About Authors:
Languluri Reddenna1*, Sree Nagavalli K2
1Department of Pharmacy Practice, Rajiv Gandhi Institute of Medical Sciences, Kadapa, Andhra Pradesh, India-516003
2Department of Pharmacy Practice, S.J.M College of Pharmacy, Chitradurga, Karnataka, India-577502
*reddennapharmd@gmail.com
{ DOWNLOAD AS PDF }
Abstract
Asthma is one of the common diseases. Asthma was a term used by the ancient Greeks to describe any condition that causes shortness of breath. Early warning signs are breathing changes, sneezing, moodiness, headache, runny/stuffy nose, coughing, chin or throat itches, feeling tired, dark circles under eyes, trouble sleeping. Asthma creates an extensive burden on individuals and families, as it is more often under-diagnosed and under-treated. World Health Organization estimates that 300 million people suffer from asthma, 2, 55, 000 people died of asthma in 2005 and over 80% of Asthma deaths were reported from low and lower-middle income countries. In India, an estimated 57,000 deaths were attributed to asthma in 2004 and it is one of the leading causes of morbidity and mortality in rural India. India had an estimated 15-20 million asthmatics. It was estimated that the number of people with asthma would grow by more than 100 million by 2025.As members of the health care team, pharmacists are in an excellent position to recognize patients who are not under the care of a physician or whose asthma will poorly controlled for a variety of reasons. Particular resources are provided to improve the care of disadvantaged groups with high morbidity, including certain racial groups and those who are poorly educated, live in large cities, or are poor and to address preventable factors, such as air pollution, that trigger exacerbations of Asthma.
REFERENCE ID: PHARMATUTOR-ART-2109
Introduction
Asthma is one of the common diseases. Asthma was a term used by the ancient Greeks to describe any condition that causes shortness of breath.[1]It is a chronic inflammatory disorder of the airways associated with increased airway hyper-responsiveness, recurrent episodes of wheezing, breathlessness, chest tightness, and coughing, particularly at night/early morning. Airway inflammation produces airflow limitation through acute bronchoconstriction, chronic mucus plugs formation and airway wall swelling or remodeling.[2] There are two general categories for classifying asthma, extrinsic and intrinsic depending upon the types of stimuli that trigger attacks.
- Extrinsic Asthma: It is caused by a type of immune system response to inhaled allergens such as pollen, animal dander or dust mite particles.
- Intrinsic Asthma: It is caused by inhalation of chemicals such as cigarette smoke or cleaning agents, taking aspirin, a chest infection, stress, laughter, exercise, cold air, food preservatives or a myriad of other factors.[3]
Early warning signs are breathing changes, sneezing, moodiness, headache, runny/stuffy nose, coughing, chin or throat itches, feeling tired, dark circles under eyes, trouble sleeping.[4]The diagnosis of asthma usually based on clinical history, objective measures of pulmonary function, and based on assessment of allergy.[5]Asthma creates an extensive burden on individuals and families, as it is more often under-diagnosed and under-treated. World Health Organization estimates that 300 million people suffer from asthma, 2, 55, 000 people died of asthma in 2005 and over 80% of Asthma deaths were reported from low and lower-middle income countries. In India, an estimated 57,000 deaths were attributed to asthma in 2004 and it is one of the leading causes of morbidity and mortality in rural India. India had an estimated 15-20 million asthmatics. It was estimated that the number of people with asthma would grow by more than 100 million by 2025.[6]The prevalence of asthma had risen over the last 30 years but now appears to be stabilized, with approximately 10–12% of adults and 15% of children affected by the disease.[7]Occupation conditions, such as exposure to fumes, gases or dust are responsible for 11% of asthma cases worldwide.[8]
People had recognized the condition for centuries, and many treatments have demanded to cure it. In fact, medicines can only control asthma, not cure it even today. Asthma medications are used to stop, control and prevent asthma symptoms. Most people need to take more than one type of medication to control asthma. There are different medications and available in tablets, aerosol inhalers, powder aerosols, liquids and injections.[9]Even though many people with asthma depend on medications to prevent and relieve symptoms, some people can do several things on their own to maintain their health and lessenthe possibility of asthma attacks. By following the below suggestions and taking medications as needed, can live a healthy, active lifestyle.[10]
- Keep home smoke free.
