The Naranjo ADR probability scale, WHO- Uppsala Monitoring Centre causality categories and Severity of reported ADRs by Modified Hartwig and Siegel scale are used to assess the ADRs.
Scales used to report adverse drug reactions:
The causality assessment system proposed by the World Health Organization Collaborating Centre for International Drug Monitoring, the Uppsala Monitoring Centre (WHO–UMC), and the Naranjo Probability Scale are the generally accepted and most widely used methods for causality assessment in clinical practice as they offer a simple methodology. The above scales are structured, transparent, consistent, and easy to apply assessment methods.
“Naranjo ADR Probability Scale”.
The Naranjo adverse drug reaction (ADR) probability scale. The Naranjo criteria classify the probability that an adverse event is related to drug therapy based on a list of weighted questions, which examine factors such as the temporal association of drug administration and event occurrence, alternative causes for the event, drug levels, dose – response relationships and previous patient experience with the medication.
The ADR is assigned to a probability category from the total score as follows:
Definite if the overall score is 9 or greater, probable for a score of 5-8, possible for 1-4 and doubtful if the score is 0.
Table1.1: Naranjo ADR Probability Scale
|
The Naranjo adverse drug reaction probability scale; To assess the adverse drug reaction, please answer the following questionnaire and give the pertinent score |
Yes |
No |
Do not know |
Score |
|---|---|---|---|---|
|
1. Are there previous conclusive reports on this reaction?
2. Did the adverse event occur after the suspected drug was administered?
3. Did the adverse reaction improve when the drug was discontinued or a specific antagonist was administered?
4. Did the adverse reaction reappear when the drug was readministered?
5. Are there alternative causes (other than the drug) that could have on their own caused the reaction?
6. Did the reaction reappear when a placebo was given?
7. Was the blood detected in the blood (or other fluids) in concentrations known to be toxic?
8. Was the reaction more severe when the dose was increased or less severe when the dose was decreased?
9. Did the patient have a similar reaction to the same or similar drugs in any previous exposure?
10. Was the adverse event confirmed by any objective evidence?
|
+1
+2
+1
+2
-1
-1
+1
+1
+1
+1 |
0
-1
0
-1
+2
+1
0
0
0
0 |
0
0
0
0
0
0
0
0
0
0 |
|
|
|
|
|
Total |
|
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT editor-in-chief@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
Table 1.2 WHO–UMC causality categories
|
Causality term |
Assessment criteria (all points should be reasonably complied) |
|---|---|
|
Certain |
|
|
Probable/likely |
|
|
Possible |
|
|
Unlikely |
|
|
Conditional/unclassified |
|
|
Unassessable/unclassifiable |
|
Role of Pharmacist in Adverse Drug Reaction Monitoring
The pharmacist being in the field of clinical, community and hospital settings is likely to get to know about an ADR event the pharmacist are also considered as expert Professionals who are consulted for drug information about an ADR management. The Pharmacist are to participate in ADR reporting as a professional obligation and responsibility in the capacity of stakeholders for patient safety.
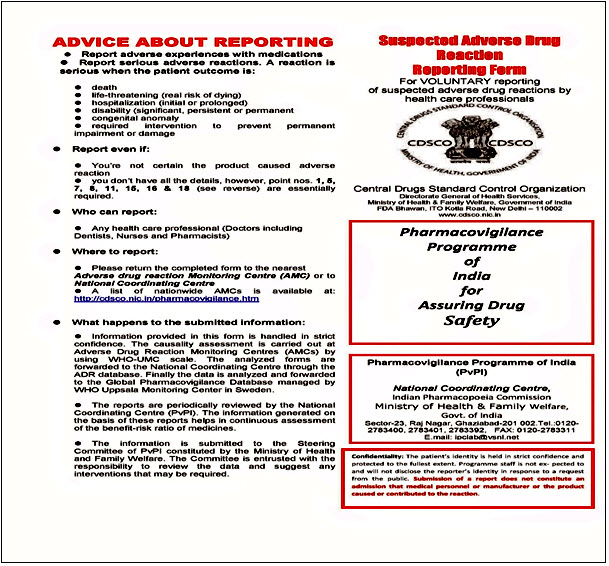
Figure1.1: suspected adverse drug reaction reporting form
Role of Uppsala Monitoring Centre In Adverse Drug Reactions Monitoring
The Uppsala Monitoring Centre is the global Pharmacovigilance center promoted by WHO. The Uppsala Monitoring Centre is the final destination for ADR reports which arrives from different countries and is reviewed for signals of ADRs. Uppsala Centre also conducts training programs and helps the establishment of country, regional and local ADR reporting centers. They also train human resources in the area of software applications for ADR monitoring.
