 About Authors:
About Authors:
1Robin Sharma*, 1Ajay Kumar, 2Dr. Bharat Prashar
1M.Pharm (Pharmacology)
2Head of Pharmacy Department
Manav Bharti University, Solan.
*sharmarobin@hotmail.com
ABSTRACT
Postoperative adhesions are a significant health problem with major implications on quality of life, health care and expenses on treatment. The purpose of this review was to investigate the incidence of post operative adhesions and the treatment measures such as efficacy of preventative techniques and adhesion barriers. The National Library of Medicine, Medline and A-Z databases were used to identify articles related to postoperative adhesions. Ileal pouch–anal anastomosis, open colectomy, and open gynecologic procedures are associated with the highest risk of adhesive small-bowel obstruction (class I evidence). Based on expert opinion (class III evidence) intraoperative preventative principles, such as meticulous haemostasis, avoiding excessive tissue dissection and ischemia, and reducing remaining surgical material such as powdered gloves have been published. Laparoscopic techniques, result in fewer adhesions than laparotomy techniques (class I evidence). Available bioabsorbable barriers, such as hyaluronic acid/carboxymethylcellulose, have been shown to reduce adhesions (class I evidence). Postoperative adhesions are a significant health problem after the surgery. General intraoperative preventative techniques, laparoscopic techniques, and the use of bioabsorbable mechanical barriers in the appropriate cases reduce the incidence and severity of peritoneal adhesions and post operative adhesions.
[adsense:336x280:8701650588]
Reference Id: PHARMATUTOR-ART-1435
Introduction
Adhesions are fibrous bands that connect anatomic sites at locations where there should not be connections. Post-operative adhesions account for more than 90% of the total intra-abdominal adhesions [1-9]. The development of post-operative adhesions after upper and lower abdominal surgery is part of the daily life of every digestive surgeon. Despite this, there are very few good quality longitudinal studies that permit an appreciation of the frequency of adhesion formation or of adhesion-related complications. Meanwhile post-operative adhesions are the cause of considerable direct and indirect morbidity, and their prevention can be considered a major public health issue. And yet, in France at this time, there is no validated recommendation neither concerning the prevention of adhesions, more particularly, concerning the use of a variety of commercial anti-adhesion products that have been marketed for at least a decade. Intraperitoneal adhesions develop between deperitonealized surfaces of abdominal organs, mesenteries, and the abdominal wall; the most common site of adhesion formation is between the greater omentum and the anterior abdominal wall [10,11]. Despite the frequency of adhesions and their direct and indirect consequences, there is only one published recommendation (from the gynecologic literature) concerning the prevention of peritoneal adhesions [12]. Faced with a very heterogeneous literature, it was proposed that a working group review the literature and provide answers to four questions:
· What factors contribute to the formation of adhesions? (pathophysiology, types of interventions);
· What is the incidence of post-operative adhesions? (after upper or lower abdominal surgery, after laparotomy or laparoscopy);
· What are the medical and surgical consequences of post-operative adhesion formation? (direct and indirect consequences);
· What measures are available to prevent post-operative adhesions? (surgical technique and pharmacologic methods)
[adsense:468x15:2204050025]
Incidence of adhesions
An assessment of how many people develop adhesions after surgery was performed in a post-mortem series by Weibel and Majno in 1973 [13]. In cadavers with no preceding abdominal surgery, adhesions were found in 28%, and in those that had had abdominal surgery 67% had adhesions. Where minor abdominal surgery had been performed, adhesions were present in about 50%. If major surgery had been undertaken adhesions were present in 76%, and in cases of multiple abdominal surgery 93% had adhesions present. The incidence of adhesions in a live population has been examined [10]. Inflammatory adhesions in patients who had not undergone any preceding abdominal surgery were found to be present in 10%. In patients who had had previous abdominal surgery, postoperative adhesions were found in 93% and inflammatory adhesions in 20%. Congenital adhesions were identified in less than 1%. The difference in the incidence of adhesions between the two studies is due to a difference in the age groups between the post-mortem and live studies. In the post-mortem study inflammatory adhesions were rarely seen in those under the age of 60 years. The mean age of patients without earlier abdominal surgery in the live study was 63 years. In patients who had had surgery the mean age was 75 years and therefore they were far more likely to have had intra-abdominal inflammatory episodes that resulted in adhesions, such as cholecystitis and diverticulitis.
Economical Burden of Adhesions
Problem associated with post operative adhesions pose a significant financial burden as they increase the surgical work load and utilize limited health resources [14]. Awareness concerning economical consequences resulting from adhesions is rising [15]. A Swedish study estimated the cost incurred for total care, including sick leave expenditure, for adhesive small bowel obstruction was at least US $ 20 million a year. Another study in United States looked at 1988 cases of abdominal adhesions associated complications and found that hospitalization and treatment cost was up to US $ 1.2 billion [16]. These studies did not include out patients and indirect cost such as loss of function due to long term disabilities. Although these added costs due to adhesions do not apply to cardiac surgery, they are very evident in other specialities such as general surgery.
Physiology and Physiopathology
The mechanism of adhesion formation is largely due to insufficient fibrinolysis at the site of visceral or parietal peritoneal injury resulting in incomplete resorption of local fibrinous deposits [17,18]. Thus, post-operative adhesions are the consequence of abnormal peritoneal cicatrisation: the lack of early post-operative fibrinolysis (in the first 48 hours) allows cellular infiltration of the initial fibrinous matrix. This leads to the formation of adhesions that, by the seventh day, are composed of an extracellular collagenous matrix infiltrated by fibroblasts (occasionally associated with painful nerve endings), smooth muscle cells, and neovascularization; this assemblage is coated with a mesothelial lining. Technical operative factors resulting in tissue trauma (electrocoagulation, ultrasonic tissue transection, laser energy versus sharp dissection with scissor and scalpel) [19,20] as well as residual microscopic or larger foreign bodies are determining risk factors for adhesion formation [21].
Intra-abdominal infections with inflammation and radiation tissue damage also contribute to adhesion formation. Finally, the presence of hemoperitoneum seems to potentiate adhesion formation in conjunction with the above-mentioned factors.
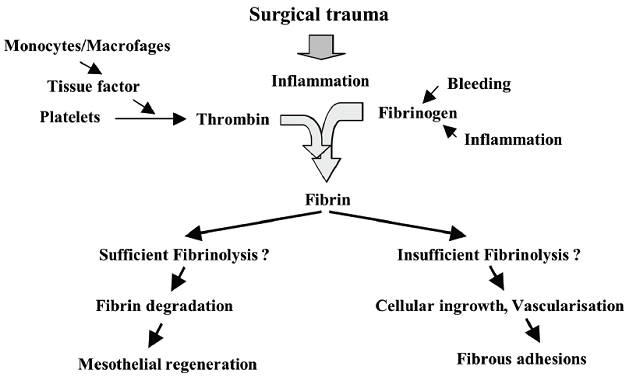
Figure 1 : A schematic illustration of process in adhesion formation.
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org
Subscribe to PharmaTutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
Incidence of Postoperative Adhesions
The frequency of peritoneal adhesion formation after abdominal surgery is difficult to assess due to the lack of studies with a high-level of evidence on this subject.
Frequency of post-operative adhesions after upper abdominal surgery
According to available data, peritoneal adhesions form in 93-100% of cases after laparotomy for upper abdominal surgery in adults [10-11]. The laparoscopic approach would seem to decrease the risk to 45% [11]. The frequency of surgical re-intervention for adhesion-related symptoms varies with the type of initial procedure but, in all cases, remains below 10% in adult patients [10] between 6.4 and 10% [22-24]. The greater omentum is the organ most typically involved by adhesion formation [10].
Frequency of symptomatic post-operative adhesions after lower abdominal surgery
An analysis of the frequency of symptomatic adhesions is not possible at present except by analysis of long-term postlaparotomy complications.
Surgery by open laparotomy
After lower abdominal open surgery, 67-93% of patientsdevelop adhesions [10,25], but only 5-18% of these casesbecome symptomatic (bowel obstructions). The rate ofsymptomatic complications varies depending on the type ofinitial operation and the duration of post operative follow-up.The rate of complications directly related to adhesionsresulting in one or more hospitalizations is 3.8% [25-33].The most common site of adhesion formation is betweenthe greater omentum and the midline closure, but theseadhesions rarely result in bowel obstruction unless the bowelwall itself is involved [10]. Risk factors for the developmentof symptomatic adhesions include the number of previousinterventions, a history of peritonitis, and age less than 60years [26].
Laparoscopic surgery
No data with high-level evidence are available in this context. The frequency of symptomatic adhesions requiring re-intervention after lower abdominal laparoscopic surgery has been evaluated at 2% after colorectal surgery (whether for benign or for malignant disease) at 2.8% after rectal surgery (benign or malignant), and at 0.76% after appendectomy [34-37]. The long-term incidence of adhesion-related post-operative obstruction has been measured in two randomized prospective studies comparing laparoscopy versus laparotomy for colorectal surgery. These studies showed no statistically significant difference in the rate of postoperative obstruction: 5.1% versus 6.5% in the study by Scholin et al., and 2.5% versus 3.1% in the study by Taylor et al. The highest rate of post-operative obstruction was seen in the group of patients who required conversion from laparoscopy to laparotomy (6%) [38].