- Keep away from paint or strong smelling cleaning solutions such as ammonia.
- Avoid strong perfumes and hair spray.
- Keep the house well ventilated.
- Remove stuffed animals that can collect dust or wash them often or cover with plastic.
- Keep bathrooms dry and clean to prevent mold and use a dehumidifier if necessary.
- Replace filters in air conditioners because they collect dust.
- Avoid feather pillows and use synthetic materials such as Dacron.
- Avoid visits to homes with animals and do not have one in home. Select pets, such as fish, that have no dander.
- Washing hands frequently helps to prevent catching a cold.
- Avoid unnecessary exposure to colds. If likely to stir up dust, wear a mask or have someone else do the cleaning.
- Regular exercise strengthens heart and lungs, which helps relieve asthma symptoms.
- Maintain a healthy weight.
- Get plenty of sleep.
- Avoid stress.
- Vitamins and minerals will be beneficial for asthma (Vitamin- A found abundantly in carrots, pumpkin, sweet potatoes, winter squashes, cantaloupe, pink grapefruit, apricots, broccoli, and spinach. Apples, apricots, avocadoes, breadfruit, blackberries, blackcurrants, blueberries, kiwifruits, jujubes, melons, peaches and pears are rich in Vitamin-C. Vitamin-E found in wheat germ, corn, nuts, seeds, olives, spinach, asparagus, and other green leafy vegetables and vegetable oils. Brazil nuts, dried, oatmeal, brown rice, whole wheat bread, black, dried, walnuts are all selenium rich foods.[11-18]
The goals of asthma management are as follows:
- Maintain normal activity levels (including exercise and other physical activity).
- Maintain (near) normal pulmonary functions.
- Prevent chronic and troublesome symptoms (e.g., coughing or breathlessness in the night, in the early morning, or after exertion).
- Prevent recurrent exacerbations of asthma and minimize the need for emergency department visits or hospitalizations.
- Provide optimal pharmacotherapy with minimal or no adverse effects.
- Pharmacological management of asthma includes long-term management, and management of exacerbations of asthma.[19]
List of Anti- Asthmatic Medicines[20-23] It was displayed in table 1.
Combination Medications It was displayed in table 2.
Table 1- List of anti-asthmatic drugs
|
Category |
Name of the drug |
Dose |
Frequency |
|
|
Β – agonists: |
|
|||
|
Short acting agents |
Tab. Salbutamol |
2-4mg |
Tid |
|
|
Inh. Salbutamol |
100-200µg |
3-4 times daily |
|
|
|
Tab. Terbutaline |
2.5-3mg |
Tid |
|
|
|
Inh. Terbutaline |
500mcg |
Every 4-6 hours |
|
|
|
Inj. Terbutaline |
250-500mcg SC/IM |
Qid |
|
|
|
Tab. Albuterol |
2-4 mg |
Tid/Qid |
|
|
|
Inh. Albuterol |
1-2 puffs |
Every 6 hours |
|
|
|
Tab. Bambuterol |
20mg |
OD |
|
|
|
Tab. Pirbuterol |
2.5–5 mg |
Depending on severity |
|
|
|
Inh. Levalbuterol |
1-2 puffs |
Every 6 hours |
|
|
|
Long acting agents |
Inh. Salmeterol |
25µg-50µg |
Bid |
|
|
Inh. Formeterol |
12-24µg |
Bid |
|
|
|
Methyl xanthine’s |
Tab. Theophylline |
200-400mg |
Every 12 hrs |
|
|
Inj. Aminophylline |
250-500mg |
Bid |
|
|
|
Tab. Doxophylline |
400mg |
OD/BID |
|
|
|
Anti-cholinergic |
||||
|
Slow acting agents |
Inh. Ipratropium bromide |
20-40µg |
4 times daily |
|
|
Long acting agents |
Inh. Tiotropium bromide |
18 µg |
Od |
|
|
Corticosteroids |
|
|||
|
Inhalations |
Inh. Beclomethasone |
100-400µg |
BID |
|
|
Inh. Budesonide |
200-400µg |
BID |
|
|
|
Inh. Ciclesonide |
80-160 µg |
OD |
|
|
|
Inh. Fluticasone |
200-500µg |
BID |
|
|
|
Inh. Flunisolide |
250 mcg/puff |
Bid |
|
|
|
Systemic drugs |
Inj. Hydrocortisone |
100-200mg |
Bid |
|
|
|
Tab. Prednisolone |
40-50mg |
OD |
|
|
Tab. Methyl-prednisolone |
2-32 mg. |
Od |
||
|
|
||||
|
Leukotrienes modifiers |
Tab. Montelukast |
10 mg |
Od (in evening) |
|
|
|
Tab. Zafirlukast |
20mg |
OD |
|
|
Immuno modulators |
Omalizumab |
42mg/vial |
OD |
|
|
Mast cell stabilizers |
Inh. Sodium Cromoglycate |
2-10mg |
Tid |
|
Table 2-Combination Medications
|
Combination of drugs |
Brand name |
Doses |
|
Budesonide + Formoterol |
Forecourt |
100mcg+6mcg(inhalation) |
|
Tiotropium bromide + Formoterolfuarate |
Duovarotacaps |
18mcg+12mcg(inhalation) |
|
Beclomethasonedipropionate + Salbutamol |
Aerocort |
100mcg+100mcg(inhalation) |
|
Levosalbutamol + Iprtropium bromide |
Duolin |
50mcg+20mcg/puff(inhalation) |
|
Etophylline + Theophylline |
Deriphylline |
77mg+23mg |
Educate patients about asthma medications
Pharmacists can help patients understand that, with appropriate therapy, most patients can lead normal, productive, and physically active lives. Preventive medication should take on a regular basis even when the patient is free of symptoms and includes inhaled anti-inflammatory agents such as corticosteroids, cromolyn and nedocromil as preferred therapy.
Instruct patients about the proper techniques for inhaling medications
Inhaled medications are preferred over oral therapies. Improper MDI technique can be one cause of a poor response to therapy. Patients using inhalation therapies need careful instruction, including systematic demonstration at the time of dispensing the medication, and observation of their technique. Patients reminded that the most important steps in a proper MDI technique are gentle exhalation before breathing in, a slow inhalation and holding the breath. Spacers were habitually indicated for most patients using a corticosteroid MDI because they improve particle deposition in the lungs and decrease local side effects such as thrush and hoarseness. Usage of metered dose inhaler was explained in figure 1.
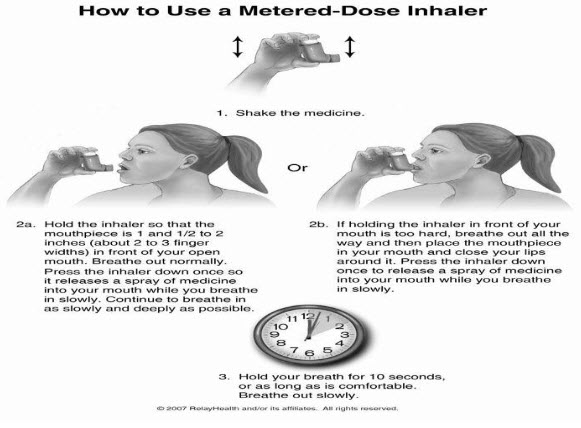
Figure 1-Usage of Metered Dose Inhaler
Monitor medication use and refill intervals to help identify patients with poorly controlled asthma
During symptomatic periods, selective short acting inhaled beta2-agonists may be sufficient to relieve asthma symptoms. When asthma is stable, it is better to use these agents on an as-needed basis. During an exacerbation, patients may increase the dose and/or frequency of use, which may lead to a delay in seeking appropriate medical care. Pharmacists may find indications of chronic overuse of short-acting inhaled beta2-agonists by checking patient’s medical history and the frequency of refills Pharmacists should also monitor for overuse of a long-acting beta2-agonist. In general, these agents should not be used more than twice a day and are not appropriate to relieve acute symptoms. Physicians will consider several factors when deciding whether to initiate or increase anti-inflammatory therapy. Wide-ranging, a short course of oral corticosteroids may be indicated if the excessive use of an MDI is short term; due to an acute, severe episode; or the result of an isolated exacerbation caused by a common cold or other upper respiratory tract infections. Refilling the prescription at intervals longer than indicated by the directions for use on the prescription may indicate nonadherence.
Encourage patients purchasing OTC asthma inhalers or tablets to seek medical care.
Asthma is one of the few possibly fatal diseases for which OTC products are available for self-treatment. Use of OTC inhalers may lead to a delay in seeking appropriate medical care. Pharmacists should state anyone using an OTC product for respiratory symptoms to a physician for diagnosis, regular monitoring, and proper treatment. The physician can then determine the need for other therapies, such as an inhaled anti-inflammatory agent to prevent symptoms. In general, bronchodilators are less effective and cause more side effects when administered by the oral route and combinations of theophylline and ephedrine have the potential to cause synergistic toxicity.
Help patients use peak flow meters appropriately
The peak expiratory flow rate is the greatest flow velocity that can be obtained during a forced expiration starting with fully inflated lungs. It provides a simple, quantitative, and reproducible measure of airway obstruction with a relatively inexpensive device that is available without a prescription. The peak expiratory flow rate is used to assess the severity of asthma as a basis for adding medication, monitoring response to chronic therapy, and detecting deterioration in lung function before symptoms develop. The physician may consider more hostile therapy if the patient’s highest value is less than 80 percent of predicted value and/or daily variability is more than 20 percent.
Help patients discharged from the hospital understand their asthma management plan
Pharmacists discuss a plan with a patient before discharge, reinforcing and clarifying instructions that are designed to prevent subsequent hospitalizations or emergency department visits. Pharmacists can review the patient’s inhaler and peak flow meter technique and provide instruction, if needed.
Criteria indicate the need for medication adjustment, improved medication administration technique, or patient education concerning asthma and its management as follows:
- Adverse effects from medications
- Waking up at night from symptoms of asthma more than twice a month
- Increased use of inhaled, short-acting beta2-agonists (e.g., more than three to four times in 1 day)
- Long-term overuse of inhaled, short-acting beta2-agonists (e.g., refilling the prescription more often than one canister/month or more than one canister/2 months of a short-acting agent when it is used in addition to a long-acting agent).
- Overuse or misuse of inhaled long-acting beta2-agonists.
- Nonadherence to anti-inflammatory medications (e.g., refilling the prescription less than half as often as would be required if the directions on the prescription were followed)
- Failure to achieve quick and sustained response (i.e., beginning within 10 to 20 minutes and lasting longer than 3 to 4 hours) to short-acting beta2-agonists during an acute asthma episode (as measured by a decrease in symptoms or an increase in peak expiratory flow rate).
- Poor tolerance to physical activity (i.e., the patient experiences symptoms of exercise-induced asthma)
- An emergency department visit or hospitalization for asthma
Written guidelines
- Specific instructions about use of medications, including dose, frequency of administration, guidelines for changing dose or adding medications if appropriate, and adverse effects to report to the clinician.
- The importance of long-term preventive medications
- How to monitor body signs or symptoms and/or PEFR to detect increasing airflow obstruction as early as possible; early signs of airflow obstruction vary according to the individual and should be identified for each patient.
- Criteria for initiating or modifying treatment: a drop in PEFR or early signs or symptoms
- List of steps to take in managing an acute asthma episode (i.e., remove the precipitating trigger, give medication, avoid strenuous physical activity, and keep patient and family calm).
- Specific criteria for seeking emergency medical care, including a pattern of declining PEFR; failure of medications at home to control worsening symptoms; difficulty in breathing (wheeze may be absent), walking, or talking; intercostal retractions; blue fingernails or lips.
- Observable signs that long-term therapy is less than optimal, such as asthma symptoms that cause sleep interruption, consistently low or highly variable PEFR, and/or too frequent use of short-acting inhaled beta2-agonists. Such signs should be promptly discussed with the clinician.[24-34]
The present review was undertaken to evaluate the incidence, prevalence, risk factors, treatment and impact of patient counseling in asthmatic patients.Kabila. B et al, [35]was conducted a study on risk factor assessment study for bronchial asthma among the rural people at rural health centre through a uniform methodology of questionnaire. Asthma was diagnosed if the respondent answered positively to (a) Wheezing or chest tightness or breathlessness (b) worsening of symptoms in morning and night. (c) Having suffered from asthma or having an attack of asthma in past two months or using past medication for respiratory problems. Besides demographic data, information on smoking habits, alcohol consumption, occupational influence and family history suggestive of asthma was also collected. More predominant risk factor is dust and concluded that keeping the house clean is the preventive measure undertaken by most of the people.
Tarig Hakim Merghaniet al,[36] was conducted a study on knowledge, attitude and behavior of asthmatic patients regarding asthma in urban areas regarding their acceptance of the diagnosis of asthma, use of inhalers, compliance to preventers and trial of non-medical methods for treatment. A sample of 490 asthmatic patients, 52% males and 48% females, was selected randomly from three major hospitals.The principal triggering factors known to the patients were dust (in 78%) and upper respiratory tract infections (in 67%). The diagnosis of asthma was refused by 27% of patients who preferred to be described as allergic rather than asthmatic. Most patients in this study (88%) used inhalers for treatment of asthma attacks whereas 12% were reluctant to use inhalers. About 44% of asthmatic patients tried non-medical methods for the purpose of cure. Asthmatic patients have poor knowledge about the pathogenesis of asthma, especially the inflammatory nature of the disease. More than a quarter of them are reluctant to accept the diagnosis of asthma and prefer to be described as allergic. Jaime Correia de Sousaa,et al [37]conducted a study on asthma incidence and accuracy of diagnosis using standardized diagnostic criteria. Symptom frequency and diagnoses of asthma were tabulated. Diagnostic accuracy was computed by dividing the rate of asthma diagnosis by the true rate using established diagnostic criteria. The diagnosis was confirmed in 260 cases, giving a true incidence rate of 2.02/1000/year (95% confidence interval 1.8 to 2.2) and an accuracy of diagnosis 84%. Asthma incidence approaches published rates if accepted criteria are used. Educational efforts to ensure diagnosis that is more accurate may improve outcomes for asthma patients.
J Liebhart, et al[38] conducted a study on prevalence and risk Factors for asthma. The prevalence of asthma depends on both hereditary and environmental factors. Knowledge of the effects of environmental and congenital factors on the frequency of occurrence of asthma may provide important clues to its pathogenesis and prevention. The overall prevalence of asthma was 8.6% (95% confidence interval [CI], 7.7% – 9.6%) among children and 5.4%,95% CI, 5.0% – 5.8%) among adults. Several risk factors for asthma were identified: family history of asthma, black smoke, residential exposure to traffic-related air pollution in both children and adults, and damp or overcrowded housing in adults. No statistically significant association was observed for passive smoking in the home, use of gas stoves, pet ownership, or exposure to ambient air pollution with sulfur dioxide. The prevalence of asthma is associated with several host and environmental factors.C G Barnard et al [39] conducted a study to assess the significance of individual risk factors in the development of occupational asthma of aluminium smelting (OAAS). The risk of OAAS was more than three times higher in individuals with an FER of 70.0–74.9% than in individuals with an FER >80.0% (adjusted OR 3.46, 95% CI 1.01 to 11.89). Individuals with hay fever may be more susceptible to occupational asthma when exposed to airborne irritants in aluminium smelting. The pathological basis may be reduced nasal filtration and increased bronchial hyperresponsiveness.
MarijaCrnc evic´ Ureket al [40] conducted a study to investigate the effectiveness of different educational programs in obtaining better asthma control and asthma-related quality of life (QoL). The improved average asthma symptom score and decreased utilization of the rescue medication were documented in all groups without significant differences among them. We also found significant improvements in both morning and evening PEFR in IVI group as well as in the morning PEFR in AS group. They conclude that among tested educational interventions the AS caused the best improvement in QoL while IVI produced the best overall response in both parameters of the asthma control and QoL. Peter G. Gibson [41] conducted a study on asthma education. Asthma self-management education which consists of information, self-monitoring, regular medical review, and a written action plan is effective and leads to a reduction in hospitalization and ER(emergency) visits for asthma. While a structured asthma self-management programme is effective in a hospital setting, attempts to deliver these programmes in primary care have met with varying success. Andrew G [42] suggests that 50% of patients with asthma do not follow physician medication recommendations. To examine the rationale for making available objective medication adherence monitors for physicians to improve the quality of care for patients with severe persistent asthma. Patients with severe asthma are at risk for nonadherence because of the use of multiple medications to control symptoms, coexisting disease states, the occurrence of depression and anxiety and the high cost of care. Research studies have demonstrated the effectiveness of objective monitoring as part of multiple clinical strategies to improve adherence and reduce morbidity and the cost of asthma care. By correctly assessing nonadherence as the cause of treatment failure in patients with not only severe asthma but mild and moderate disease as well, practicing physicians may improve the quality of care provided.
Prabhakaran et al [43] conducted a study to distinguish knowledge, inhaler technique and compliance to treatment. There was significant improvement in knowledge aspects (ability to identify rescue medication[p-value is 0.031],different stimuli can trigger asthma symptoms [p-value is 0.016], peak flow meter is used for monitoring asthma [p-value is 0.004], asthma symptoms are caused by airway swelling/ narrowing [p-value is less than 0.001], steroid inhaler are to be used daily as preventive therapy [p-value is less than 0.001], self-reported inhaler compliance (number of puffs per administration [p-value is less than 0.001] per day [p-value is less than 0.001]) and in inhaler technique [p-value is 0.001]. There was also significant reduction in emergency department attendances (p-value is less than 0.001) and hospital admissions (p-value is less than 0.001). This study demonstrated the effectiveness of an asthma education programme in patients hospitalized for asthma exacerbation. Vijaya Kumar. S [44] was conducted a study by using WHO-based prescription-auditing performa and found that combination therapy (80%) was given to a significant number of patients as compared to monotherapy (20%). In combination therapy, the two-drug combination was the most often prescribed (57.69%). Further, anti-asthmatic drugs was mostly given (68.18%) by the oral route, followed by inhalation route (27.27%) and injection route (4.55%). The asthmatic problem was more prevalent in grade-III employees like drivers and laborers and concluded that study may be more meaningful. Further,improve the prescribing as well as dispensing practices of the pharmacist through successful implementation of interventional programs in health centers.Awinashpandey[45] conducted a study to establish the drug-prescribing trend of anti-asthmatic drugs and suggested that β-agonist (40%) were the most frequently prescribed anti-asthmatic drugs followed by Methylxanthine (27%), corticosteroids (25%), leukotriene antagonist (4.4%) and anti-histaminics (3.6%) was the least prescribed. Analysis of prescription revealed that multiple drug therapy (81%) was opted for a significant number of patients as compared to single drug therapy (19%). Conflicting to popular belief, oral dosage form tablets (56.3%) were preferred over inhalation (33.8%). It can be concluded that the present prescribing pattern of anti-asthmatics does not completely meet standard guidelines of asthma treatements.
Roberto Cano-De La Cuerda,et al [46] conducted a study on Effectiveness of Therapeutic Education and Respiratory Rehabilitation Programs for the Patient with Asthma. Educating asthmatic patients and their families is essential for therapeutic intervention. Complete continuous, dynamic and adaptive education, changes in attitudes and behaviors of the patient and family can be achieved and will undoubtedly lead to an improvement in their quality of life. Among other non-pharmacological interventions, respiratory rehabilitation is an alternative treatment and primarily aimed at patients with moderate to severe asthma.
The study concludes that the most predominant risk factors were dust, smoke and climate variation.Most of the people using multiple drugs for treatment due to severity and comorbid diseases compared to single drug, combination therapy. Single drugs and combination therapy was used by mild and moderate asthma patients. As per patient counseling point of view, most patients have inadequate knowledge about disease, use of medication (inhalers),irregular visits to physician and finally most patients not following preventive measures given by physician and clinical pharmacist. However, most patients have knowledge about disease, preventive measures and risk factors. The burden of Asthma in India is of necessary degree to warrant its recognition as a priority in government health strategies. Particular resources are provided to improve the care of disadvantaged groups with high morbidity, including certain racial groups and those who are poorly educated, live in large cities, or are poor and to address preventable factors, such as air pollution, that trigger exacerbations of Asthma.
References
1.Joseph t. Dipiro - pharmacotherapy- sixth edition- publication 1999- chapter 26- page no.: 503- 535
2.Global initiative for asthma- updated 2010. Available from: ginasthma.org
3.sancd.org/uploads/pdf/Asthma_factsheet.pdfs
4. nationaljewish.org
5.Herfindal text book of therapeutics- drug and disease management. chapter 34.2006.
6.World health organization. Global surveillance, prevention and control of chronic respiratory diseases: a comprehensive approach, 2007
7.Harrison’s principles of internal medicine- 17th edition- published in 2008- chapter 248
8.World health organization. Global surveillance, prevention and control of chronic respiratory diseases: a comprehensive approach, 2007
9. medical-exam-essentials.com/current-asthma-treatment.html
10.Global initiative for asthma- updated 2010 (ginasthma.org)
11.Herfindal text book of therapeutics- drug and disease management- 2006th year edition- chapter 34.
12. ehow.com
13. aaaai.org -- American Academy of Allergy, Asthma & Immunology
14.Kabila B, Sankar V- Risk factor Assessment Study For Bronchial Asthma among the Rural People- Indian Journal of Pharmacy Practice- Volume 4- Issue 3- Jul to Sep, 2011
15.Voices.yahoo.com/prevent-asthma-attacks-through-diet-l... - united states 10 oct 2009
16.Tricia M. McKeever - 2004 The American Thoracic Society- Accepted July 12, 2004 (atsjournals.org)
17. webmd.com/asthma/guide/asthma-diet-what-you-should-know
18.asthma.about.com/od/asthmacam/a/asthma_diet.html
19.Global initiative for asthma- updated 2010 (ginasthma.org)
20.29. KD Tripathi – Essentials Of Medical Pharmacology- 6th Edition- 2010 publication, Chapter 16- page No.: 213-237
21.Drug Today – January to March 2012- Volume II- Page No.: 893-913
22. CIMS- Jan to April. 2012- Page No.: 134- 152 ( cimsasia.com)
23.British National Formulary- March 2010- Page No.: 163- 185 (bnf.org)
24.National Center for Health Statistics. Current estimates from the National Health Interview Survey: United States. Vital and Health Statistics. Series 10. Washington, D.C. U.S.Government Printing Office. Issues from 1985-1993.
25.Weiss KB, Gergen PJ, Hodgson TA. An economic evaluation of asthma in the United States. New England Journal of Medicine 1992; 326:862-6.
26.Asthma—United States: 1980-90. Morbidity and Mortality Weekly Report 1992; 41:733 5.
27.National Heart, Lung, and Blood Institute, National Asthma Education Program, Expert Panel Report. Guidelines for the Diagnosis and Management of Asthma. NIH Publication No. 91-3042, August 1991.
28.Self TH, Brooks JB, Lieberman P, Ryan MR. The value of demonstration and role of the pharmacist in teaching current use of pressurized bronchodilators. Canadian Medical Association Journal 1983; 128:129-31.
29.Kesten S, Zive K, Chapman KR. Pharmacist knowledge and ability to use inhaled medication delivery systems. Chest 1993; 104:1737-42.
30.De Blaquiere P, Christensen DB, Carter WB, Martin TR. Use and misuse of metered-dose inhalers by patients with chronic lung disease. American Review of Respiratory Diseases 1989; 140:910-6.
31.Hindle M, Newton DA, Chrystyn H. Investigations of an optimal inhaler technique with the use of urinary salbutamol excretion as a measure of relative bioavailability to the lung. Thorax 1993; 48(6):607-10.
32.Executive Committee, American Academy of Allergy and Immunology. Inhaled betaadrenergic agonists in asthma. Journal of Allergy and Clinical Immunology 1993; 91:1234-7.
33.Larsson S, Svedmyr N. Bronchodilating effect and side effects of beta2-adrenoceptor stimulants by different modes of administration (tablets, metered aerosol, and combinations thereof). American Review of Respiratory Diseases 1977; 116:861-9.
34.Weinberger M, Bronsky E. Interaction of ephedrine and theophylline. Clinical Pharmacology and Therapeutics 1975; 17:585-92.
35.Kabila B, Sankar V- Risk factor Assessment Study For Bronchial Asthma among The Rural People- Indian Journal of Pharmacy Practice- Volume 4- Issue 3- Jul to Sep, 2011
36.Tarig Hakim Merghani - Knowledge, attitude and behaviour of asthmatic patients regarding asthma in urban areas in Khartoum State, Sudan- Khartoum Medical Journal (2011)- vol.04No.:1- Page No.:524-531
37.Jaime Correia de Sousaa,- Asthma incidence and accuracy of diagnosis in the Portuguese sentinel practice network- Primary Care Respiratory Journal (2010); 19(4): 352-357
38.LiebhartJ et al - “Prevalence and Risk Factors for Asthma in Poland: Results From the PMSEAD Study” - J InvestigAllergol Clin Immunol 2007; Vol. 17 (6): 367-374
39.Barnard C G et al - “Assessing individual employee risk factors for occupational asthma in primary aluminium smelting” - Occup Environ Med 2004;61:604–608. doi: 10.1136/oem.2003.009159
40.MarijaCrnc evic´ Ureket - “Effect of educational programs on asthma control and quality of life in adult asthma patients” - Patient Education and Counseling 58 (2005) Page No.:47–54
41.Peter G. Gibson - “Asthma education” - Respiratory Medicine (2003) 97, 1036–1044
42.Andrew G - “Should patients with persistent severe asthma be monitored for medication adherence?” - VOLUME 94, FEBRUARY, 2005- Ann Allergy Asthma Immunol. 2005;94:251–257.
43.PrabhakaranL et al - Impact of an asthma education programme on patients’ knowledge, inhaler technique and compliance to treatment - Singapore Med J 2006- 47(3)- Page No.:225-231
44.Vijaya KumarS - Drug utilization and prescription monitoring of asthma patients- Young Pharmacists 2009- Year : 2009 | Volume : 1 | Issue : 2 | Page : 180-183
45.AwanishPandey- Prescription Pattern in Asthma Therapy At Gorakpur Hospitals Lung India- volume 7- Issue1 – Jan-March 2010(lungindia.com)
46.Roberto Cano-De La Cuerda,et al conducted a study on Effectiveness of Therapeutic Education and Respiratory Rehabilitation Programs for the Patient with Asthma- Arch Bronconeumol. 2010;46(11):600-606
|
PharmaTutor (ISSN: 2347 - 7881) Volume 2, Issue 2 Received On: 25/012/2014; Accepted On: 20/01/2014; Published On: 10/02/2014 How to cite this article: L Reddenna, S Nagavalli, Management of Asthma: Role of Clinical Pharmacist, 2014, 2(2), 124-133 |
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE









