About Author:
Anuradha Kaplish
M. Pharmacy (Drug discovery and drug development)
University Institute of Pharmaceutical Sciences, Panjab University,
Chandigarh-160014, India
1. INTRODUCTION
A peptic ulcer is a hole in the gut lining of the stomach, duodenum, or esophagus. A peptic ulcer of the stomach is called a gastric ulcer; of the duodenum, a duodenal ulcer; and of the esophagus, an esophageal ulcer. An ulcer occurs when the lining of these organs is corroded by the acidic digestive juices which are secreted by the stomach cells. Peptic ulcer disease is common, affecting millions of Americans yearly. The medical cost of treating peptic ulcer and its complications runs in the billions of dollars annually. Recent medical advances have increased our understanding of ulcer formation [1,2].
[adsense:336x280:8701650588]
Reference Id: PHARMATUTOR-ART-1168
Ulcers average between one-quarter and one-half inch in diameter. They develop when digestive juices produced in the stomach, intestines, and digestive glands damage the lining of the stomach or duodenum.
The two important digestive juices are hydrochloric acid and the enzyme pepsin. Both substances are critical in the breakdown and digestion of starches, fats, and proteins in food. They play different roles in ulcers.About 25 million American are expected to have peptic ulcers at some point in their lives. Peptic ulcer disease affects all age groups but is rare in children. Men have twice the risk for ulcers as women. The risk for duodenal ulcers tends to rise at around age 25 and continues until age 75; gastric ulcers peak in people between the ages of 55 and 65.
2. PEPTIC ULCER
2.1. Causes
For many years, excess acid was believed to be the major cause of ulcer disease. Accordingly, treatment emphasis was on neutralizing and inhibiting the secretion of stomach acid. While acid is still considered significant in ulcer formation, the leading cause of ulcer disease is currently believed to be infection of the stomach by a bacteria called "Helicobacter pyloridus" (H. Pylori).Before the discovery of the bacterium H. Pylori, the stomach was believed to be a sterile environment. However, in 1982 two Australian scientists identified H. Pylori as the main cause of stomach ulcers. They showed that inflammation of the stomach and stomach ulcers result from an infection of the stomach caused by the H. Pylori bacteria. This discovery was so important that the researchers were awarded the Nobel Price in Medicine in 2005. The bacteria appear to trigger ulcers in the following way:
· H. Pylori's corkscrew shape enables it to penetrate the mucous layer of the stomach or duodenum so it can attach itself to the lining.
· It survives in the highly acidic environment by producing urease, an enzyme that generates ammonia to neutralize the acid.
· H. Pylori then produces a number of toxins and factors that can cause inflammation and damage to the lining, leading to ulcers in certain individuals.
· It also alters certain immune factors that allow it to evade detection and cause persistent inflammation for a life even without invading the mucous membrane.
It is also strongly linked to stomach (gastric) cancer and possibly other non-intestinal problems. The magnitude of H. Pylori infection, particularly in older people, may not always predict the presence or absence of peptic ulcers. Other variables must to be present to actually trigger ulcers. These may include:
[adsense:468x15:2204050025]
·Genetic Factors. Some people harbor genetic strains of H. Pylori that may make the bacteria more dangerous and increase the risk for ulcers. The most intensively investigated genetic factor is cytotoxin-associated gene A (CagA), which has been associated with both gastric and duodenal ulcers, as well as with stomach cancer. Other genetic types that may also increase bacterial severity are called vacuolating cytotoxin (vacA) and antigen-binding adhesin (BabA) genotypes. Some of these genetic factors may be more or less important for development of ulcers, depending on ethnicity. [6,7]
·Immune Abnormalities. Some experts suggest that certain individuals have abnormalities in the immune response of the intestine, which allow the bacteria to injure the lining.
·Lifestyle Factors. Although lifestyle factors such as chronic stress, drinking coffee, and smoking were long believed to be primary causes of ulcers, it is now thought they only increase susceptibility to ulcers in some H. Pylori carriers.
·Shift Work and Other Causes of Interrupted Sleep. People who work the night shift have a significantly higher incidence of ulcers than day workers. Researchers suspect that frequent interruptions of sleep may weaken the ability of the immune system to protect against endotoxins.
When H. Pylori was first identified as the major cause of peptic ulcers, it was found in 90% of people with duodenal ulcers and in about 80% of people with gastric ulcers. As more people are being tested and treated for the bacteria, however, the rate of H. Pylori- associated ulcers has declined. For example, a 2001 study suggested that about half of ulcers are not caused by H. Pylori. Instead, they tend to be caused by regular use of nonsteroidal anti-inflammatory drugs (NSAIDs), which include aspirin and other common pain relievers. Genetic factors or, rarely, Crohn's disease or Zollinger-Ellison syndrome, also cause ulcers [9].
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
Some researchers now believe that duodenal ulcers are not caused by H. Pylori, but that the presence of the bacteria simply delays healing. This fact, they say, may explain why up to half of cases of acute duodenal perforation show no evidence of H. Pylori, and why duodenal ulcers can recur even after H. Pylori has been eradicated.
A 2006 study published in the Journal of Biological Chemistry indicates that a protein called decay-accelerating factor (DAF) acts as receptor for H. Pylori. Animal studies show that blocking this interaction renders H. Pylori harmless to the stomach. Researchers hope the discovery leads to new drugs that can reduce the risk of peptic ulcer [5].
Long-term use of NSAIDs is the second most common cause of ulcers, and the rate of NSAID-caused ulcersis increasing. About 20 million people take prescription NSAIDs regularly, and more than 25 billion tablets of over-the-counter brands are sold each year in the U.S. alone. The most common NSAIDs are aspirin, ibuprofen, and naproxen, although many others are available. Patients with NSAID-caused ulcers should stop taking these drugs [10].
There is no doubt NSAIDs increase the risk of ulcers and gastrointestinal (GI) bleeding. The risk of bleeding is continuous for as long as a patient takes these drugs and may persist for about one year after stopping. Short courses of NSAIDs for temporary pain relief should not cause major problems, because the stomach has time to recover and repair any damage that has occurred.
Specific NSAIDs pose greater or lesser risks for ulcers and bleeding. No NSAIDs, however, even over-the-counter brands, should be used long-term except under a doctor's direction [10,12].
Certain drugs other than NSAIDs may cause or aggravate ulcers, particularly those taken for cardiovascular disease and its risk factors. A review of more than 306,000 primary care patients found that spironolactone, a common diuretic prescribed in heart failure, was associated with a 2.7% increased risk of ulcer or upper GI bleeding. Exacerbation of peptic ulcers is a rare but noted side effect of niacin, a drug that can reduce LDL cholesterol and raise HDL cholesterol. Low-dose aspirin, dipyridamole, and vitamin K antagonists such as Coumadin nearly double the risk of upper GI bleeding [11].
The least common major cause of peptic ulcer disease is Zollinger-Ellison syndrome (ZES).Zollinger-Ellison syndrome (ZES) is the least common major cause of peptic ulcer disease. In this condition, tumors in the pancreas and duodenum (gastrinomas) produce excessive amounts of gastrin, a hormone that stimulates gastric acid formation. These tumors are usually malignant, so proper and prompt management of the disease is essential.
These tumors are usually malignant, must be removed and acid production suppressed to relieve the recurrence of the ulcers.
The incidence of ZES in the United States is estimated at 1 case per million people per year, and at 0.1 - 1% among patients with peptic ulcers. The mean age at onset is 45 - 50, and men are affected more often than women [13].
Rarely, certain conditions may cause ulceration in the stomach or intestine, including:
· Radiation treatments
· Bacterial or viral infections
· Alcohol abuse
· Physical injury
· Burns
2.2. SYMPTOMS
Dyspepsia:The most common symptoms of peptic ulcer are known collectively as dyspepsia. Peptic ulcers can occur without dyspepsia or any other gastrointestinal symptom, especially when caused by NSAIDs. Dyspepsia may be persistent or recurrent and can encompass a variety of symptoms in the upper abdomen, including:
· Pain or discomfort
· Bloating
· A feeling of fullness. People with severe dyspepsia are unable to drink as much fluid as people with mild or no dyspepsia.
· Hunger and an empty feeling in the stomach, often 1 - 3 hours after a meal
· Mild nausea (Vomiting, in fact, may relieve symptoms.)
·Regurgitation (sensation of acid backing up into the throat.)
· Belching
Ulcer Pain:The pain of ulcers can be either localized in one place or diffuse. The pain is described as a burning, gnawing, or aching in the upper abdomen, or as a stabbing pain penetrating through the gut. The symptoms may vary depending on the location of the ulcer:
· Duodenal ulcers often cause a gnawing pain in the upper stomach area several hours after a meal, and the pain is often relieved by eating a meal.
· Gastric ulcers may cause a dull, aching pain, often right after a meal; eating does not relieve the pain and may even worsen it. Pain may also occur at night.
Ulcer pain may be particularly confusing or disconcerting when it radiates to the back or to the chest behind the breastbone. In such cases it can be confused with other conditions such as heart attack.
Symptoms of Anemia: Because ulcers can cause hidden bleeding, patients may experience the symptoms of anemia, including fatigue and shortness of breath[14].
Emergency Symptoms: A sudden onset of severe symptoms may indicate intestinal obstruction, perforation, or hemorrhage, all of which are emergencies. Symptoms may include:
· Tarry, black, or bloody stools
· Severe vomiting, which may include blood or a substance with the appearance of coffee grounds (a sign of a serious hemorrhage) or entire stomach contents (sign of intestinal obstruction)
· Severe abdominal pain with or without vomiting or evidence of blood
Anyone who experiences any of these symptoms should go to the emergency room immediately.
Peptic ulcers may lead to emergency situations. Severe abdominal pain with or without evidence of bleeding may indicate a perforation of the ulcer through the stomach or duodenum. Vomiting of a substance that resembles coffee grounds or the presence of black tarry stools may indicate serious bleeding.
2.3. Classification
A peptic ulcer may arise at various locations:
- Stomach (called gastric ulcer)
- Duodenum (called duodenal ulcer)
- Esophagus (called esophageal ulcer)
- Meckel's Diverticulum (called Meckel's Diverticulum ulcer)
Types of peptic ulcers:
Type I: Ulcer along the lesser curve of stomach
Type II: Two ulcers present - one gastric, one duodenal
Type III: Prepyloric ulcer
Type IV: Proximal gastresophageal ulcer
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
2.4. DIAGNOSIS
A peptic ulcer is always suspected in patients with persistent dyspepsia. Dyspepsia, however, occurs in 20% to 40% of people who live in industrialized nations, and only about 15% to 25% of these people actually have an ulcer. There are a number of steps needed to make an accurate diagnosis of ulcers.
Medical and Family History:The physician will ask for a thorough report of a patient's dyspepsia and other important symptoms, such as weight loss or fatigue, any present and past medication use (especially chronic use of NSAIDs), family members with ulcers, and drinking and smoking habits.
Ruling Out Other Disorders:In addition to peptic ulcers, a number of conditions, notably gastroesophageal reflux disease (GERD and irritable bowel syndrome), cause dyspepsia. In most cases, however, no cause can be determined. (In such cases, the symptoms are
referred to collectively as functional dyspepsia.)Peptic ulcer symptoms, notably abdominal and chest pain, may resemble those of other conditions, such as gallstones,or even the chest pain of heart attack. Certain features may help to distinguish these different conditions. However, symptoms often overlap, and it is impossible to make a diagnosis based on symptoms alone. A number of tests are needed.
The following are some disorders that may be confused with peptic ulcers:
Ø GERD. About half of patients with gastroesophageal reflux disease (GERD) also have dyspepsia.With GERD or other problems in the esophagus (food pipe), however, the main symptom is usually heartburn, a burning pain that radiates up to the throat. It typically develops after meals and is often relieved by antacids. The patient may have difficulty swallowing, and there is often regurgitation or acid reflux.Pain due to heart events, such as angina or a heart attack, is more likely to occur with exercise, and it may radiate to the neck, jaw, or arms. In addition, patients typically have distinct risk factors for heart disease, such as a family history, smoking, high blood pressure, obesity, and high cholesterol.Gallstones. The primary symptom in gallstones is typically a steady gripping or gnawing pain on the right side(under the rib cage), which can be quite severe and can radiate to the upper back. Some patients experience the pain behind the breast bone. The pain is often precipitated by a fatty or heavy meal, but gallstones almost never cause dyspepsia [15,16].
Ø Irritable Bowel Syndrome. Irritable bowel syndrome can cause dyspepsia, nausea and vomiting, bloating, and abdominal pain. It occurs more often in women. Dyspepsia may also occur with gastritis, stomach cancer, or as a side effect of certain drugs, including NSAIDs, antibiotics, iron, corticosteroids, theophylline, and calcium blockers used to treat high blood pressure.
Noninvasive Tests for Gastrointestinal (GI) Bleeding: When ulcers are suspected, the physician administers tests to detect any bleeding. They include a rectal exam, a complete blood count, and a fecal occult blood test (FOBT). The FOBT tests for hidden (called occult) blood in stools. Typically, the patient is asked to supply up to six stool specimens in a specially prepared package. A small quantity of feces is smeared on specially treated paper, which reacts to hydrogen peroxide. If blood is present, the paper turns blue.
Noninvasive Screening Tests for H. Pylori: Simple blood, breath, and stool tests can now detect H. Pyloriwith a fairly high degree of accuracy. It is not entirely clear, however, which individuals should be screened for H. Pylori.
Candidates for Screening. Some physicians currently test for H. Pylorionly in individuals with dyspepsia who also have high−risk conditions, such as the following:
- Strong indications for ulcers, such as weight loss, anemia, or indications of bleeding.
- History of active ulcers.
- Risk factors for stomach cancer or other complications from ulcers.
Smokers and those who experience regular and persistent pain on an empty stomach may also be good candidates for screening tests. Some physicians argue that testing for H. Pylorimay be beneficial patients with dyspepsia who are regular NSAID users. In fact, given the possible risk for stomach cancer in H. Pyloriinfected people with dyspepsia, some experts now recommend that any patient with dyspepsia that lasts longer than four weeks should be given blood tests for H. Pylori.
Specific Screening Tests for H. Pylori: The following are the screening tests used or under investigation for H. Pylori.
Breath Test: A simple test called the carbon isotope−urea breath test (UBT) can identify up to 99% of people who harbor H. Pylori. Up to two weeks before the test the patient must be off any antibiotics, bismuth−containing agents (such as Pepto Bismol), and proton−pump inhibitors. As part of the test, the patient swallows a special substance containing urea (a compound in mammals metabolized from nitrogen) that has been treated with carbon atoms. If present, the H. Pyloribacteria convert the urea into carbon dioxide, which is detected and recorded in the patient's exhalation after ten minutes.
Blood Tests: Blood tests are used to measure antibodies to H. Pylori, with results available in minutes.Diagnostic accuracy is reported at 80% and 90%. One such important test is called enzyme−linked?immunosorbent assay (ELISA). An ELISA test of the urine is also showing promise in children.
Stool Test:A test to detect genetic fingerprints of H. Pyloriin the feces appears to be as accurate as the breath test for initial detection of the bacteria and for detecting recurrences after antibiotic therapy.
Panendoscopy: Panendoscopy (also called gastroscopy or, simply, endoscopy) is a procedure that evaluates the esophagus, stomach, and duodenum using an endoscope (a long thin tube containing a tiny video camera). When used with biopsy, panendoscopy is the most accurate procedure for detecting the presence of peptic ulcers, bleeding, and stomach cancer.It can also be used to confirm a diagnosis of H. Pylori.Appropriate Candidates for Panendoscopy. Panendoscopy is invasive and expensive and not suitable for everyone with dyspepsia. Most individuals with these symptoms are managed effectively after simple screening methods. Panendoscopy is usually reserved for patients with dyspepsia who also have risk factors for ulcers, stomach cancer, or both. Such factors include the following:
- Having so−called "alarm" symptoms (unexplained weight loss gastrointestinal bleeding, vomiting, difficulty in swallowing, or anemia).
- Being over 45 (when the risk for stomach cancer increases).
There is some debate over whether patients under 45 with persistent dyspepsia and no alarm symptoms should have endoscopy.
Capsule Endoscopy: Capsule endoscopy involves swallowing a capsule the size of a large vitamin, which contains tiny camera, light source, and a radio transmitter. The device takes and records pictures as it passes through the intestinal tract. At this point, its benefits are limited to the small intestine, so it is unlikely to play a role in the diagnosis of peptic or gastric ulcers. However, it has the potential to be an important tool for the diagnosis of obscure upper GI bleeding. Patients who have used it have usually found it painless and preferable to conventional endoscopy.
Upper GI Series:The upper GI (gastrointestinal) series was the standard diagnostic method for peptic ulcers until the introduction of adequate tests for detecting H. Pylori. The patient drinks a solution containing barium. Then x−rays are taken, which may reveal inflammation, active ulcer craters, or deformities and scarring due to previous ulcers. Endoscopy is more Accurate, although more invasive and expensive.
Other Laboratory Tests: Stool tests may show traces of blood that are not visible, and blood tests may reveal anemia in those who have bleeding ulcers. If Zollinger−Ellison syndrome is suspected, blood levels of gastrin should be measured.
2.5. Pathophysiology
Historically, our understanding of the pathophysiology of peptic ulcer disease focused on abnormalities in the secretion of gastric acid and pepsin, and on the suppression of acid as a treatment strategy. Today, gastric hypersecretion-associated with gastrinoma in Zollinger–Ellison syndrome, antral G-cell hyperplasia, an increase in parietal-cell mass, and a physiological imbalance between the antagonistic gastric hormones gastrin and somatostatin—is still an important issue in peptic ulcer disease. Moreover, it is known that cholinergic hypersensitivity and parasympathetic dominance are related to the stimulation not only of hydrochloric acid but also pepsin, which is often neglected as a cofactor in the development of erosive injury to the gastric mucosa. Psychologic stress, cigarette smoking, alcohol consumption, use of nonsteroidal anti-inflammatory drugs (NSAIDs) including aspirin, oral bisphosphonates, potassium chloride, immunosuppressive medications, and an age-related decline in prostaglandin levels have all been shown to contribute to peptic ulcer disease. It was, however, the isolation of H. Pylori and its identification as the most important cause of peptic ulcer disease that led to exploration of the role of inflammation and its associated cytokine cascade in gastric acid secretion.
H. Pylorievades attack by the host immune system and causes chronic, indolent inflammation by several mechanisms. H. Pylori can damage the mucosal defense system by reducing the thickness of the mucus gel layer, diminishing mucosal blood flow, and interacting with the gastric epithelium throughout all stages of the infection. H. Pylori infection can also increase gastric acid secretion; by producing various antigens, virulence factors, and soluble mediators, H. Pylori induces inflammation, which increases parietal-cell mass and, therefore, the capacity to secrete acid. The H. Pylori cytotoxin-associated gene CagA also has an important role: it interferes with gastric epithelial cell-signaling pathways, thereby regulating cellular responses and possibly contributing to apical junction barrier disruption, interleukin-8 secretion and phenotypic changes to gastric epithelial cells.
Understanding the pathophysiology of peptic ulcer disease is at something of a crossroads: mechanisms of injury differ distinctly between duodenal and gastric ulcers. Duodenal ulcer is essentially an H. Pylori-related disease and is caused mainly by an increase in acid and pepsin load, and gastric metaplasia in the duodenal cap. Gastric ulcer, at least in Western countries, is most commonly associated with NSAID ingestion, although H. Pylori infection might also be present Chronic, superficial and atrophic gastritis predominate in patients with gastric ulcers, when even normal acid levels can be associated with mucosal ulceration In both conditions, ulcer is associated with an imbalance between protective and aggressive factors, with inflammation being a leading cause of this imbalance.
The isolation of H. Pylori in the early 1980s was one of the most exciting advances in the history of peptic ulcer disease, and it has dramatically changed the management of peptic ulcer. Eradication of H. Pylori infection is now the mainstay of treatment for peptic ulcer disease, and has resulted in very high ulcer healing rates and recurrence rates that have dropped dramatically, especially for individuals with a duodenal ulcer. The greater recognition of the role of NSAIDs and aspirin in gastrointestinal-tract injury has led to the development of therapeutic and preventive strategies that rely on the use of antisecretory drugs, the prostaglandin analog misoprostol, or selective cyclo-oxygenase (COX)-2 inhibitors (coxibs) [37].
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
2.6. TREATMENT
2.6.1. DRUG TREATMENT
The following drugs are sometimes used in the treatments of peptic ulcers caused by either NSAIDs or H. Pylori
H2 Blockers: H2 blockers impede acid production by blocking the actions of histamine, a substance produced by the body that encourages acid secretion in the stomach. H2 blockers were the standard treatment for peptic ulcers until the development of antibiotic regimens against H. Pylori. These drugs cannot cure ulcers, but in certain cases they are useful. They are effective only for duodenal ulcers, however, and have little effect on stomach (gastric) ulcers. Four H2 blockers are currently available over the counter in the US: famotidine (Pepcid AC), cimetidine (Tagamet), ranitidine (Zantac), and nizatidine (Axid). All have good safety profiles and few side effects. Each is discussed below. H2 blockers can interact with other drugs, so the physician should be made aware of any other drugs a patient is taking. There are some differences among these drugs. Famotidine (Pepcid AC). Famotidine (Pepcid AC) is the most potent H2 blocker. The most common side effect of famotidine is headache, which occurs in 4. 7% of people who take it. Famotidine is virtually free of drug interactions but it may have significant adverse effects in patients with kidney problems. Cimetidine. Cimetidine (Tagamet) has few side effects; approximately 1% of people taking cimetidine will experience mild temporary diarrhea, dizziness, rash, or headache. Cimetidine interacts with a number of commonly used medications, such as phenytoin, theophylline, and warfarin. Long term use of excessive doses (more than 3 grams a day) may cause impotence or breast enlargement in men; these problems resolve after the drug is discontinued. Ranitidine. Ranitidine (Zantac) interacts with very few drugs. In one study, ranitidine provided more pain relief and healed ulcers more quickly than cimetidine in people younger than 60, but there was no difference in older patients. A Peptic Ulcers 14 common side effect of ranitidine is headache, which occurs in about 3% of the people who take it. Nizatidine. Nizatidine (Axid) is a new H2 blocker. It is nearly free of side effects and drug interactions. Long−Term Concerns. In most cases, these agents have good safety profiles and few side effects. H2 blockers caninteract with other drugs, although some less so than other. In all cases, however, the physician should be made aware of any other drugs a patient is taking. There are also some concerns about possible long−term effects.
Also of concern are reports that long−term acid suppression with these drugs may cause cancerous changes in the stomach in patients who also have untreated H. Pyloriinfections.
- Liver damage. (This is more likely with ranitidine than other H2 blockers, but is rare in any event.)
- Kidney−related complications. Adverse effects on the central nervous system in patients with even moderate renal (kidney) insufficiency have been reported with famotidine and may result in anxiety, depression, and mental disturbances.
- Increased risk for pneumonia in hospitalized patients. Ulcer complications (perforation, bleeding). Some experts are concerned that the use of acid−blocking drugs may actually increase the risk for serious complications from ulcers by masking their symptoms
Proton−Pump Inhibitors (PPIs): Actions against Ulcers. Proton−pump inhibitors (PPIs) are the drugs of choice for managing patients with peptic ulcers from any cause. They suppress the production of stomach acid. These agents work by inhibiting the molecule in thestomach glands that is responsible for acid secretion, which is called the gastric acid pump. PPIs can be used as part of a multi−drug regimen for H. Pylorior used alone for preventing and healing NSAID−related ulcers. They are even useful in the treatment of ulcers caused by Zollinger−Ellison syndrome. (Of note, certain individuals carry a gene that regulates an enzyme called CYP2C19 that reduces the effectiveness of proton−pump inhibitors. This gene may be present in between 18% and 20% of Asians, who may not respond as well to these agents.) Standard Brands. The standard PPI for ulcers has been omeprazole (Prilosec). In fact, it has been recommended for over−the−counter use. Other newer agents include lansoprazole (Prevacid), rabeprazole (Aciphex), esomeprazole (Nexium), and pantoprazole (Protonix). All are available orally. Pantoprazole is also available as an injection and lansoprazole as a suspension, which may be useful for patients who cannot take oral medications. In a comparison study of these agents, esomeprazole was superior in treating healing injuries in the esophagus that caused gastroesophageal reflux disease (GERD). It is not known yet, however, whether any individual PPI has superior advantages for treating ulcers.
Adverse Effects. Proton−pump inhibitors may pose the following concerns:
Side effects are uncommon but may include headache, diarrhea, constipation, nausea, and itching.
Proton−pump inhibitors should be avoided by pregnant women and nursing mothers, although recent studies suggest that they do not pose an increased risk of birth defects.They may interact with certain drugs, such as antiseizure agents (e.g., phenytoin), anti−anxiety drugs (e.g., diazepam), and blood thinners (e.g., warfarin).Long−term use of high−dose PPIs may produce vitamin B12 deficiencies, but studies are needed to confirm
any significance of this risk.The long−term use of proton−pump inhibitors by people with H. Pylorimay, in theory at least, reduce acid secretion enough to cause atrophic gastritis (chronic inflammation of the stomach). This condition, in turn, is a risk factor for stomach cancer. To compound concerns, long−term use of PPIs may mask symptoms of stomach cancer and so delay a diagnosis. To date, however, there have been no reports of an increased risk of stomach cancer with long−term use of these drugs
Prostaglandin analogues:Misoprostol (Cytotec) is prostaglandin analogue and increases prostaglandin levels in the stomach lining, which protects against the major intestinal toxicity of NSAIDs. Actions Against Ulcers. Misoprostol can reduce formation of ulcers in the upper small intestine by two−thirds and in the stomach by three quarters. It does not neutralize or reduce acid, so although the drug is helpful for preventing NSAID−induced ulcers, it is not useful in healing existing ulcers.
Side Effects.Diarrhea and other gastrointestinal problems are severe enough to cause 20% of patients to stop taking thedrug. Taking misoprostol after meals should minimize these effects. One study indicated that taking the drugtwo or three times a day instead of the standard regimen of four times may prove to be just as effective and cause fewer side effects.Misoprostol can induce abortion or cause birth defects and should not be taken by pregnant women. If pregnancy occurs during treatment, the drug should be discontinued at once and the physician contacted immediately.
Antacids: Many antacids are available without prescription and are the first drugs recommended to relieve heartburn and mild dyspepsia. They play no major role in either prevention or healing of ulcers but help in the following ways:
All of the many brands available rely on various combinations of three basic compounds, magnesium, calcium, or aluminum, which neutralize the acid in the stomach.
They may also defend the stomach by increasing acid−buffering bicarbonate and mucus secretion.It is generally believed that liquid antacids work faster and are more potent than tablets, although some evidence suggests that both forms work equally well.
Basic Salts Used in Antacids. There are three basic salts used in various antacids:
Magnesium: Magnesium compounds are available in the form of magnesium carbonate, magnesium trisilicate, and, most commonly, magnesium hydroxide (Milk of Magnesia). The major side effect of these magnesium compounds is diarrhea.
Calcium: Calcium carbonate is a potent and rapid−acting antacid. It can cause constipation. There have been rare cases of hypercalcemia (elevated levels of calcium in the blood) in people taking calcium carbonate for long periods of time. This can lead to kidney failure and is very dangerous. None of the other antacids have this side effect.
Aluminum: The most common side effect of antacids containing aluminum compounds (Amphogel, Alternagel) is constipation. Maalox and Mylanta are combinations of aluminum and magnesium, which balance the side effects of diarrhea and constipation. People who take large amounts of antacids that contain aluminum may also be at risk for calcium loss and osteoporosis. Long−term use also increases the risk for kidney stones. People who have recently experienced GI bleeding should not use aluminum compounds, if possible. Interactions with Other Drugs. Antacids can interact with a number of drugs in the intestines and reduce their absorption. Conversely, some antacids increase the potency of certain drugs. The interactions can be avoided by taking these other drugs one hour before or three hours after the antacid.
Drug Interactions with Antacids (e.g., Maalox, Mylanta): Drugs that are less absorbed with antacids Drugs that are made more potent with
Antacids: tetracycline ciprofloxacin (Cipro) valproic acid sulfonylureas propranolol (Inderal)captopril (Capoten) ranitidine (Zantac) famotidine (Pepcid AC) quinidine levodopa
Ulcer Protectives: Bismuthcompounds that contain bismuth are often used in the three−drug antibiotic regimens. They destroy the cell walls of the H. Pyloribacteria. The only bismuth compound available in the US has been bismuth subsalicylate (Pepto−Bismol), although a drug combination of the H2 blocker ranitidine and bismuth citrate (Tritec) has been released. High doses can cause vomiting and depression of the central nervous system, but the doses given for ulcer patients rarely cause side effects.
Sucralfate (Carafate) seems to work by adhering to the ulcer crater and protecting it from further damage by stomach acid and pepsin. It also promotes the defensive processes of the stomach. Sucralfate has an ulcer−healing rate similar to that of H2 blockers. Other than constipation, which occurs in 2.2% of patients, the drug has few side effects. Sucralfate does interact with a wide variety of drugs, including warfarin, phenytoin, and tetracycline.
Antibiotics: H. Pyloriis usually highly sensitive to certain antibiotics, particularly amoxicillin or antibiotics such as clarithromycin that belong to the drug class known macrolides. Either type of agent serves effectively as a second antibiotic in a three−drug regimen. Others being used are tetracycline,metronidazole, and ciprofloxacin.Amoxicillin is the most common form of penicillin. It is inexpensive, but many people are allergic to it.Clarithromycin (Biaxin) is a macrolide and is the most expensive of the antibiotics used against H. Pylori. It is also very effective, but there is growing bacterial resistance to this drug. Resistance rates tend to be higher in women and increase with age. Researchers fear that resistance will increase as the drug is used more and more against H. Pylori.Tetracycline is effective, but tetracyclines have unique side effects among antibiotics, including skin reactions to sunlight, possible burning in the throat, and tooth discoloration. Pregnant women cannot take it. Ciprofloxacin (Cipro), known as a fluoroquinolone, is also sometimes used in ulcer regimens. Metronidazole (Flagyl) was the mainstay in initial combination regimens for H. Pylori. As with clarithromycin, however, there continues to be growing bacterial resistance to the drug (about 25% to 35% of H. Pylori bacteria)
Side Effects of Antibiotics.: The most common side effects of nearly all antibiotics are gastrointestinal problems, including cramps, nausea, vomiting, and diarrhea.Allergic reactions can also occur with all antibiotics but are most common with medications derived from penicillin or sulfa. These reactions can range from mild skin rashes to rare but severe, even life−threatening anaphylactic shock.Some drugs, including certain over−the−counter medications, interact with antibiotics; patients should report to the physician all medications they are taking. They double the risk for vaginal infections in women.
Treatment regimes which have been shown in randomized controlled trials (RCTs) to be most effective consist of two antibiotics combined with either bismuth or a proton
pump inhibitor or H2-antagonist.Two regimes are mentioned:
1. “Standard” triple therapy
This is the most thoroughly tested option, consists of a two week course of:
•bismuth subcitrate (4 x 120 mg daily) with
•metronidazole (3 x 400 mg daily) and
•tetracycline (4 x 500 mg daily)
It is cheap and has been shown to eradicate H.pylori in around 95% of patients. One week’s treatment may be as good as two, but a direct comparison has not
been performed. This regimen has commanly been given alongside an H2-antagonist or proton pump inhibitor, but the benifits of this have not been conclusively evaluated.
The H2-antagonist or proton pump inhibitor is stopped once healing has occured.
2. Other triple therapies
A recent multi-centre clinical trial has evaluated five new regimes, and found two to achive eradication rates of 95 per cent or over:
One week of:
•omeprazole (2 x 20 mg daily)
•amoxicillin (2 x 1000 mg daily)
•clarithromycin (2 x 500 mg daily)
Alternatively, one week of:
•omeprazole (2 x 20 mg daily)
•metronidazole (2 x 400 mg daily)
•clarithromycin (2 x 250 mg daily)
Experimental Agents: Ecabet is a unique anti−ulcer agent that is showing promise in early studies. Therapeutic effects of ecabet sodium, an antiulcer drug, on dextran sodium sulfate-induced ulcerative colitis in rats ulcerative colitis model. In vitro ecabet accelerated the restitution of epithelial cells, which was not affected by a TGF-β antibody. Ecabet inhibited the leukotriene B4 production and 5-lipoxygenase activity
It acts on the mucus lining of the stomach and has anti−bacterial activity[13,14].
Endoscopy for Treating or Preventing Bleeding Ulcers: Endoscopy is important for both diagnosing and treating bleeding ulcers. The physician first places an endoscope (a thin, flexible plastic tube) into the patient's mouth and down the esophagus (food pipe) into the stomach. Endoscopy Used for Diagnosing Bleeding Ulcers and Determining Risk for Rebleeding. Physicians are able to detect the signs of bleeding such as active spurting or oozing of blood from arteries. Endoscopy can also detect specific features in the ulcers referred to as stigmata, which indicate a higher or lower risk for rebleeding.
Such features include the following:
Low−risk (5% to 15%) for bleeding: flat dot; a clean or white base.
High−risk (30% to 50%) for bleeding. Swollen but nonbleeding blood vessels; blood clots that adhere to ulcers.According to one study, if patients with these high−risk features are untreated, their risk for rebleeding after endoscopy ranges from about 10% in the first day after endoscopy to about 3% by the third day. Identifying and treating patients with high−risk features in the ulcers (referred to as stigmata) can reduce these risks. (Other factors that increase the risk for rebleeding include have bleeding disorders, very low blood pressure, other serious medical conditions, and bleeding that started after hospitalization.)
Endoscopy as Treatment. Endoscopy is usually employed to treat bleeding from ulcers with visible blood vessels that are less than 2 mm in diameter. This approach also appears to be very effective in preventing rebleeding in patients whose ulcers are not bleeding but have high−risk features (swollen blood vessels or clots adhering to ulcers).
The surgeon passes a probe through an endoscopic tube and applies electricity, heat, or small clips to coagulate the blood and stop the bleeding. It also causes fluid build−up that helps to compress the blood vessels.Peptic Ulcers n high−risk cases, the physician may inject epinephrine (commonly known as adrenaline) directly into the ulcer to enhance the effects of the heating process. Epinephrine activates the process leading to blood
coagulation, narrows the arteries, and enhances blood clotting.
Intravenous (IV) administration of a proton pump inhibitor most likely omeprazole or the newer PPI pantoprazole−significantly prevents rebleeding and appears to be cost effective. In one major study, the use of IV proton−pump inhibitors reduced the risk for bleeding from 23% without the agent to 7% with a PPI. (Oral PPIs are also effective, but studies are needed to compare their effectiveness with IV PPIs. A proton−pump inhibitor may also be useful alone for initial bleeding episodes if endoscopy is unsuccessful, inappropriate, or unavailable.)
Intravenous H2 blockers are often used, but a major analysis reported no benefits from their use in bleeding duodenal ulcers−−although they may be useful for gastric ulcers. Endoscopy is effective in controlling bleeding in more than 85% of appropriate candidates. If rebleeding occurs, a repeat endoscopy performed by experienced doctors may be effective in about 75% of cases. Those who fail to respond require major abdominal surgery. The most serious complication from endoscopy is perforation of the stomach or intestinal wall, which occurred in about 1.4% of patients in one large 2002 study.
Other Medical Considerations. Certain agents may be warranted after endoscopy: Patients who harbor the H. Pyloribacteria, even if NSAIDs caused the bleeding, should be treated with antibiotic therapy to eradicate the bacteria. Triple therapy, including antibiotics, to eradicate H. Pyloriimmediately after endoscopy is warranted in most patients infected with the bacteria.
Somatostatin (a hormone used to prevent bleeding in cirrhosis) is also useful for reducing persistent peptic ulcer bleeding or the risk of recurrence. Researchers are investigating adding other therapies, such as fibrin glue, a blood clotting factor. To date none are more effective than the current therapies.
2.6.2. SURGICAL TREATMENT
"Major abdominal surgery for bleeding ulcers is now generally performed only when endoscopy fails or is not appropriate. Certain emergencies may require surgical repair, such as when an ulcer perforates the wall of the stomach or intestine, causing sudden intense pain and life−threatening infection. The surgical treatment of perforated ulcer dates from the year1880, when Mikulicz sutured a perforated gastric ulcer for the first time [25]. Suture is still the method of choice for surgical treatment of ulcer perforation [23]. The first two cases of primary gastric resection for ulcer perforation was described by von Haberer as early in 1919 [26]. The method was used extensively for several decades [23] but is now rarely used for treatment of ulcer perforation. During the 1970s and 1980s suture supplemented with vagotomy was an alternative surgical procedure [27, 28]. Conservative management of ulcer perforation as an alternative to surgery in selected patients was first advocated by Taylor in 1946 [29]. Series practicing such treatment have reported amazingly good results, with lethality rates of 5% to 11% [29, 30]. This treatment strategy, however, has never been accepted generally. When antibiotics came into general use around 1950, markedly reduced rates of postoperative complications and deaths after ulcer perforation were observed (Fig. 5) [23,31]. Use of antibiotics is today standard treatment with ulcer perforation surgery. As recognized from the first years of surgical treatment, the duration of perforation is an important treatment aspect. Inolder studies (1939–1953) the time from perforation to operation was short (median values up to 6 hours), reported by Yudine [24], DeBakey [23], and Noordijk . Far longer treatment delays are reported in more recent studies (1980–1990) (median values ranging from 12 to 24 hours); reported by Mattingly et al. Boey et al. [32], Irvin [33], Bodner et al. and Gunshefski et al.A study from Norway showed a steady increase in treatment delay during the period 1935–1990, reflecting an increase in in-hospital delay whereas preadmission delay was stable [34]. This increase could be partly attributed to more extensive preoperative diagnostic effort [35], aging of the patients, and a larger proportion of female patients. Delay was longer during regular working hours than at other times of the day, and treatment delay was particularly long among women and elderly patients [34].
2.6.3. COMPLEMENTARY AND SUPPORTIVE THERAPIES
Diet: It was common in the past to restrict people suffering from peptic ulcers to frequent intake of small amounts of bland foods and milk. Exhaustive research conducted since then has shown that a bland diet is not effective in reducing the incidence or recurrence of ulcers, and that frequent small meals throughout the day are no more effective than consumption of three meals per day. Large amounts of food should still be avoided because stretching or swelling of thestomach can result in painful symptoms.
Fruits and Vegetables: The good news is that a diet rich in fiber may cut the risk of developing ulcers in half and speed healing of existing ones. Fiber found in fruits and vegetables is particularly protective; vitamin A contained in many of these foods may increase the benefit. Some studies on associations between specific food chemicals and ulcers are as follows:
In one study, apples and yams appeared to be especially helpful.
Apples, celery, cranberries, onions, red wine, and green and black tea are also high in natural chemicals known as flavonoids that appear to inhibit H. Pylorigrowth and have many other health benefits. In fact, cranberry juice specifically may have properties that help prevent H. Pylorifrom infecting the intestinal lining.
Of great interest are laboratory experiments suggesting that a compound found in broccoli and broccoli sprouts called sulforaphane may also be lethal to H. Pylori, even drug−resistant strains.
Tea has chemicals that may help protect against cancers in the stomach and esophagus. Milk actually encourages the production of acid in the stomach, although moderate amounts (two to three cups a day) can be drunk without harm. Coffee and Carbonated Beverages. Coffee (both caffeinated and decaffeinated), soft drinks, and fruit juices with citric acid increase stomach acid production. Although no studies have proven that any of these drinks contribute to ulcers, consuming more than three cups of coffee per day may increase susceptibility to H. Pyloriinfection. Studies conducted on spices and peppers have yielded conflicting results. The rule of thumb is to use these substances moderately, and to avoid them if they irritate the stomach. Some studies suggest that high amounts of garlic may have some protective properties against stomach cancer, although a recent study concluded that it offered no benefits against H. Pyloriitself and, in high amounts, causes considerable gastrointestinal distress. Although no vitamins have been shown to protect against ulcers, H. Pyloriappears to impair absorption of vitamin C, which may play a role in the higher risk of stomach cancer.
Exercise: Some evidence exists that exercise may help reduce the risk for ulcers in some people. In one 2000 study, exercise was associated with a lower risk for duodenal (but not gastric) ulcers in men. In this study, exercise appeared to have no effect on ulcer development in women.
Stress Relief: Stress relief programs have not been shown to promote ulcer healing, but they may have other health benefits.
Alternative Treatments: Melatonin is a hormone found in the brain that is normally associated with its role in sleep. Researchers have alsoobserved that gastrointestinal tract is rich in melatonin, and that the hormone may have properties that help prevent ulcers, reduce acid secretion, and improve blood flow. It is not known whether this would benefit peptic ulcers, but it appears to warrant some research. Melatonin is a powerful hormone that can have major effects on all parts of the body.Doses of melatonin over 0.3 can disrupt the body's natural clock in the brain and long−term consequences are unknown.
High doses have been associated with the following adverse events:
- Mental impairment.
- Severe headaches.
- Nightmares.
Interactions with other drugs are not completely known. It should be stressed that melatonin is currently classified as a dietary supplement and not as a drug, so its quality and effectiveness is uncontrolled in the US. (The United States is the only developed nation that does not regulate this agent.) The bottom line is that at this time, people who take melatonin are experimenting on themselves.
Herbal medication and yoga: Herbal medications and supplements (such as liqorice, marshmallow, and glutamine) probably have no role in the treatment of peptic ulcers. Asanas, which are beneficial in the treatment of hyperacidity and ulcers, are vajrasana, uttanpadasana, pavanarnuktasana, bhujangasana, paschimottanasana. Yogic kriyas like Jalneti and pranaya
Home Remedies for Peptic Ulcer:Given below are the simplest and the most effective home remedies for the treatment of peptic ulcers.Fenugreek (methi) seeds:Take 2-3 tablespoon of fenugreek (methi) seeds and boil it in a glass of water. Add little amount of soil to it. Allow the mixture to boil till it become half of its constituent. Take this mixture 2-3 times a day, until the ulcer is not cured completely. One of the useful home remedies for peptic ulcers.
Fruits: Among various other fruits, banana is considered as one of an effective fruit for treating peptic ulcer. Banana helps in lowering the acidic substance inside the body. Take 2-3 bananas mixed in a glass of milk for 4-5 times a day. Similarly, wood apple (bael) is also very useful. Take few bael leaves and keep it into water overnight. Drain the mixture and take this 2-3 times a day. This works great for peptic ulcer patient. One of the useful home remedies for peptic ulcers.
Milk: Milk is really good for patient with peptic ulcer. Patient should take 2-3 glasses of water everyday. Warm milk containing drops of castor oil is also very good for treating peptic ulcer.
Lemon: Lemon extract or juice is also very effective in treating peptic ulcer. Prepare fresh lemon juice, add little amount of salt to it. This drink helps in digestion and hence helps in treating peptic ulcers. This is one of the best home remedies for peptic ulcers.
Vegetables: Among vegetables cabbage is very useful for treating peptic ulcer. Cut cabbage into small pieces, allow the vegetable to boil in water till the constituent become half. Drain the mixture and take this 2-3 time a day. One can also add little amount of black pepper powder to it.
Drumsticks: Drumstick leaves are also an effective home remedy for the treatment of peptic ulcer. Take 15-20 leaves of drumstick and make its paste. Mix this paste in fresh curd. Take this 2-3 times a day. This is one of the important home remedies for peptic ulcers.
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
2.7. RISK FACTORS
About 25 million people in the U.S. are expected to develop peptic ulcers at some point in their lives. Peptic ulcer disease affects all age groups, but is rare in children. Men have twice the risk of ulcers as women. The risk of duodenal ulcers tends to rise beginning around age 25 and continues until age 75; gastric ulcers peak at age 55 - 65. Peptic ulcers are less common than they once were. Research suggests that ulcer rates have even declined in areas with widespread H. Pylori infection. The increased use of proton-pump inhibitor drugs may be responsible for this trend.
Risk Factors for H. Pylori: H. Pylorigrows and colonizes only in the intestinal tracts of primates. The bacteria are most likely transmitted directly from person to person. Still, little is yet known about its transmission. About half the world's adults are infected with H. Pylori. The bacteria are nearly always acquired during childhood and persist throughout life, if not treated. The prevalence in children ranges from less than 10% to more than 80%, with the highest infection rates (3 - 10%) in developing countries and the lowest (0.5%) in industrialized nations, where rates continue to decline. Even in industrialized countries, however, infection rates in regions with crowded, unsanitary conditions are equal to those in developing countries. It is not entirely clear how the bacteria are transmitted. One study did not find that infected students posed any risk for their classmates. Transmission within families may be the most important route for H. Pylori. A 2002 study reported that spouses of people with peptic ulcers are at significantly higher risk for ulcers, suggesting that the bacteria may be transmitted during intimate contact. Some evidence suggests that bacteria may spread during GI tract illness, particularly when vomiting occurs. The bacteria also may be passed in stools. Since H. Pylori can live in water, but not apparently in food, the bacteria may also be transmitting through sewage-contaminated water.
Although H. Pylori infection is common, ulcers in children are very rare, and only a minority of infected adults develops ulcers. Some known risk factors include smoking, alcohol use, having a relative with peptic ulcers, being male, and the presence of the cytotoxin-associated gene A (CagA). Experts are unable to determine, however, any single factor or group of factors that can determine which infected patients are most likely to develop ulcers.
Risk Factors for NSAID-Induced Ulcers : Between 15 - 25% of patients who have taken NSAIDs regularly will have evidence of one or more ulcers, but in most cases these ulcers are very small. Given the widespread use of NSAIDs, however, the potential total number of people who can develop serious problems may be very large. Long-term NSAID use can damage the stomach and, possibly, the small intestine. In April 2005, the FDA asked manufacturers of prescription NSAIDs to include with their products the same boxed warning used for the COX-2 inhibitor celecoxib (Celebrex). This boxed warning emphasizes the increased risk for cardiovascular events and GI bleeding in people taking these drugs. (Pharmaceutical companies are trying to develop new COX-2 inhibitors without these dangerous side effects. Early safety studies of the novel COX-2 inhibitor known as CS-706 showed its effect on gastric mucosa to be the same as placebo.)
The FDA also requested manufacturers of over-the-counter NSAIDs to revise their labels to include more specific language concerning potential cardiovascular and GI risks. Due to its proven heart benefits, aspirin was excluded from these labeling revisions.
Frequent Users of NSAIDs: Anyone who uses NSAIDs regularly is at risk for gastrointestinal problems. Even low-dose aspirin (81 mg) may pose some risk, although the risk is lower than with standard doses. In one 4-year study, 4.5% of regular NSAID users were hospitalized for GI bleeding. The highest risk, however, was found in people who require long-term use of very high-dose NSAIDs, notably patients with rheumatoid arthritis. Other people who take high doses of NSAIDs include those with chronic low back pain, fibromyalgia, and chronic stress.
Contributing Factors. Certain factors add to the risk for ulcers in NSAID-users:
· Age 65 and older
· History of peptic ulcers or upper gastrointestinal bleeding
· Other serious ailments, such as congestive heart failure
· Use of other medications, such as the anticoagulant warfarin (Coumadin), corticosteroids, or the osteoporosis drug alendronate (Fosamax)
· Alcohol abuse
· Those infected with H. Pylori. A 2002 study reported that the combination of NSAID use and H. Pylori posed a 3.5-fold greater risk of ulcers than either factor alone. However, not all studies have reported the higher risk in infected patients.
|
Ulcer Risk by Specific NSAID |
||
|
Lowest Risk |
Medium Risk |
Highest Risk |
|
· Nabumetone · Etodolac · Salsalate · Sulindac |
· Aspirin. Even low-dose ("baby") aspirin (81 mg) may pose some risk · Ibuprofen · Naproxen · Diclofenac · Tolmetin |
· Flurbiprofen · Piroxicam · Fenoprofen · Indomethacin · Meclofenamate · Ketoprofen Note: Ketoprofen is often considered a medium-risk drug, but one study reported that taking the drug in low doses for as little as 1 week causes significant GI injury. |
Other Risk Factors for Ulcers from Either H. Pylori or NSAIDs:Stress and Psychological Factors. Although stress is no longer considered a cause of ulcers, studies still suggest that stress may predispose a person to ulcers or prevent existing ulcers from healing. Some experts estimate that social and psychological factors play a contributory role in 30 - 60% of peptic ulcer cases, whether they are caused by H. Pylori or NSAIDs. Some experts even believe that the anecdotal relationship between stress and ulcers is so strong that treatment of psychological factors is warranted.
Smoking: Smoking increases acid secretion, reduces prostaglandin and bicarbonate production, and decreases mucosal blood flow. Results of studies on the actual effect of smoking on ulcers, however, are mixed. Some evidence suggests that smoking delays the healing of gastric and duodenal ulcers. One study reported that after ulcers healed, about half of nonsmokers experienced a relapse of their ulcer disease after 1 year, but that all heavy smokers relapsed after 3 months. Other studies have found no increased risk for ulcers in smokers. In any case, any impact of smoking on ulcers does not seem to be affected by the presence of H. Pylori. Tobacco use and exposure may cause an acceleration of coronary artery disease and peptic ulcer disease. It is also linked to reproductive disturbances, esophageal reflux, hypertension, fetal illness and death, and delayed wound healing.
3. CURRENT SCEENERIO
To integrate the realization that peptic ulcer most commonlyreflects infection with Helicobacter pylori or use of aspirin and othernonsteroidal anti-inflammatory drugs (NSAIDs) into a disease managementapproach. Guidelines were outlined by the author andpresented for review to the American College of Gastroenterology (ACG)Practice Parameters Committee, selected by the president of the ACG, and apanel of experts in peptic ulcer, selected by the committee. These guidelines were formulated following extensivereview of the literature obtained by MEDLINE search and presented fordetailed review and revision to unpublicized committee meetings on threeoccasions and to experts by mail. These recommendations are an officialstatement of the ACG and have been approved by the AmericanGastroenterological Association and the American Society forGastroenterological Endoscopy. Firm recommendations are discriminated fromreasonable suppositions pending definitive data. The pathophysiology of Helicobacter pylori-associated gastroduodenal diseases, ulcerogenesis and carcinogenesis is intimately linked to activation of epidermal growth factor receptor (EGFR) and production of vascular endothelial growth factor (VEGF). Extracellular virulence factors such as CagA and VacA have been proposed to regulate EGFR activation and VEGF production in gastric epithelial cells. We demonstrate that the H. Pylori secretory protein, HP0175 by virtue of its ability to bind TLR4, transactivates EGFR and stimulates EGFR-dependent VEGF production in the gastric cancer cell line AGS. Knockout of the hp0175 gene attenuates the ability of the resultant H. Pylori strain to activate EGFR or to induce VEGF production. HP0175-induced activation of EGFR is preceded by translocation of TLR4 into lipid rafts. In lipid rafts, the Src kinase family member Lyn interacts with TLR4 leading to tyrosine phosphorylation of TLR4. Knockdown of Lyn prevents HP0175-induced activation of EGFR and VEGF production. Tyrosine phosphorylated TLR4 interacts with EGFR. This interaction is necessary for the activation of EGFR. Disruption of lipid rafts with methyl cyclodextrin prevents HP0175-induced tyrosine phosphorylation of TLR4 and activation of EGFR. This mechanism of transactivation of EGFR is novel, and distinct from that of metalloprotease-dependent shedding of EGF-like ligands leading to autocrine activation of EGFR. It provides new insight into our understanding of the receptor crosstalk network.Helicobacter pylori infection is the major cause of peptic ulceration and gastric adenocarcinoma. To address the hypothesis that the human acquired immune response to H pylori influences pathogenesis, we characterised the gastric T helper (Th) and regulatory T cell (Treg) response of infected patients.
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
The human gastric CD4+ T cell response of 28 donors who were infected with H pylori and 44 who were not infected was analysed using flow cytometry. The T cell associated mucosal cytokine response was analysed by real-time polymerase chain reaction assay of samples from 38 infected and 22 uninfected donors. Recombinant interleukin 10 (IL10) was added to co-cultures of H pylori and AGS cells and its suppressive effects upon inflammatory responses were measured.
In vitro studies showed that IL10 inhibited IL8 expression and activation of nuclear factor kappa B induced by H pylori in gastric epithelial cells, and enhanced H pylori growth in a bacterial-cell co-culture model.
A number of studies have now demonstrated the efficacy of antibiotic therapy in H pylori eradication compared with conventional therapies. Therefore the exact cause of peptic ulcer is being determined by my forthcoming project reseach. Use of histamine receptor antagonists (cimetidine, ranitidine) or the proton pump inhibitor omeprazole as a single therapy resulted in high levels of ulcer healing of about 78% at 10 weeks after therapy commenced, but eradication of H pylori was low, at 5% or less
Triple therapy studies (in combination with ranitidine or cimetidine) covering up to 768 patients demonstrated eradication rates of about 96%, with ulcer healing in 93% of patients at 10 weeks A recent study (Hosking et al, 1994) examined the need for an acid suppressing medicine (omeprazole) in combination with triple therapy, and found comparable eradication rates and ulcer healing; they concluded that addition of omeprazole was not needed, and that one week of treatment was sufficient. Most other studies continued acid suppressing medicine for some weeks longer than eradication therapy.
Use of amoxycillin with omeprazole, the other major treatment regimen, produced eradication rates of 70-86%, with ulcer healing of 89-95%. The numbers of patients in these studies is smaller, and complicated by an incompletely reported study with high numbers but apparently with less good results both with and without this trial (Unge & Ekstr1993). Omeprazole was usually used for some weeks longer than amoxycillin.
Combining the single arms of randomised controlled trials identified and comparing active eradication therapies with results of ulcer healing therapies using cimetidine, ranitidine or omeprazole, it can be seen that the eradication therapies are highly effective. The improved eradication rates are highly significant, and the numbers needed to treat (NNT; Sackett et al, 1991) are 1.2 - 1.5. Thus 1.3 patients needs to be treated with eradication therapy to get a positive H pylori eradication; this is a very efficient treatment - 77 patients out of 100 would benefit.
The use of adequate antibiotic therapy results in eradication of H pylori together with cure of the ulcer Helicobacter pylori plays important roles in gastric carcinogenesis, and gastric cancer development is characterized by accumulation of various gene mutations. However, the mechanism of how H. Pylori induces gene mutations in the gastric mucosal cells is unknown. Activation-induced cytidine deaminase (AID) is exclusively expressed in B lymphocytes and is essential for somatic hypermutation of immunoglobulin genes. Here we found that AID-transgenic mice develop not only lymphomas but also gastric adenomas. Moreover, we revealed ectopic expression of AID in H. Pylori -positive human gastritis mucosa as well as in gastric cancer cells, whereas no AID expression was present in non infected mucosa. In vitro studies showed that AID protein as well as Mrna was induced by H. Pylori infection in association with induction of various p53 gene mutations in human gastric epithelial cells. H. Pylori -induced AID expression was blocked by NF-B inhibition. Furthermore, AID gene introduction into gastric mucosal cells accelerated p53 gene mutations, and inhibition of AID using sRNA significantly reduced H. Pylori -induced p53 gene mutations. Finally, in H. Pylori -infected human gastric mucosa, high AID expression levels were associated with frequent p53 gene
mutations, whereas in H. Pylori -negative subjects, no or low AID expression was accompanied by no or low p53 gene mutation frequencies. Thus, AID appears to play important roles in H. Pylori –induced gastric carcinogenesis by enhancing various gene mutations in the gastric mucosal cells
Since cure ofH. Pylori infection decreases recurrence rates and facilitates healing,antibiotic therapy is indicated for all H. Pylori-infected ulcer patients.No optimal, simple antibiotic regimen has yet emerged. Simultaneousconventional ulcer therapy is recommended to facilitate symptom relief andhealing. For refractory ulcers, only maximal acid inhibition offersadvantage over continued conventional therapy; cure of H. Pylori infectionis likely to facilitate healing of refractory ulcers. Only with complicatedor refractory ulcers should conventional maintenance therapy be continued,at least until successful H. Pylori eradication is confirmed. A search forNSAID use is indicated for all ulcer patients. For NSAID-associated ulcersthese drugs should be discontinued if possible and H. Pylori, if present,should be cured. Together our data suggest that H pylori induces a regulatory T cell response, possibly contributing to its peaceful coexistence with the human host, and that ulcers occur when this regulatory response is inadequate.