Medical and surgical consequences of peritoneal adhesions
Adhesions are responsible for direct complications (acute intestinal obstruction, chronic abdominal pain, infertility) and for indirect complications encountered at surgical re-interventions (difficult dissection, prolonged operative time, intra- and post-operative complications).
Direct consequences
There are multiple direct of adhesions with serious potential complications.
Acute intestinal obstruction
Peritoneal adhesions are the underlying cause of 32% of acute intestinal obstructions and of 65%-75% of small bowel obstructions. (SBO) This complication accounts for 2.6-3.3% of all indications for laparotomy [10,30-47]. The number of previous abdominal surgeries increased the development of peritoneal adhesions. The interval between the initial abdominal surgery and the first episode of acute small bowel obstruction varies enormously from eight days to 60 years with a mean interval of 3.7-8.9 years [10,30-47]. The need to resect intestine during re-intervention for small bowel obstruction varies from 5.7-23.2% [39]. The greatest risk of this complication seems to occur after previous colorectal surgery, which is fraught with risks of more complex adhesion formation. Recurrent complications of adhesions occur frequently after surgery for acute bowel obstruction (12-19%). The identified risk factors for acute intestinal obstruction were: age under 40 years, a complicated post-operative course, the type of adhesions (complex), multiple (>3) previous abdominal surgeries, and conservative treatment of a previous acute small bowel obstruction [41]. It seems that the first episode of acute small bowel obstruction occurs in 3/4 cases after one or two abdominal surgery [41]. However, the increase of peritoneal adhesions based on the number of surgical procedures, does not correlate in proportion to the risk of bowel obstruction. The post-operative mortality related to surgery to relieve adhesion-related acute small bowel obstruction was estimated at less than 10%. The pre- and post-operative risk factors for mortality included: ASA score greater or equal to 3, age above 75 years, the presence of dyspnea at rest, renal insufficiency, hemoconcentration/dehydration, the type of obstruction (mechanical + strangulation), intraoperative complications (intestinal spillage with peritoneal contamination), and post-operative medical complications. Surprisingly, the need for intestinal resection did not appear as a risk factor for mortality [47,48]. The post-operative morbidity for adhesion-related acute SBO is estimated at 13—47%. Risk factors for morbidity include: ASA greater or equal to 3, age above 80 years, poor general condition for independent living, past history of cardiac insufficiency, previous stroke with neurological deficit, chronic obstructive pulmonary disease (COPD), leukopenia (WBC <4500/mm3), creatinine more than 1.2 mg/dL, the type of previous surgery (intestinal resection vs. adhesiolysis), infected or contaminated operative field, more than ten adhesions, and failure to perform enterectomy after a bowel injury [47,48]. The most frequent complications were: pneumonia/atelectasis (17%), prolonged ileus more than seven days (16%), inability to wean from ventilator within 48 hours (13%), need for endotracheal re-intubation (9%), wound infection (9%), abdominal wall abscess and/or evisceration (more common after enterectomy) [47,48].
Post-operative chronic abdominal pain
Post-operative pain due to adhesions is a controversial entity; its definition remains imprecise and is often not specified in the numerous studies on this subject. Its actual incidence is therefore unknown. Laparoscopy has both a diagnostic and therapeutic role since it permits recognition and simultaneous treatment of the cause of pain, although adhesiolysis may result in renewed adhesion formation. In any case, the benefit of extensive adhesiolysis in the treatment of patients with chronic abdominal pain and diffuse adhesions has not been proved, and this procedure has its own significant morbidity (enterotomy) [49]. On the other hand, chronic abdominal pain frequently recurs, even after an initial period of improvement.
Indirect consequences of intestinal adhesions during surgical re-interventions
The presence of abdominal adhesions increases operative time, particularly when the operative site of interest has already been dissected. Adhesions lead to increased intra-operative morbidity due mainly to intestinal wounds. Intestinal injuries occur in from 0.06% to 19% of cases and are the cause of increased post-operative morbidity (fistula, intestinal obstruction, wound abscess, respiratory complications) [50,51]. The number of previous laparotomies, and obesity (BMI > 25 kg/m2) were risk factors for intestinal injury. The laparoscopic approach seems to be associated with a delay in recognition of intestinal perforation [52-57]. The laparoscopic approach to adhesiolysis also seems to directly increase the incidence of this complication, particularly due to accidents of trocar placement that are responsible for 40% of such injuries. If bowel injury is recognized intra-operatively, conversion to laparotomy is often necessary. The risks related to conversion are highly variable depending on the type of procedure performed (3.3-100%). There are few reports of hemorrhagic complications due to adhesiolysis. The need for post-operative transfusion is higher in patients who have had previous laparotomy [58]; they are considerably higher if the surgery addresses an abdominal site that had been previously dissected. For all these reasons, it is important that patients be informed of an increased risk of surgical complications associated with previous surgery and postoperative adhesions.
Prevention
In view of the magnitude of the medical problems and financial burden related to adhesions, prevention or reduction of postoperative adhesions in an important priority. Some groups have recognized the importance of the problem and have attempted to educate physicians on this issue. Numerous articles on adhesion barriers have been published but several controversies such as the effectiveness of available agents and their indication in general surgical patients still exist. Most of the available literature is based on gynecologic patients. For general surgical patients no recommendations or guidelines exist. Any prevention strategy should be safe, effective, practical, and cost effective. A combination of prevention strategies might be more effective but our knowledge on this topic is fairly limited. The prevention strategies can be grouped into 4 categories: general principles, surgical techniques, mechanical barriers, and chemical agents.
Adhesion control
Clinically, there is no means of completely preventing adhesion formation. Two commonly used solutions in clinical practice that have some anti-adhesion effect in the laboratory animal are povidone-iodine [59] and 32% dextran 70 [60]. Povidone-iodine is popular among some general surgeons as a peritoneal lavage, more for the antimicrobial effect than the anti-adhesion properties. Dextran is often used by gynaecological surgeons for adhesion prevention in infertility surgery and there is some clinical evidence that it has some effect in these cases [61]. Independent of adjuvant therapy for the prevention of adhesion formation, there are several operative steps that can be taken to reduce the extent of adhesion formation and to minimise the chances of subsequent adhesive obstruction:
1. Handle the bowel carefully to reduce serosal trauma.
2. Avoid unnecessary dissection.
3. Exclude foreign material from the peritoneum, e.g. use absorbable ligatures and sutures where possible, preferably those that are hydrolysed rather than phagocytosed. If non absorbable material is to be used then keep the cut ends as short as possible. Avoid excessive use of gauze swabs. Wear starch free gloves.
4. Adequately excise ischaemic or infected debris within the peritoneum.
5. Preserve the omentum, if possible. Place the omentum around the site of surgery and run the omentum under the wound to encourage low-risk adhesions to form.
6. Avoid the division of adhesions that do not involve the small bowel.
By what means we can prevent post-operative adhesions?
Technical means
Any surgical technique that can reduce visceral and peritoneal traumatic injury is considered a priori potentially beneficial in the prevention of adhesions.
Two methods devolving from this principle are:
· Surgery should be performed with the most atraumatic technique possible [62,63]. The measures which seem most useful to prevent the risk of adhesions include: gentle manipulation of tissue, meticulous hemostasis, the choice of small caliber sutures of inert composition, frequent irrigation of the area of dissection to prevent the formation of fibrinous deposits, minimal use of monopolar electrocautery to prevent diffuse thermal injury, maximal resection of devitalized tissues, removal of fibrinous residues and blood clot prior to peritoneal closure;
· Laparoscopy: the theoretic advantages of this approach include: minimal incision of the parietal peritoneum, a maximal reduction of microscopic foreign bodies, preservation of the moist closed intraperitoneal environment, decreased bleeding and more precise dissection (particularly for pelvic and rectal surgery), and the absence or minimization of manipulation beyond the operative zone; these advantages have been highlighted in several retrospective studies comparing laparotomy and laparoscopy [63-65], but the level of evidence is low in these studies. The theoretical advantages have not been shown to translate into a decreased risk of bowel obstruction in two randomized prospective studies comparing the long-term risk of bowel obstruction after colorectal surgery by the laparotomy or laparoscopic approach [38,66]. These contradictory results suggest that a decrease in abdominal adhesions does not necessarily result in a decrease in the rate of post-operative obstruction.
Commercial products and devices to prevent adhesion formation
The mechanisms of action of anti-adhesion products are based on two principles: hydroflotation and the barrier phenomenon.
Hydroflotation
It is the mechanism of action of products instilled into the peritoneal cavity. These are fluids such as a 4% solution of Icodextrin. Their principal theoretical advantage is that the product is applied to the entire peritoneal surface and is easy to use in the laparoscopic setting. Disadvantages include: the kinetics of peritoneal reabsorption are variable from patient to patient, but reabsorption is often complete within one to two days while the histopathologic process of adhesion formation continues throughout the first postoperative week, and the fluid tends to accumulate in the pelvis and pouch of Douglas as the patient changes position [62]. At this time, these products do not have marketing approval in France for gastrointestinal surgery indications.