Benefits Of Adverse Drug Reactions Monitoring
The ADR monitoring is a gate way to identify the risks due to use of drugs and also an opportunity to re-evaluate the risk-benefit analysis serving as updated guidelines for prescription writing.If ADR is sever than there can be a revival of licensing for the drug this becomes as a continuous engagement for the industry who is involved in sale of the drugs. There is a regulatory reform even in India to run, collect and submit periodical reports of Pharmacovigilance on selected products in order to continue with licensing of further sale of drug.
The Terminologies Used To Code The Adverse Drug Reactions
MedDRA is fully implemented in the WHO global safety database allowing entry and retrieval of information in either MedDRA or WHO- Adverse Reactions Terminology is used to code the ADRs. The structure of MedDRA is System organ class (SOC),High level group term (HLGT), High level term (HLT), Preferred term (PT) and Lowest level term (LLT).SOC is the highest level of the terminology, and distinguished by anatomical or physiological system, etiology, or purpose.HLGT is subordinate to SOC, Super ordinate descriptor for one or more HLTs. HLT is subordinate to HLGT, Super ordinate descriptor for one or more PTs.PT is represents a single medical concept.[66]
Seriousness And Severity
The American Food and Drug Administration defines a serious adverse event as one when the patient outcome is one of the following:[6]
• Death
• Life-threatening
• Hospitalization (initial or prolonged)
• Disability - significant, persistent, or permanent change, impairment, damage or disruption in the patient's body function/structure, physical activities or quality of life.
• Congenital anomaly
• Requires intervention to prevent permanent impairment or damage
• As research better explains the biochemistry of drug use, fewer ADRs are Type B and more are Type A.
Common mechanisms are:
Abnormal pharmacokinetics due to
• Genetic factors
• Comorbid disease states
• Synergistic effects between either a drug and a diseasetwo drugs
Abnormal pharmacokinetics
Comorbid disease states
Various diseases, especially those that cause renal or hepatic insufficiency, may alter drug metabolism. Resources are available that report changes in a drug's metabolism due to disease states.
Genetic factors
Abnormal drug metabolism may be due to inherited factors of either Phase I oxidation or Phase II conjugation. Pharmacogenomics is the study of the inherited basis for abnormal drug reactions.
Assessing causality
Causality assessment is used to determine the likelihood that a drug caused a suspected ADR. There are a number of different methods used to judge causation, including the Naranjo algorithm, the Venulet algorithm and the WHO causality term assessment criteria.Each have pros and cons associated with their use and most require some level of expert judgement to apply.
Monitoring bodies
• On an international level, the WHO runs the Uppsala Monitoring Centre, and the European Union runs the European Medicines Agency (EMEA).
• In the United States, the Food and Drug Administration (FDA) is responsible for monitoring post-marketing studies. In Canada, the Marketed Health Products Directorate of Health Canada is responsible for the surveillance of marketed health products.
• In Australia, the Therapeutic Goods Administration (TGA)conducts postmarket monitoring of therapeutic products.
PRESENT RESEARCH STUDY
AIM:
The study aims to assess the role of clinical pharmacist in identification and reporting of adverse drug reactions in antiretroviral therapy wards of a teritary care teaching hospital.
OBJECTIVES:
The Main Objective Of The Present Study Includes Preventing the medication related problems (ADVERSE DRUG REACTIONS),Monitoring of ADVERSE DRUG REACTIONS , Identifying and minimizing medication related problems, Improving Patient safety initiatives, Providing better therapy to the large number of patients, Improving the Patient health related outcomes.
METHODOLOGY:
Study Design: It is a Prospective observational study.
Study Period: The Present study was conducted for a period of 8 months from july 2016 to feburary 2017.
Study site : The Present study was conducted in ART Department at Rajiv Gandhi Institute of Medical Sciences ( RIMS), Kadapa.
Sample size: The Patients admitted in hospital during the study period of 8 months it was 100Patients.
Source of Data: All the patients satisfying the inclusion criteria were selected from ART department in Rajiv Gandhi institute of medical sciences (RIMS) Government Hospital, Kadapa. All the required data was collected from patients through Patient representative interview and case sheets and treatment charts.
Inclusion criteria
• Patients with aging above 18 years.
• Patients having previous history of medical, medication problems in ART.
• The Patients who are willing to participate in the study.
Exclusion criteria
• Patients who are not willing to Participate in the study.
RESULTS:
AGE WISE DISTRIBUTION OF MALE POPULATION:
In this study total of 100 patients were enrolled in the study. The males population is 55.The age wise male Patients population ranges from 2(3.6363) Patients were in the age group of 10-20 years , 27(49.09)Patients were in the age group of 20-30 years, 12(21.81) patients were in the age group of 30-40 years ,9(16.3636) patients were in the age group of 40-50 years ,5 (9.0909)Patients were in the age group of 50-60 years.
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT editor-in-chief@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
Table 1.1 Age wise distribution of male patients
|
Age in years |
Total number of Patients |
Percentage (%) |
|
10-20 |
2 |
3.6363 |
|
20-30 |
27 |
49.09 |
|
30-40 |
12 |
21.81 |
|
40-50 |
9 |
16.3636 |
|
50-60 |
5 |
9.0909 |
|
Total |
55 |
55 |
|
|
|
P value <0.0001 |
Fig 1.1 Age wise distribution of male patients


Fig 1.2 Age wise distribution of male patients showing percentage of distribution.
AGE WISE DISTRIBUTION OF FEMALE POPULATION:
In this study total of 100 patients were enrolled in the study. The Females population is 45.The age wise Female patients population ranges from the 0 Patients were in the age group of 10-20 and 16 (35.5) were from 20-30 years, 19(42.22) Patients were in the age group of 30-40 years and 5 (11.111)patients were in the age group of 40-50 years and 3(6.66)patients were in the age group of 50-60 years ,2(4.44) patients were in the age group of 60-70 years ,0 patients were in the age group of 70-80 years .
Table 1.2 Age wise distribution of Female Patients
|
Age |
Total |
Percentage (%) |
|
10-20 |
0 |
0 |
|
20-30 |
16 |
35.5 |
|
30-40 |
19 |
42.22 |
|
40-50 |
5 |
11.111 |
|
50-60 |
3 |
6.66666 |
|
60-70 |
2 |
4.444 |
|
70-80 |
0 |
0 |
|
Total |
45 |
45 |
|
|
|
P value <0.0001 |
Fig 1.3 Age wise distribution of Female patients.


Fig 1.4 Age wise distribution of Female patients showing percentage of distribution.
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT editor-in-chief@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
Table 1.3 Showing Medical Diagnosis Cases of HIV with other Comorbidities.
|
VARIOUS MEDICAL DIAGNOSIS CASES |
TOTAL |
|
HIV WITH HYPERTENSION AND DIABETES MELLITUS |
15 |
|
HIV WITH PNEUMONIA AND URINARY TRACT INFECTION |
11 |
|
HIV WITH TUBERCULOSIS |
16 |
|
HIV WITH TUBERCULOSIS AND LEPROSY |
11 |
|
HIV WITH SEPTICEMIA |
7 |
|
HIV WITH HYPERTENSION |
9 |
|
HIV WITH GROSS ANEMIA |
10 |
|
HIV WITH AGRANULOCYTOSIS |
13 |
|
HIV WITH ASTHMA AND COPD |
3 |
|
HIV WITH OTHER COMORBIDITIES |
5 |
|
Total Cases |
100 |
Table 1.4: TYPES AND NUMBER OF ADVERSE DRUG REACTIONS
|
Type of ADR |
Number ADRS |
Percentage (%) |
|
TYPE-A |
56 |
51.851851
|
|
TYPE-B |
46 |
42.59259
|
|
TYPE-C |
6 |
5.55 |
|
Total |
108 |
100 |

Figure 1.5 : Types Of ADRS And Their Distribution
DISCUSSION:
In this study total of 100 patients were enrolled in the study. The males population is 55.The age wise male Patients population ranges from 2(3.6363) Patients were in the age group of 10-20 years , 27(49.09)Patients were in the age group of 20-30 years, 12(21.81) patients were in the age group of 30-40 years ,9(16.3636) patients were in the age group of 40-50 years ,5 (9.0909)Patients were in the age group of 50-60 years. The Females population is 45.The age wise Female patients population ranges from the 0 Patients were in the age group of 10-20 and 16 (35.5) were from 20-30 years, 19(42.22) Patients were in the age group of 30-40 years and 5 (11.111)patients were in the age group of 40-50 years and 3(6.66)patients were in the age group of 50-60 years ,2(4.44) patients were in the age group of 60-70 years ,0 patients were in the age group of 70-80 years. A total 108 ADRS were screened during the study period. In which TYPE-A ADRS are 56(51.851851) , TYPE-B ADRS are 46 (42.59259) and TYPE-C ADRS are 6(5.55).
CONCLUSION:
The present study concludes that clinical pharmacist play a key role in patient safety, Particularly in ART department they are important for educating guiding the health care professionals related to safety use of medications. Even through drug related problems were founded but after reporting information to physicians we are minimizing harmful to Patient’s. In future clinical pharmacy services is one of the effective services in hospital to improve the quality of life of patient’s in the hospital. Implementing such a practices in the hospitals and country we can make the country and society becomes free of diseases.
REFERENCES:
1. *M. Manasa rekha ,A. Bharath kumar ---a prospective study on implementation of clinical pharmacy services to general medicine department in a teritary care teaching hospital published in journal of pharma research in ISSN: 2319-5622.
2. American College of Clinical Pharmacy. Pharmacotherapy 2008-28 (6), 816–817.
3. American College of Clinical Pharmacy.The Definition of Clinical Pharmacy. Pharmacotherapy 2008; 28(6):816-817.
4. Kucukarslan SN, Peters M, Mlynarek M, Nafziger DA. Dopharmacists’ presences on rounding teams reduce preventable adverse drug events in hospital general medical units.CMAJ 2004 Feb; 170(3):333.
5. Roberts MS , Stokes JA , King MA, Lynne TA, Purdie DM.Outcomes of a randomized controlled trial of a clinical pharmacy intervention in 52 nursing homes. Br J Clin Pharmacol 2001; 51:257-265.
6. Langebrake C, Hilgarth H. Clinical Pharmacist intervention in German University Hospital. Pharm World Sci 2010; 32:194-199.
7. srinivasan r, ramya g. Adverse drug reaction-causality assessment. international journal of research in pharmacy and chemistry.2011,1(3).
8. dr. rajaram, g., dr. sugirda, p. and dr. lenin, r.Pattern of adverse cutaneous drug reactions presenting to general practitioners in a semi urban area.asian journal of science and technology vol. 6, issue 09, pp. 1788-1790, september, 2015.
9. Jean F Kozak and Akber Mithani.Prevalence of Adverse Drug Events in Long Term Care: Variations in Screening Between Nurses and Physician-Pharmacist Reviewers. HSOA Journal of Gerontology & Geriatric Medicine.2015, 1: 007.
10. Ragesh G., Sindhubharathi A, Ushasri M, Srinivasulu A.A Study On Assessment Of Clinical Pharmacy Services To Cardiology Department In Tertiary Care Teaching Hospital.Int J Pharm Pharm Sci, Vol 6, Issue 2, 192-195.2015.
11. Satish Kumar BP, Prasanna Dhalal, Rajesh Venkataraman. Assessment of Clinical Pharmacist Intervention in Tertiary Care Teaching Hospital of southern India, Asian journal of pharmaceutical and clinical research.,6, 2013, 258-261.
12. Gairik sengupta et al.Adverse drug reaction monitoring in psychiatry out patient department of Indian teaching hospital.indian journal of practice.2011.
13. Mohamed N Al-Arifi, AY Mayet, Syed Wajid, M Al-Saadi.Knowledge,Attitude and Perception of Physicians towards Adverse Drug Reaction Reporting at King Khalid University Hospital, Riyadh, Saudi Arabia.Tropical Journal of Pharmaceutical Research May 2015; 14(5): 907-911.
14. Walli Mohammed,Dr. Samreen Afroz, Dr. Satish Miriyala,Dr. G. Ramya Naidu, Shardha Srikanth.World Journal Of Pharmaceutical Research.Vol 4, Issue 3, 2015..
15. Ashok Kumar.D,M.Venkata Subbaiah,M. Purushothaman.Evaluation Of Adverse Drug Reactions In A Tertiary Care Teaching Hospital.World Journal Of Pharmacy And Pharmaceutical Sciences.Vol 4, Issue 08, 2015.
16. Arvind Kumar Sharma, Dr. Rakesh Sonawane, Dr Nidhi Jain, Dr. Jayesh Rajgopal. Assessment of Adverse Drug Reactions reported to the regional Adverse Drug Reaction Monitoring Centre at a tertiary care teaching hospital in Bhopal.Indian joural of applied research.Volume : V, Issue : X, October – 2015.
17. N.Vanitha Rani, Rini Thoma,Rohini E,P. Soundararajan.A Study On Drug Related Problems In Chronic Kidney Disease Patients Of A Tertiary Care Teaching Hospital In South India.World Journal of Pharmaceutical Research.Vol 3, Issue 4, 2014.
18.Mahendra KumarBJ,SandeepA,BhimarayS Krishnagoudar,Katti Ravi Venkappa.Assessment and Evaluation of Drug Information Services provided by the Clinical Pharmcists in a rural tertiary care Teaching Hospital of South India.RGUHS Journal of Pharmaceutical Sciences. Apr-Jun, 2011/ Vol 1/ Issue 1.
19. Dimple Gohel1 ,Sandip Kumar Bhat.Evaluation of Dermatological Adverse Drug Reaction in the Outpatient Department of Dermatology at a Tertiary Care Hospital.Indian Journal of Pharmacy Practice, Vol 7, Issue 3, Jul–Sep, 2014.
20. Jose J, Rao P G. Pattern of adverse drug reactions notified by spontaneous reporting in an Indian tertiary care teaching hospital, PharmacolRes, 54(3), 2006, 226-33.
21. Lukshmy hettihewa.casualty assessment and the severity of the adverse drug reactions (adr) actively detected in hospital-in patients in tertiary care hospital sri lanka: prospective observational survey.Asian Journal of Research in Biological and Pharmaceutical Sciences. 2(1), 2014,1 - 10.
22. Pirmohamed M, James S, Meakin S, Green C,Scott A K, Walley T J.Adverse drug reactions as cause of admissions to hospital: prospective analysis of 18820 patients, BMJ, 329(7456),2004, 15-9.
23. Criegee-Rieck M, Neubert A, Egger T, Levy M.Implementation of a computer-assisted monitoring system for the detection of adverse drug reactions in gastrenteroloy, Ailment Pharmacol Ther, 19, 2004, 3039.
24. Satish kumar bassatti koppal puttegowda , santhosh yapamakula lakshminarayana and naveen assessing the pattern of drug information queries in a rural south indian tertiary care teaching hospital. malaysian journal of pharmaceutical sciences vol. 8, no. 2, 1–9 (2010).
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT editor-in-chief@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE