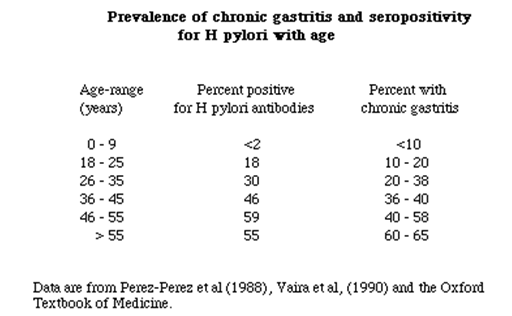
H. Pylori infection induces ectopic AID expression in the gastric mucosal cells via NF-B activation. Thus, AID appears to play important roles in H. Pylori –induced gastric carcinogenesis by enhancing various gene mutations in the gastric mucosal cells. To address the hypothesis that the human acquired immune response to H pylori influences pathogenesis, The scientists characterised the gastric T helper (Th) and regulatory T cell (Treg) response of infected patients [38]. H.pylori prevalence varied depend upon the age group as given in the table:
4. FUTURE PERSPECTIVES:
Our work aims to understand why some people infected with Helicobacter pylori develop stomach ulcers or gastric cancer, whilst others remain completely symptom-free. How h.pylori is involved in the induction of the peptic ulcer still have not been established. The chemokines interleukin (IL)-8 and macrophage inflammatory protein-1 (MIP-1) are related to the ulcerogenesis in peptic ulcer patients in organ cultures and the numbers of inflammatory cells infiltrating the lamina propria by using the mucosal tissues obtained from gastric ulcer (GU) patients with and without H. pylori infection. By using data basis analysis we determine that how the chemokines are related to the peptic ulcer[5]. The standard treatment regimen for H. pylori uses 2 antibiotics and a PPI. Many studies, however, suggest that a 7-day treatment may work just as well. A report published evaluated a shorter course of treatment using the PPI rabeprazole and 2 antibiotics. They found that a 4-day treatment eliminated H. pylori and was associated with fewer side effects. A study published comparing 1- and 2-week treatments with amoxicillin, clarithromycin, and omeprazole for H. pylori eradication found both regimens to be similar in efficacy, safety, and compliance[16].Treatment regimes which have been shown in randomized controlled trials (RCTs) to be most effective for the treatment of peptic ulcer is being anlysed[36].The antibiotic regimens and other treatment regimens are being analysed and the prevalence of the disease in smokers and non-smokers is checked by my forthcoming work.
5. REFERENCES
1. "Peptic Ulcer: Peptic Disorders: Merck Manual Home Edition
2. wikipedia.org/wiki/Image:Deep_gastric_ulcer.png
3. Kim YH, Lee JH, Lee SS, et al (2002). "Long-term stress and Helicobacter pylori infection independently induce gastric mucosal lesions in C57BL/6 mice". Scand. J. Gastroenterol
4. Tatsuji Shimizua; Kazuo Kusugamia et al; Helicobacter pylori-Associated Gastric Ulcer Exhibits Enhanced Mucosal Chemokine Activity at the Ulcer Site; Digestion journal of gastroenterology Vol. 62, No. 2-3, 2000
5. F. Franceschi, D. Roccarina, G. Gigante,B. Giupponi,G. De Marco,F. Barbaro, G. Niccoli, G. Lanza,G. Sgueglia,L. Altamura, Department of Emergency,Rome, Italy; Cardiology, Rome, Italy
6. T. Chiba, Y. Matsumoto, Y. Endo & H. Marusawa Department of Gastroenterology and Hepatology, Kyoto University, Kyoto, Japan
7. Van Der Weyden MB, Armstrong RM, Gregory AT (2005).Department of Histopathology, University of Nottingham, Queens Medical Centre, Nottingham, UK
8. Medical Sciences, Gardiner Institute, Western Infirmary, University of Glasgow, Glasgow, G11 6NT, UK.
9. Goer A, Gothe H, Schiffhorst G, Sterzel A, Grass U, Haussler B. Pharmacoepidemiol Drug Saf. 2007 Feb 26
10. Jansson EA, Petersson J, Reinders C, et al.2007-2008 Ayushveda Informatics India Pvt Ltd. All Rights Reserved
11. Ohkusa1; Takashimizu1; Fujiki1; Araki1; Ariake1; Shimoi1; Honda1; Enomoto1; Sakurazawa1; Horiuchi1; Suzuki1; Ishii1; Ishikura1 Alimentary Pharmacology & Therapeutics, Volume 12, Number 5, May 1998 , pp. 457-461(5)
12. Tsunehisa; YAMADA Hiroshi; et al Therapeutic effects of ecabet sodium, an antiulcer drug, on dextran sodium sulfate-induced ulcerative colitis in rats; Discovery & Pharmacology Research Laboratories, Toda, Saitama, JAPON
13. National Digestive Diseases Information Clearinghouse (niddk.nih.gov)
14. American Gastroenterological Association (gastro.org).
15. Field SK, Sutherland LR. Does medical antireflux therapy improve asthma in asthmatics with gastroesophageal reflux: a critical review of the literature. Chest 1998;114:275–283.
16. Donnellan C, Sharma N, Preston C, et al. Medical treatments for the maintenance therapy of reflux oesophagitis and endoscopic negative reflux disease. Cochrane Database Syst Rev 2005;2:CD003245.
17. Redefining the Role of Surgery for Perforated Duodenal Ulcer in the Helicobacter pylori Era; Annals of Surgery. 231(2):159, February 2000.
18. Helicobacter pylori Foundation (www.helico.com).
19. Centers for Disease Control and Prevention (www.cdc.gov)
20. Cullen DJ, Hawkey GM, Greenwood DC, et al (1997). "Peptic ulcer bleeding in the elderly: relative roles of Helicobacter pylori and non-steroidal anti-inflammatory drugs". Gut 41 (4): 459–62. PMID 9391242. PMC:1891536
21. Van Der Weyden MB, Armstrong RM, Gregory AT (2005). "The 2005 Nobel Prize in physiology or medicine". Med. J. Aust. 183 (11–12): 612–4. PMID 16336147
22. DeBakey, M.: Acute perforated gastroduodenal ulceration.Surgery8:1028,8:852 1940
23. Svanes, C., Lie, R.T., Kvåle, G., Svanes, K., Søreide, O.: Survival after peptic ulcer perforation: a time trend analysis. J. Clin. Epidemiol.49:1363, 1996
24. Mikulicz, J.: Ueber Laparotomie bei Magen und Darmperforation.Samml. Klin. Vort. Leipzig 262:2307, 1885
25. Von Haberer, H.: Zur Therapie akuter Geschwursperforationen des Magens und Duodenums in die freie Bauchhohle. Wien Klin. Wochnschr. 32:413, 1919
26. Jordan, P.H., Jr., Korompai, F.L.: Evolvement of a new treatment for perforated duodenal ulcer. Surg. Gynecol. Obstet. 142:391, 1976
27. Boey, J., Branicki, F.J., Alagaratnam, T.T., Fok, P.J., Choi, S., Poon,A., Wong, J.: Proximal gastric vagotomy: the preferred operation for perforations in acute duodenal ulcer. Ann. Surg. 208:169, 1988
28. Taylor, H.: Perforated peptic ulcer: treated without operation. Lancet 2:441, 1946
29. Seeley, S.F., Campbell, D.: Nonoperative treatment of perforated peptic ulcer: a further report. Surg. Gynecol. Obstet. 102:435, 1956
30. Svanes, C., Espehaug, B., Salvesen, H., SØreide, O., Svanes, K.: A multifactorial analysis of factors related to lethality following treatment of perforated gastroduodenal ulcer 1935–85. Ann. Surg. 209: 418, 1989
31. Boey, J., Choi, S.K.Y., Alagaratnam, T.T., Poon, A.: Risk stratification in perforated duodenal ulcers. Ann. Surg. 205:22, 1987
32. Irvin, T.T.: Mortality and perforated peptic ulcer: a case for risk stratification in elderly patients. Br. J. Surg. 76:215, 1989
33. Svanes, C., Salvesen, H., Espehaug, B., Svanes, K., Søreide, O.: Perforated peptic ulcer: an analysis of the increase in treatment delay 1935–85. Surg. Res. Commun. 6:181, 1989
34. Svanes, C., Salvesen, H., Bjerke Larssen, T., Svanes, K., Søreide, O Trends in and value and consequences of radiologic imaging of perforated gastrodeuodenal ulcer. Scand. J. Gastroenterol. 25:257, 1990
35. Alimentary Pharmacology & Therapeutics, Volume 12, Number 5, May 1998 , pp. 457-461(5)
36. Chiba N, Rao BV, Rademaker JW, Hunt RH. Meta-analysis of the efficacy of antibiotic therapy in eradicating Helicobacter pylori. The American Journal of Gastroenterology 1992; 87: 1716-1727
37. Lind T, Veldhuyzen van Zanten SJO, Unge P, Spiller RC, Bayerdorffer E, O’Morain C, Wrangstadh M, Idstrom JP. The MACH1 study: optimal oneweek treatment for H.pylori defined; EFFECTIVENESS Matters Vol 1, Issue 2, September 1995.
38. K Robinson1,2; R Kenefeck1,2 et al; Helicobacter pylori-induced peptic ulcer disease is associated with inadequate regulatory T cell responses;Institute of Infection, Immunity & Inflammation, University of Nottingham, Centre for Biomolecular Sciences, Nottingham, UK.
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE