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org
Subscribe to PharmaTutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
The barrier phenomenon
It is the preponderant mechanism of action of a variety of products marketed as biocompatible and biodegradable films, such as membrane films of hyaluronic acid on a supporting structure of carboxymethylcellulose (Seprafilm®, Genzyme Corp., USA), oxidized cellulose (Interceed®, Johnson& Johnson, New Brunswick, NJ, USA), and in the form of inert non-resorbable prostheses such as expanded polytetrafluoroethylene patches (PTFE) (Gore-Tex® and Preclude®, Gore & associates, Newark, Delaware, USA). Their principal advantage is to set up a fixed physical barrier between the viscera from the parietal peritoneum, whose reabsorption kinetics can be much better controlled and predictable than is the case for solutions and gels. Their principal disadvantage is that their action is limited only to the site where they are placed. A single leaf of these products covers only a small percentage of the total peritoneal surface; the surgeon must be mindful that it only requires a single adhesion (that may develop at some distance from the operative site) to provoke a severe complication such as bowel obstruction [62]. The surgeon must therefore select the zone for film application where he anticipates the greatest likelihood of adhesion formation; surgeons usually opt for the incision line and the site of surgical dissection. A second disadvantage is that films are technically difficult to apply through laparoscopic access ports. This is particularly the case for Seprafilm® [67]; it is extremely difficult to achieve accurate placement of Seprafilm® at laparoscopy, and yet the effect of the treatment depends essentially on impeccably accurate placement. For placement of nonresorbable patches (expanded PTFE) that require suture fixation, laparoscopic placement is even more difficult. Products in gel form depend of both hydroflotation and the barrier phenomenon for their effect; these include 0.5% ferric hyaluronate gel (Intergel®, Lifecore Biomedical Inc, Chaska, MN, USA) and a hydrogel of polyethylene glycol delivered as a spray (Spraygel®, Confluent Surgical Inc, Waltham, MA, USA), or a derivative with more rapid resorption and neutral coloration (Sprayshield® Covidien,Waltham, MA, USA). The advantages of gel anti-adhesion products are a longer half-life (one to two weeks) than instilled peritoneal liquids, and ease of application compared to film placement, particularly when applied to irregular surfaces such as the limbs of enteric anastomoses.
Bioabsorbable gels
Various agents have been developed and tested, but most have been abandoned or withdrawn because of safety issues or a lack of efficacy. SprayGel (Confluent Surgical, Inc, Waltham, MA) is one of the more extensively tested gels. It is a sprayable hydrogel that adheres to the tissues for a period of 5 to 7 days. After several days it is hydrolyzed into water-soluble molecules and is absorbed. The safety of SprayGel has been shown in a few gynecologic and colorectal studies [68-71].Although early preliminary clinical trials showed its effectiveness, a larger-scale study was stopped owing to a lack of efficacy.
Future advances
In the absence of any clinically proven means of preventing adhesions from forming, the onus lies with the surgeon to try and minimalise their occurrence by improved and assiduous surgical techniques. The advent of laparoscopic surgery may alter the incidence of adhesions and adhesive obstruction after abdominal surgery. The reduced bowel trauma from handling, the absence of large abdominal wounds and the exclusion of foreign material such as lint, gauze and starch from the abdominal cavity must reduce adhesion formation after laparoscopic surgery. One study has already demonstrated that when a stimulus is applied at open laparotomy in an animal it produces more adhesions than when the same stimulus is applied through the laparoscope [72]. No additional adhesions were found at remote areas when the laparoscope had been used. Despite the promise of laparoscopic surgery, adhesions will continue to be a major source of concern for surgeons, not only because of the technical difficulties they present but also because of the volume of work they generate. It is possible that in the future these problems may be reduced by some form of rt-PA peritoneal lavage after surgery or adhesion division that will deter adhesion formation or re-formation and this will go some way in lightening the burden of a pathological process produced by surgery itself.
Conclusion
Postoperative adhesions are a significant health problem with major implications on quality of life and health care expenses. General intraoperative preventative techniques, such as starch-free gloves, avoiding unnecessary peritoneal dissection, avoiding spillage of intestinal contents or gallstones, and reducing remaining surgical material, may reduce the risk of adhesions and should be applied in every patient. Laparoscopic techniques are preferable to open techniques whenever possible. In high-risk procedures the use of bioabsorbable mechanical barriers should be considered.
References
1. Dcizerega GS. Biochemical events in peritoneal tissue repair. Eur J Surg 1997; 577:10-16.
2. Dizerega GS. The peritoneum: post-surgical repair and adhesions formation. In Rock JA, Murphy AA, Jones HW, eds. Female reproductive surgery. Boston: Williams and Wilkins 1992, 2-18.
3. Coleman MG, McLain AD, Moran BJ. Impact of previous surgery on time taken for incision and division of adhesions during laparotomy. Dis Colon Rectum 2000; 43:1297-99.
4. Rangabashyam N. Peritoneal surgery. Susrutha Surgical Continuing Medical Education Programme, Chennai, 2001.
5. Rangabashyam N. Reopertive Surgery for bowel obstruction following abdominal operation, Methods of intestinal decompression and difficulties in abdominal closure. ASICON, New Delhi, December 2000.
6. Suman.V.Gupta. Post-operative adhesions - Morbidity and Management. Journal of Gastroenterology 1997; 72:28-37.
7. Holmdahl L. The role of Fibrinolysis in Adhesion formation. Eur J Surg 1997; 57;24-31.
8. Ray NF, Denton WG, Thamer M, Henderson SC, Perry S. Abdominal Adhesiolysis: Inpatient care and expenditure in the United States in 1994. J Am Coll Surg 1998; 186(l):l-9.
9. Manzies D, Ellis H. Intestinal obstruction from adhesions: How big is the problem? Ann R Coll Surg, 6, 1993, 9-23.
10. Menzies D, Ellis H. Intestinal obstruction from adhesions: how big is the problem? Ann R Coll Surg Engl 1990; 72:60-3.
11. Nunobe S, Hiki N, Fukunaga T, et al. Previous laparotomy is not a contraindication to laparoscopy-assisted gastrectomy for early gastric cancer. World J Surg 2008; 32:1466-72.
12. De Wilde RL, Trew G, ESGE Expert adhesions working party. Postoperative abdominal adhesions and their prevention in gynaecological surgery. Expert consensus position. Gynecol Surg 2007; 4:161-8.
13. Wiebel MA, Majno G. Peritoneal adhesions and their relation to abdominal surgery. Am J Surg 1973; 126:345-53.
14. Panay N and Lower A.M (1999). New directions in the prevention of adhesions in laparoscopic surgery. Curr Opin Obstet Gynecol 11:379-385.
15. Monk B.J, Berman M.L and Montez F.J (1994). Adhesions after extensive gynaecologic surgery: clinical significance, etiology and prevention. Am J Obstet Gynecol 170:1396-1403.
16. Ray N.F, Larsen J.W, Stillman R.J and Jacobs R.J (1993). Economical effect of hospitalization for lower abdominal adhesiolysis in United States in 1988. Surg Gynecol Obstet 176:271-276.
17. Raftery AT. Regeneration of parietal and visceral peritoneum: an electron microscopical study. J Anat 1973; 115(Pt 3):375-92.
18. Van der Wal JBC, Jeekel J. Biology of the peritoneum in normal homeostasis and after surgical trauma. Colorectal Dis 2007; 9(Suppl. 2):9-13.
19. Bellina JH, Hemmings R, Voros JI, Ross LF. Carbon dioxide laser and electrosurgical wound study with an animal model: a comparison of tissue damage and healing patterns in peritoneal tissue. Am J Obstet Gynecol 1984; 148(3):327-34.
20. Forestier D, Slim K, Joubert-Zakeyh J, Nini E, Dechelotte P, Chipponi J. Do bipolar scissors increase postoperative adhesions? An experimental double-blind randomized trial. Ann Chir 2002; 127(9):680-4.
21. Duron JJ. Postoperative intraperitoneal adhesion pathophysiology. Colorectal Dis 2007; 9(Suppl. 2):14-24.
22. Wilkins BM, Ellis H. Incidence of postoperative adhesion obstruction following neonatal laparotomy. Br J Surg 1986; 73:762-4.
23. Karayiannakis AJ, Polychronidis A, Perente S, et al. Laparoscopic cholecystectomy in patients with previous upper or lower abdominal surgery. Surg Endosc 2004; 18(1):97-101.
24. Hayashi S, Takayama T, Masuda H, et al. Bioresorbable membrane to reduce postoperative small bowel obstruction in patients with gastric cancer. Ann Surg 2008; 247:766-70.
25. Leung TT, Dixon E, Gill M, et al. Bowel obstruction following appendectomy: what is the true incidence? Ann Surg 2009; 250:51-3.
26. Parker MC, Wilson MS, Menzies D, et al. The SCAR-3 study: 5- year adhesion related readmission risk following lower abdominal surgical procedures. Colorectal Dis 2005; 7(6):551-8.
27. Ellis H, Moran BJ, Thompson JN, et al. Adhesion-related hospital readmissions after abdominal and pelvic surgery: a retrospective cohort study. Lancet 1999; 353(9163):1476-80.
28. Lower AM, Hawthorn RJ, Ellis H, et al. The impact of adhesions on hospital readmissions over ten years after 8849 open gynaecological operations: an assessment from the surgical and clinical adhesions research study. BJOG 2000; 107(7):855-62.
29. Parker MC, Ellis H, Moran BJ, et al. Postoperative adhesions: ten-year follow-up of 12,584 patients undergoing lower abdominal surgery. Dis Colon Rectum 2001; 44(6):822-9.
30. MacLean AR, Cohen Z, MacRae HM, et al. Risk of small bowel obstruction after the ileal pouch-anal anastomosis. Ann Surg 2002; 235(2):200-6.
31. Fazio VW, Ziv Y, Church JM, et al. Ileal pouch-anal anastomoses complications and function in 1005 patients. Ann Surg 1995; 222(2):120-7.
32. Nieuwenhuijzen M, Reijnen MM, Kuijpers JH, et al. Small bowel obstruction after total or subtotal colectomy: a 10-year retrospective review. Br J Surg 1998; 85(9):1242-5.
33. Andersson RE. Small bowel obstruction after appendicectomy. Br J Surg 2001; 88(10):1387 91.
34. Wong DC, Chung CC, Chan ES, Kwok AS, Tsang WW, Li MK. Laparoscopic abdominoperineal resection revisited: are there any health-related benefits? A comparative study. Tech Coloproctol 2006; 10:37-42.
35. Zhou ZG, Hu M, Li Y, et al. Laparoscopic versus open total mesorectal excision with anal sphincter preservation for low rectal cancer. Surg Endosc 2004; 18:1211-5.
36. Staudacher C, Vignali A, Saverio DP, Elena O, Andrea T. Laparoscopic vs. open total mesorectal excision in unselected patients with rectal cancer: impact on early outcome. Dis Colon Rectum 2007; 50:1324-31.
37. Duron JJ, Hay JM, Msika S, et al. Prevalence and mechanisms of small intestinal obstruction following laparoscopic abdominal surgery: a retrospective multicenter study. French Association for Surgical Research. Arch Surg 2000; 135:208-12.
38. Taylor GW, Jayne DG, Brown SR, et al. Adhesions and incisional hernias following laparoscopic versus open surgery for colorectal cancer in the CLASICC trial. Br J Surg 2010; 97(1):70-8.
39. Miller G, Boman J, Shrier I, Gordon PH. Natural history of patients with adhesive small bowel obstruction. Br J Surg 2000; 87(9):1240-7.
40. Tingstedt B, Isaksson J, Andersson R. Long-term follow up and cost analysis following surgery for small bowel obstruction caused by intra-abdominal adhesions. Br J Surg 2007; 94(6):743-8.
41. Duron JJ, Jourdan Da Silva N, du Montcel ST, et al. Adhesive postoperative small bowel obstruction: incidence and risk factors of recurrence after surgical treatment: a multicenter prospective study. Ann Surg 2006; 244(5):750-7.
42. Wilson MS, Hawkswell J, McCloy RF. Natural history of adhesional small bowel obstruction: counting the cost. Br J Surg 1998; 85(9):1294-8.
43. Levard H, Boudet MJ, Msika S, et al. Laparoscopic treatment of acute small bowel obstruction: a multicentre retrospective study. ANZ J Surg 2001; 71(11):641-6.
44. Choi HK, Chu KW, Law WL. Therapeutic value of gastrografin in adhesive small bowel obstruction after unsuccessful conservative treatment: a prospective randomized trial. Ann Surg 2002; 236(1):1-6.
45. Di Saverio S, Catena F, Ansaloni L, Gavioli M, Valentino M, Pinna AD. Water soluble contrast medium gastrografin) value in adhesive small intestine obstruction (ASIO): a prospective, randomized, controlled, clinical trial. World J Surg 2008; 32(10):2293-304.
46. Fevang BT, Fevang J, Lie SA, et al. Long-term prognosis after operation for adhesive small bowel obstruction. Ann Surg 2004; 240(2):193-201.
47. Margenthaler JA, Longo WE, Virgo KS, et al. Risk factors for adverse outcomes following surgery for small bowel obstruction. Ann Surg 2006; 243(4):456-64.
48. Duron JJ, du Montcel ST, Berger A, et al. Prevalence and risk factors of mortality and morbidity after operation for adhesive postoperative small bowel obstruction. Am J Surg 2008; 195(6):726-34.
49. Van Goor H. Consequences and complications of peritoneal adhesions. Colorectal Dis 2007; 9(Suppl. 2):25-34.
50. Makoha FW, Fathuddien MA, Felimban HM. Choice of abdominal incision and. risk of trauma to the urinary bladder and bowel in multiple cesarean sections. Eur J Obstet Gynecol Reprod Biol 2006; 125(1):50-3.
51. Van Der Krabben AA, Dijkstra FR, Nieuwenhuijzen M, et al. Morbidity and mortality of inadvertent enterotomy during adhesiotomy. Br J Surg 2000; 87(4):467-71.
52. El-Hakim A, Chiu KY, Sherry B, et al. Peritoneal and systemic inflammatory mediators of laparoscopic bowel injury in a rabbit model. J Urol 2004; 172(4 Pt1):1515-9.
53. LeBlanc KA, Booth WV, Whitaker JM, Bellanger DE. Laparoscopic incisional and ventral herniorrhaphy in 100 patients. Am J Surg 2000; 180(3):193-7.
54. Ben-Haim M, Kuriansky J, Tal R, et al. Pitfalls and complications with laparoscopic intraperitoneal expanded polytetrafluoroethylene patch repair of postoperative ventral hernia. Surg Endosc 2002; 16(5):785-8.
55. Carbajo MA, Martp del Olmo JC, Blanco JI, et al. Laparoscopic approach to incisional hernia. Surg Endosc 2003; 17(1):118-22.
56. Rosen M, Brody F, Ponsky J, et al. Recurrence after laparoscopic ventral hernia repair. Surg Endosc 2003; 17(1):123-8.
57. Bencini L, Sánchez LJ. Learning curve for laparoscopic ventral hernia repair. Am J Surg 2004; 187(3):378-82.
58. Van der Voort M, Heijnsdijk EA, Gouma DJ. Bowel injury as a complication of laparoscopy. Br J Surg 2004; 91(10):1253-8.
59. Gilmore OJA, Reid C. Prevention of peritoneal adhesions by a new povidone-iodine/PVP solution. Jf Surg Res 1978; 25:477-81.
60. Holtz G, Baker ER. Inhibition of peritoneal adhesion formation after lysis with 32% dextran 70. Feruil Steril 1980; 34: 394-5.
61. Adhesion Study Group. Reduction of post-operative pelvic adhesions with intraperitoneal 32% dextran 70:a prospective randomised clinical trial. Fertil Steril 1983; 40:612-19.
62. Johns A. Evidence-based prevention of post-operative adhesions. Human Reproduction Update 2001; 7(6):577-9.
63. Duron JJ. Brides et adherences intraperitoneales postoperatoires: realites actuelles et futures. Ann Chir 2004; 129(9):487-8.
64. Dowson HM, Bong JJ, Lovell DP, Worthington TR, Karanjia ND, Rockall TA. Reduced adhesion formation following laparoscopic versus open colorectal surgery. Br J Surg 2008; 95(7):909-14.
65. Audebert AJ, Gomel V. Role of microlaparoscopy in the diagnosis of peritoneal and visceral adhesions and in the prevention of bowel injury associated with blind trocar insertion. Fertil Steril 2000; 73:631-5.
66. Scholin J, Buunen M, Hop W, et al. Bowel obstruction after laparoscopic and open colon resection for cancer: Results of 5 years of follow-up in a randomized trial. Surg Endosc 2011; 25(12):3755-60.
67. Khaitan L, Scholz S, Richards WO. Laparoscopic adhesiolysis and placement of Seprafilm (trademark): A new technique and novel approach to patients with intractable abdominal pain. J Laparoendosc Adv Surg Tech A 2002; 12(4):241-7.
68. Dunn R, Lyman MD, Edelman PG, et al. Evaluation of the SprayGel adhesion barrier in the rat cecum abrasion and rabbit uterine horn adhesion models. Fertil Steril 2001;75:411– 6.
69. Mettler L, Audebert A, Lehmann-Willenbrock E, et al. A randomized, prospective, controlled, multicenter clinical trial of a sprayable, site-specific adhesion barrier system in patients undergoing myomectomy. Fertil Steril 2004;82:398–404.
70. Johns DA, Ferland R, Dunn R. Initial feasibility study of a sprayable hydrogel adhesion barrier system in patients undergoing laparoscopic ovarian surgery. J Am Assoc Gynecol Laparosc 2003;10:334–8.
71. Tjandra JJ, Chan MK. A sprayable hydrogel adhesion barrier facilitates closure of defunctioning loop ileostomy: a randomized trial. Dis Colon Rectum 2008;51:956–60.
72. Luciano AA. Laparotomy versus laparoscopy. Prog Clin Biol Res 1990;358:35-44.
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org
Subscribe to PharmaTutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE









