About Authors:
AK Hafeez, MA Akheel, A Ashfaque, NK Meera
Dept of Pharmacy Practice,
VIPS,
Bangalore, India
Abstract
Aim: To study the prescribing pattern for the treatment of Dengue in tertiary care hospital in Bangalore.
Methods: A retrospective study was carried on prescribing pattern of drugs for the treatment of dengue in a tertiary care teaching hospital in Bangalore. This study included hundred patients both male and female in the age group of 1 – 70 years, the prescriptions were analysed for the drug therapy given.
Results:The results show that the most commonly prescribed class of drugs were antipyretic (99%), anti-ulcer (95%), antibiotics (69%) and anti emetic (40%). In addition, supplementary treatment was also observed. 100% of suffered population was treated with IV fluids. Since a specific treatment is not available for Dengue, the patients were treated symptomatically.
Conclusion:This survey highlights the demands for a more specific treatment, lest it leads to another epidemic break in the country.
[adsense:336x280:8701650588]
Referencs Id: PHARMATUTOR-ART-1191
Introduction
Dengue fever (DF) is an acute febrile viral disease frequently presenting with headaches, bone or joint and muscular pains, rash and leukopenia as symptoms. Dengue haemorrhagic fever (DHF) is characterized by four major clinical manifestations: high fever, haemorrhagic phenomena often with hepatomegaly and, in severe cases, signs of circulatory failure. Such patients may develop hypovolemic shock resulting from plasma leakage. This is called dengue shock syndrome (DSS) and can be fatal (1).
Dengue is the most rapidly spreading mosquito-borne viral disease in the world. In the last 50 years, incidence has increased 30-fold with increasing geographic expansion to new countries and, in the present decade, from urban to rural settings. An estimated 50 million dengue infections occur annually and approximately 2.5 billion people live in dengue endemic countries(2). Dengue has a wide spectrum of clinical presentations, often with unpredictable clinical evolution and outcome.(3).
Dengue virus, a member of the family flaviviridae, has four serologically related but genetically distinct virus serotypes, namely, Den-1, Den-2, Den-3 and Den-4. Dengue infection (DI) is presently the most important arboviral disease of mankind (4).
The origin of dengue viruses is uncertain. Whatever their origin, there has been an exponential diversification in dengue virus genotypes which has paralleled the increase in the human population over the last 200–300 years (5).The global epidemiology of dengue fever/dengue hemorrhagic fever (DF/DHF) is changing fast. Dengue infection has been known to be endemic in India for over two centuries as a benign and self limited disease. In recent years, the disease has changed its course manifesting in the severe form as DHF and with increasing frequency of outbreaks (6). At present, DI is endemic in over 100 countries worldwide and causes nearly 100 million cases of DF, 500,000 cases of DHF and 24,000 deaths each year(7).
Karnataka has the second highest number of dengue cases in the year 2010 in India up to August in India. According to the sources, the numbers of dengue cases are increasing in the state. While Karnataka reported 1,764 dengue cases with eight deaths in 2009, it recorded 1,338 with one death just from January to August 2010. (8)
The time between the bite of a mosquito carrying dengue virus and the start of symptoms averages 4 to 6 days, with a range of 3 to 14 days. An infected person cannot spread the infection to other persons but can be a source, or reservoir, of dengue virus for mosquitoes for about 6 days. Risk factors for dengue hemorrhagic fever include a person's age and immune status, as well as the type of infecting virus. Persons who were previously infected with one or more types of dengue virus are thought to be at greater risk for developing dengue hemorrhagic fever if infected again (9)
The standard treatment of dengue shock syndrome is to immediately administer intravenous fluids to expand plasma volume. Clinicians give blood if patients are bleeding. There are no drugs available specifically for the treatment of dengue haemorrhagic fever. Corticosteroids are used in some countries, particularly those in South-East Asia for managing dengue shock syndrome. They are thought to be effective for stabilizing capillary permeability and have been used in addition to fluid replacement (10).Dengue is been treated symptomatically.
[adsense:468x15:2204050025]
MATERIALS AND METHOD
A retrospective study was carried out on prescribing pattern of drugs in the treatment of dengue in Bangalore, Karnataka which was a highly prone to Dengue epidemic. The subjects of the study were infected males and females between the age group of 1-70 years. The study was carried out from June to October, 2010. The prescriptions and the relevant data were collected from the inpatients admitted to the Medicine and Paediatric department. The data were collected from the medical record department of a tertiary care hospital in Bangalore. 100 prescriptions with confirmed diagnosis of Dengue fever were collected and statistically analyzed.
RESULTS
The hospital records of 100 subjects of ages 1 to70 years admitted for treatment of Dengue were examined. Analysis of the data collected indicates that; more male (65%) than female (35%) were admitted for Dengue treatment (Fig 1). This gives a male to female ratio of 1.86:1. The age distribution were: 1 -18 year (paediatrics) = 29 (29.0%); 19-60 years (adult) = 60 (60.0%) above 60 years (geriatrics) = 3 (3.0%) (Fig 1, table1) the most affected age group being between 19-60 years. Average length of stay was 5.65 days. In our study out of 100 patients number of death was one with the condition of dengue fever with multiple organ dysfunctions. Diagnosis of Dengue was done by Dengue rapid test (DRT) or Ig G +, Ig M +, Ag+ or Dengue profile test.
|
Description |
No. |
|
Total no of cases |
100 |
|
Age |
|
|
Range |
1-70 |
|
Age group ( in years) |
|
|
1-18 (Paediatrics) |
29 |
|
19-60 (Adults) |
68 |
|
61 and above (Geriatrics) |
3 |
|
Sex |
|
|
Male |
65 |
|
Female |
35 |
|
Male: female ratio |
1.86:1 |
|
Length of stay (days) |
|
|
Range |
2 -11 |
|
Average stay |
5.65 |
Fig 1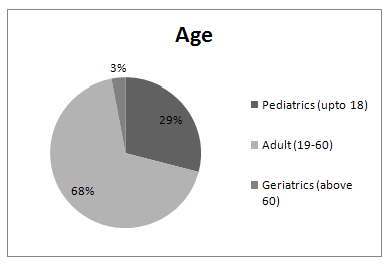
The most commonly used class of drugs were antipyretic (99%), anti-ulcer (95%), and antibiotics (69%) (Fig 2) and supplementary treatment was also given. The most commonly prescribed combination was antipyretic, anti ulcer, antibiotic and anti emetic drugs.
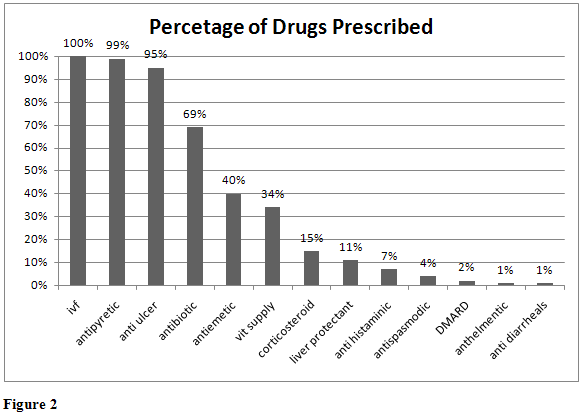
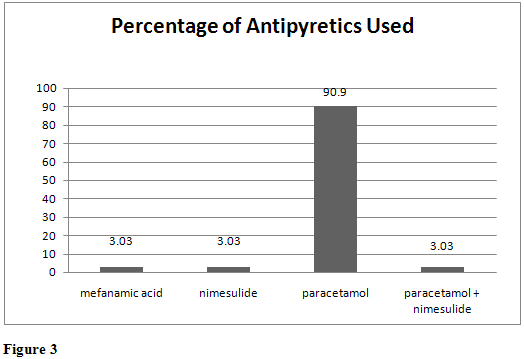
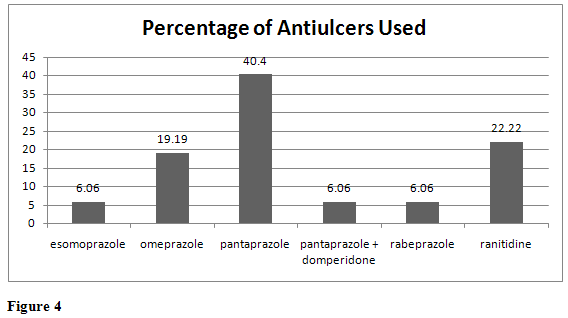
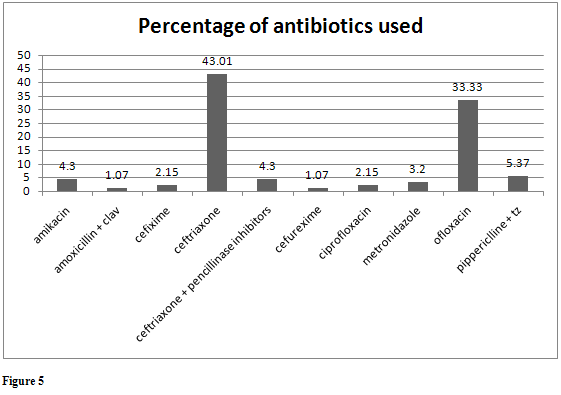
Among Antipyretics Paracetamol (90.9%), Mefanamic acid (3.03%), Nimesulide (3.03%) and combination of Paracetamol and Nimesulde (3.03%) were used (Fig 3). In Antiulcer Pantaprazole (40.4%), Ranitidine (22.22%), Omeprazole (19.19%), Esomoprazole (6.06%), Rabeprazole (6.06%) and combination of Pantaprazole and Domperidone (6.06%) were used (Fig 4). Among antibiotics Ceftriaxone(43.01%), Ofloxacin (33.33%), Pippericlline + Tazobactam (5.37%), Ceftriaxone + Pencillinase Inhibitors (4.3%), Amikacin(4.3%), Metronidazole (3.2%), Ciprofloxacin (2.15%), Cefixime (2.15%), Cefurexime(1.07%) and Amoxicillin + Clavalunic acid (1.07%) was prescribed (Fig 5). In Anti-emetics Ondansetron was used.
Supplementary treatment included anti emetics (40%), vitamin supplements (34%), corticosteroids (15%), liver protectants (11%), anti histmainics (7%), anti-spasmodics (4), DMAD (2), anthelmentics (1%) and anti diarrheal (1%) (Fig2). 100% of patients were treated with intravenous fluids. 42 % of the subjects were given transfusion during the hospitalization.
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
Discussion
There are no drugs available specifically for the treatment of Dengue fever and they are treated symptomatically. No effective vaccine or drug treatment for dengue fever is yet available, so management of the disease has relied on vector control measures, such as reduction of breeding sites and use of insecticides. Such measures have succeeded in eradicating mosquitoes in some regions, but have proved difficult to maintain in the long term. A drastic change in the outlook of the community and public health authorities with regard to hygiene and mosquito control measures is essential to stand a chance in the war against the mosquitoes
The search for dengue antivirals is a new endeavour that is gaining momentum due to both increased interest in dengue and substantial progress in the structural biology of dengue virus.
To develop a suitable health education strategy it is necessary to understand the level of knowledge and perceived risk of the community regarding mosquito-borne infectious diseases to determine what practices the people use to prevent mosquito bites at home, to determine media type and specific channels of communication for effective and efficient dissemination of information.In India, epidemics are becoming more frequent and are straining the limited resources of the public health system.
As Dengue fever has spread very rapidly in last few years in India, The need for the preventive treatment of Dengue can never be sidelined; however this might take several years to come till a vaccine or medicine is developed, thus the need arises to find a symptomatic treatment the can give the best results, to overcome the Dengue infection breaking into an epidemic again. Doctors and pharmacists along with the help of patients can work in unison to develop treatment that gives the best possible results. Similar surveys can help trigger research work related to specific treatments and prevent another outbreak of the epidemic.
Conclusion
The results show that the most commonly prescribed class of drugs were antipyretic (99%), anti-ulcer (95%), antibiotics (69%) and anti emetic (40%). In addition, supplementary treatment was also observed. Since the specific treatment is not available for Dengue and only patients were given symptomatic treatment, therefore it demands specific treatment.
References:
1. Dengue haemorrhagic fever. Diagnosis, treatment, prevention and control. Second edition. World health Organisation. Geneva 1997.
2. WHO. Dengue and dengue haemorrhagic fever. Factsheet No 117, revised May 2008. Geneva, World Health Organization, 2008 (who.int/mediacentre/ factsheets/fs117/en/).
3. Dengue: Guidelines for Diagnosis, Treatment, Prevention and Control. World Health Organization 2009. WHO/HTM/NTD/DEN/2009.1
4. World Health Organization. Prevention and control of dengue and dengue hemorrhagic fever: comprehensive guidelines. WHO Regional publication, SEARO 1999; 29.
5. Major Aaskov JG (2003). Infectious Diseases: Dengue. ADF Health 4: 66-71.
6. Gupta E, Dar L, Kapoor G, Broor S (2006). The changing epidemiology of dengue in Delhi, India. Virol J 3: 92.
7. Kumaria R (2010). Correlation of disease spectrum among four Dengue serotypes: a five years hospital based study from India. Braz J Infect Dis 14: 141-146.
8. Jayashree N, Senthalir S. State No.2 in dengue cases [Bangalore],Times of India, The, Sep 14, 2010.
9. USACHPPM, Readiness thru Health, Just the Facts, Dengue. Apr 2001. U.S. Army Center for Health Promotion and Preventive Medicine. 5158 Blackhawk Road, Aberdeen Proving Ground, MD 21010-5403 cdc.gov/ncidod/dvbid/arbor/arboinfo.htm
10. Panpanich R, Sornchai P, Kanjanaratanakorn K (2006). Corticosteroids for treating dengue shock syndrome. Cochrane Database of Systematic Reviews 3: 1-16.
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE









