{ DOWNLOAD AS PDF }
ABOUT AUTHORS
ASHIKA RANJANI. M*, SAHITHI GOUD. B, AMATUL WADOOD SUMAYYA, SYEDA NABILA FIRDOUS, AMATUL ALI SAMEERA
Dept. of Pharmacy Practice
Sree Dattha Institute of Pharmacy, Jawaharlal Nehru Technological University (Hyderabad)
Sheriguda (V), Ibrahimpatnam (M), Ranga Reddy (Dist), Telangana, India
ABSTRACT
AIMS AND OBJECTIVES: Our aim was to evaluate the clinical use of Antihypertensive drugs in patients with chronic Kidney disease at a tertiary care teaching hospital.
METHOD: An observational, prospective cohort study was conducted at a tertiary care teaching hospital in Hyderabad, T.S, India. A total of 184 patients from the inpatient department of nephrology Department at Gleneagles Global Hospitals, Bairamalguda, LB Nagar, Hyderabad. All information significant to the study was collected from the case records and discussions conducted with the in-patients and bystanders during ward rounds, with the support of a physician, which were analyzed by SPSS software. Moreover, daily follow-ups were conducted to assemble data on amendment in therapy, add-on therapy, and clinical improvement.
RESULTS: The Mean Age was 59.29 years and the standard deviation was 1.116 of the population, 60% were smokers and 40% were alcoholics. The most commonly used Class of anti-hypertensive drugs are Calcium channel blockers with percentage of 64.13%, Diuretics with percentage of 57.60%, β blockers with percentage of 43.47%. Whereas most commonly used Calcium channel blockers are Amlodipine with percentage of 52%, and Cilindipine with percentage of 9.10%.Diuretics are are Furosemide with percentage of 36.90% and Toresemide 11.40%. Most commonly used Adenergic Antagonist are in β Blockers are Metoprolol with percentage of 31.50%, In α blockers are prazosin with percentage of 26%, In α+β blocker are Carvedilol with percentage of 8.60%. Most commonly used ARB’s are Telmisartan with percentage of 6.50%, and ACE’s are Ramipril with percentage of 1%. Most commonly used central sympatholytics are Clonidine with percentage of 18.40%, Vasodilators are Minoxidil with percentage of 1%. Medication adherence have been done, In which patients with High Adherence are with percentage of 16.21%, Medium Adherence are with percentage of 45.94%, Low Adherence are with percentage of 37%. This is done by Morisky medication adherence scale 8.
CONCLUSION: We have concluded that the CCB’s, diuretics and β-blockers are the most commonly used anti-hypertensive classes in hypertensive patients with CKD. Use of anti-hypertensives in CKD patients does not deviate from the guidelines laid down by NKF KDOQI guidelines. The patients should be educated about the rational use of drugs to decrease medication adherence.
[adsense:336x280:8701650588]
Reference Id: PHARMATUTOR-ART-2652
|
PharmaTutor (Print-ISSN: 2394 - 6679; e-ISSN: 2347 - 7881) Volume 7, Issue 03 Received On: 03/01/2019; Accepted On: 18/02/2019; Published On: 01/03/2019 How to cite this article: Ranjani, A.M., Goud, S., Sumayya, A., Firdous, S. and Sameera, A. 2019. Drug Utilization of Anti Hypertensives in CKD Patients: A Randomized Prospective Study at a Tertiary Care Teaching Hospital. PharmaTutor. 7, 3 (Mar. 2019), 41-72. DOI:https://doi.org/10.29161/PT.v7.i3.2019.41 |
INTRODUCTION
Chronic kidney disease most often results from a progressive loss of functioning nephrons caused by a primary kidney disease or as a secondary complication of certain systemic diseases, but it can also result from an acute event causing irreversible damage to the kidneys. (Mary Anne Koda-Kimble et al., 2008)
Both Hypertension (HTN) and CKD are serious interrelated global public health problems. Nearly 30% and 15% of US adults have HTN and CKD, respectively. Because HTN may cause or result from CKD, HTN prevalence is higher and control more difficult with worse kidney function. (Horowitz B et al., 2015)
There is a high prevalence of HTN in renal patients, which depends on the type of nephropathy and the degree of renal failure. Other independent risk factors for HTN in patients with renal disease are: advanced age, the presence of diabetes, hyper triglyceridaemia and the severity of proteinuria. BP control in renal patients is quite poor and should be improved to reduce progression of the renal disease. (Ridao N etal., 2001)
The Third National Health and Nutrition Examination Survey (NHANES III), a national study of more than 18,000 persons 20 years of age or older conducted from 1988 through 1994, provides information on the stages of CKD in the U.S. population. From these data, it is estimated that 8. 3million Americans have CKD stages 3 to 5. They also reported that 11.3 million Americans are at risk for developing or have mild decrease in kidney function (CKD stage 1 and 2).Data describing the ESRD population are made available annually by the U.S. Renal Data System (USRDS). The reports characterize the development, treatment, morbidity, and mortality associated with ESRD in the United States and include data from patients with kidney transplants. Based on the most recent data from the USRDS, more than 472,000 patients were receiving renal replacement therapy for ESRD at the end of 2004, with approximately 104,000 new patients starting treatment during that year. A continued increase in incidence rates of ESRD has been observed over the past decade, although this rate has decreased to approximately 1.5% to 5% per year over the past 5 years. The continued increase in incidence rates of ESRD, in conjunction with a relatively stable death rate for this population, accounts for the overall increase in the prevalence of ESRD. CKD has been identified as one of the focus areas for the Healthy People 2010 national health initiative; one of the specific objectives is to reduce the number of new cases of ESRD.4 Populations at increased risk for developing ESRD include males and the older population, particularly patients 65 years of age and older. More than 49% of incident hemodialysis patients in 2004 were age 65 or older, a much larger percentage than for the peritoneal dialysis and transplant populations.3 Racial distribution of the dialysis population shows that the prevalence is greatest in whites (61%) and blacks (32%), followed by Hispanics (14%) and Asians (4%). Blacks and Native Americans have a three to four times greater incident rate of kidney failure than white individuals.
A variety of causes are responsible for the remaining cases of ESRD, among which are cystic kidney disease, other urologic causes, and acquired immunodeficiency syndrome (AIDS) nephropathy. Mortality Advances in dialysis and transplantation have improved patient care; however, mortality rates during the first year of ESRD have not improved over the past decade (first-year adjusted death rate is 234/1,000 patient-years in the year 2003 for prevalent ESRD patients).Patients with cardiovascular disease on dialysis have a fivefold greater risk of all-cause mortality when compared with the general Medicare population and with patients with CKD not yet requiring renal replacement therapy. (Mary Anne Koda-Kimble et al., 2008) Comorbid conditions, low albumin, malnutrition, and anemia at initiation of dialysis are strong predictors of mortality. Life expectancy is 20% to 25% of that of the general population. Cardiovascular-related events, particularly cardiac arrest and myocardial infarction, are the leading causes of death in the ESRD population. This is not surprising given the high prevalence of coexisting cardiac disorders in patients with ESRD and the elevated risk for mortality associated with these conditions. The Healthy People 2010 initiative for CKD will also focus on decreasing deaths from cardiovascular disease.4 Infection (predominantly septicemia) and cerebrovascular disease are also substantial contributors to overall mortality in patients with ESRD. (Mary Anne Koda-Kimble et al., 2008)
It has been estimated that at least 6% of the adult U.S. population have chronic renal damage with a GFR 60 mL/min per 1.73 m2 (stages 1 and 2 CRD) and hence are at imminent risk of a progressive further decline in GFR. An additional 4.5% of the U.S. population are in stages 3 and 4 CRD. Diabetic and hypertensive nephropathy are the leading underlying etiologies of both CRD and ESRD. Hypertension is a particularly common cause and consequence of CRD in the elderly, in whom chronic renal ischemia due to renovascular disease may be an under recognized additional contribution to the pathophysiologic process. It should be noted that cardiovascular mortality precludes most patients with CRD from reaching the stage of ESRD. Identification of CRD as a major risk factor for cardiovascular morbidity and mortality, and the expectation of effective interventions to diminish premature cardiovascular mortality, and increasing longevity overall, will increase the cohort of patients reaching ESRD. Although the clinical manifestations of the declining GFR per se dominate the clinical presentation in all forms of CRD, in many cases the underlying etiology can be presumed from associated additional clinical information. (Kasper et al., 2008)
Hypertension is present in more than 80% of patients with CKD and contributes to progression of kidney disease toward end stage (ESRD) as well as to cardiovascular events such as heart attack and stroke. In fact the risk for cardiovascular death in this patient population is greater than the risk for progression to ESRD. Proteinuria is an important co-morbidity in hypertensives with CKD and increase risk of disease progression and cardiovascular events. Treatment of hypertension is therefore imperative. The National Kidney Foundation clinical practice guidelines recommend a blood pressure goal of <130 mmHg systolic and <80 mmHg diastolic for all CKD patients. Recent post-hoc analyses of the Modification of Diet in Renal Disease study indicate that lower blood pressure may provide long-term kidney protection in patients with non-diabetic kidney disease. Specifically a mean arterial pressure <92 mmHg (e.g. 120/80 mmHg) as compared to 102-107 mmHg (e.g. 140/90 mmHg) is associated with reduced risk for ESRD. In most cases achieving this goal requires both non-pharmacologic and pharmacologic intervention. Dietary sodium restriction to no more than 2 grams daily is important. In addition, moderate alcohol intake, regular exercise, weight loss in those with a body mass index greater than 25 kg/M(2) and reduced amount of saturated fat help to reduce blood pressure.
The first line pharmacologic intervention should be an angiotensin converting enzyme inhibitor or angiotensin II type 1 receptor blocker in those with diabetes or non-diabetics with more than 200 mg protein/gram creatinine on a random urine sample. For non-diabetics with less than 200 mg protein/gram creatinine on a random urine sample, no specific first-line drug class is recommended. After initial dosing with an ACEi, ARB or other drug, a diuretic should be added to the regimen. Thereafter, beta-blockers, calcium channel blockers, apha blockers and alpha 2 agonists (e.g. clonidine) and finally vasodilators (e.g. minoxidil) should be added to achieve blood pressure goal. Combinations of ACEi and ARB are helpful in reducing proteinuria and may also lower blood pressure further in some some cases. Blood pressure should be monitored closely in hypertensive patients with CKD and both clinic and home blood pressure measurements may help the clinician adjust treatment. (Toto RD, 2005)
Adjustments in dietary intake and use of loop diuretics, occasionally in combination with metalozone, may be needed to maintain salt and hence extracellular fluid volume balance. In contrast, overzealous salt restriction and diuretic use may cause hypovolemia and precipitate a further decline in GFR. Occasional patients with salt-wasting states need to be given sodium-rich diets or sodium supplements. Water restriction is indicated only if there is a demonstrated propensity to hyponatremia. Intractable ECFV expansion, despite dietary restriction and diuretic use, indicates the need to initiate renal replacement therapy. Hyperkalemia often responds to dietary restriction of potassium, avoidance of potassium-containing or -retaining medications, and to) the use of diuretics if they are also indicated for management of sodium balance. Many salt substitutes contain potassium instead of sodium, and patients with CRD seeking to avoid sodium should be cautioned accordingly as part of their dietary counseling. Potassium-binding resins taken with cathartics can promote gastrointestinal potassium losses and thus are useful as temporizing measures in the treatment or avoidance of hyperkalemia in CRD patients. However, the need for such treatment over a prolonged period, in the absence of other reversible causes of hyperkalemia, usually signifies the need to initiate renal replacement therapy. (Kasper, 2008)
In a small proportion of people with kidney disease, the condition will eventually get to a point where their kidneys stop working. This rarely happens suddenly, so there should be time to plan the next stage of your treatment. One of the options when CKD reaches this stage is to have dialysis. This is a procedure to remove waste products and excess fluid from the blood.
There are two main types of dialysis:
Haemodialysis: This involves diverting blood into an external machine, where it's filtered before being returned to the body.
Peritoneal dialysis: This involves pumping dialysis fluid into the space inside your tummy to draw out waste products from the blood passing through vessels lining the inside of your tummy.
Haemodialysis is usually done about three times a week, either at hospital or at home. Peritoneal dialysis is normally done at home several times a day, or overnight. If there is no use of kidney transplant, treatment with dialysis usually need to be done lifelong. (British Kidney Patient Association 2006)
LITERATURE REVIEW
DEFINITION
Chronic kidney disease is characterized by a progressive deterioration in kidney function ultimately leading to irreversible structural damage to existing nephrons (Mary Anne Koda-Kimble et al., 2008). Kidney damage is indicated by pathologic abnormalities or markers of injury, including abnormalities in blood or urine tests and imaging studies. The presence of protein in the urine (defined as proteinuria, albuminuria, or micro albuminuria based on protein type and amount) is an early and sensitive marker of kidney damage.
STAGES
Based on the progressive nature of this condition, a staging system has been established to classify kidney disease according to the eGFR, which is estimated clinically using creatinine clearance (ClCr). Specifically, CKD is defined as kidney damage with a normal or a mildly decreased eGFR (stages 1 and 2) or a eGFR (Mary Anne Koda-Kimble et al., 2008).
TABLE-1: Stages according to National Kidney Foundation. NKF-K/DOQI Clinical Practice Guidelines for Chronic Kidney Disease: Evaluation, Classification, and Stratification (Mary Anne Koda-Kimble et al., 2008).
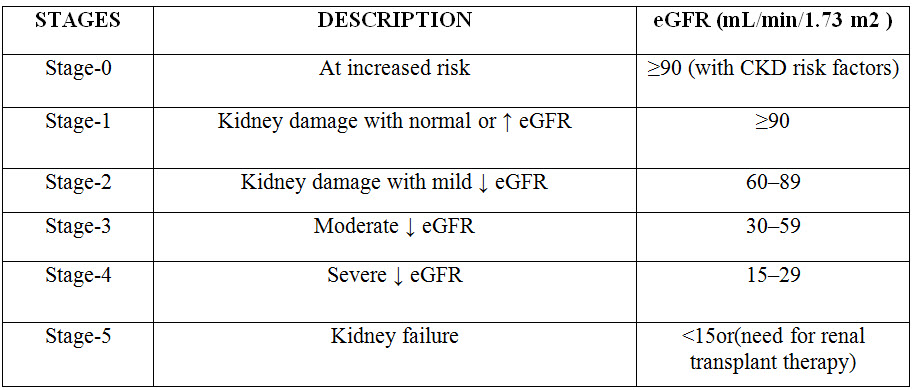
CKD is classified by cause of kidney disease, glomerular filtration rate (GFR) category, and albuminuria level based on new recommendations from the Kidney Disease: Improving Global Outcomes (KDIGO) guidelines, referred to as CGA staging (cause, GFR, albuminuria) (Barbara G. Wells et al., 2015).
EPIDEMOLOGY
Both hypertension (HTN) and CKD are serious interrelated global public health problems. Nearly 30% and 15% of US adults have HTN and CKD, respectively. Because HTN may cause or result from CKD, HTN prevalence is higher and control more difficult with worse kidney function. Etiology of CKD, presence and degree of albuminuria, and genetic factors all influence HTN severity and prevalence. In addition, socioeconomic and lifestyle factors influence HTN prevalence and control. There are racial and ethnic disparities in the prevalence, treatment, risks, and outcomes of HTN in patients with CKD. Control of blood pressure (BP) in Hispanic and African Americans with CKD is worse than it is whites. There are disparities in the patterns of treatment and rates of progression of CKD in patients with HTN. The presence and severity of CKD increase treatment resistance. HTN is also extremely prevalent in patients receiving hemodialysis, and optimal targets for BP control are being elucidated. Although the awareness, treatment, and control of HTN in CKD patients is improving, control of BP in patients at all stages of CKD remains suboptimal (Horowitz B et al., 2015).
RISK FACTORS
Age: Renal function decreases with age in both men and women (Iseki K, 2005) Thus, the elderly population is more prone to develop CKD after various renal insults (Falodia J. Singla MK 2012). At any age and various conditions can lead to CKD. After the age of 40, kidney filtration begins to fall by approximately 1% per year. In addition to the natural aging of the kidneys, many conditions that damage the kidneys are more common in older people including diabetes, high blood pressure, and heart disease (Centers for Disease Control and Prevention 2018).
Gender: These include gender differences in kidney anatomy, kidney hemodynamic stress response, effect of sex hormones, diet, lipid metabolism, and blood pressure (Neugarten J. Golestaneh L 2013; Silbiger S. Neugarten J 2013).
Anatomically, the kidney is usually larger in men, due to a larger body surface area. The hemodynamic stress response of the kidney differs between men and women; men may develop higher filtration fraction in response to angiotensin II infusion (Miller JA. 1999).
Low birth weight: The intrauterine growth restriction might cause a low nephron number, which could predispose to hypertension and renal disease (Mackenzie HS. 1999). Low nephron number leads to intraglomerular hypertension and hyper filtration in the available nephrons and lower over-all GFR and higher urine albumin-to-creatinine ratio (Vikse BE et al., 2008).
Smoking: Smoking can increase the CKD risk through proinflammatory state, oxidative stress, prothrombotic shift, endothelial dysfunction, glomerulosclerosis and tubular atrophy (Mirrakhimov AE. 2012)
Nephrotoxins: Medications can cause or worsen kidney dysfunction and these effects are exacerbated in patients with underlying CKD. Many commonly used drugs, including over-the-counter medications, can cause nephrotoxicity (The UMHS Clinical Guideline on Chronic Kidney Disease. 2013)
Alcohol and recreational drugs have been linked to CKD progression as well as excessive use of analgesic drugs and exposure to heavy metals (Falodia J. Singla MK, 2012).
Diabetes Mellitus: Diabetes mellitus (DM) is the leading cause of CKD and ESRD .Mechanisms that lead to kidney disease in diabetes include hyper filtration injury, advanced glycosylation end products, and reactive oxygen species.
Hypertension: High blood pressure can damage blood vessels throughout your body. This can reduce the blood supply to important organs like the kidneys. High blood pressure also damages the tiny filtering units in your kidneys. As a result, the kidneys may stop removing wastes and extra fluid from your blood. The extra fluid in your blood vessels may build up and raise blood pressure even more (McClellan WM. Flanders WD, 2003).
Obesity: Obesity may contribute to the pathogenesis of kidney damage through inflammation, oxidative stress, endothelial dysfunction, prothrombotic state, hypervolemia, and adipokine derangements.
Glomerular hypertrophy and hyper filtration may accelerate kidney injury by increasing capillary wall tension of the glomeruli and decreasing podocyte density (Lea JP. Nicholas SB, 2002). Obesity may contribute to the pathogenesis of kidney damage through inflammation, oxidative stress, endothelial dysfunction, prothrombotic state, hypervolemia, and adipokine derangements (National Kidney Foundation-Hypertension). Besides high BMI, carrying excess weight around the abdomen is linked to an increased risk of CKD (Chang A. Kramer H, 2012).
Family history: Family members of CKD patients have a high prevalence of CKD and its risk factors due to hereditary disorders and urologic causes (Kwakernaak AJ et al., 2013).
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT editor-in-chief@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
PATHOPHYSIOLOSY
The initial structural damage may depend on the primary disease affecting the kidney. However, the majority of progressive nephropathies share a final common pathway to irreversible renal parenchymal damage and ESRD. The key elements of this pathway are
1. loss of nephron mass,
2. glomerular capillary hypertension, and
3. proteinuria
Loss of nephron mass: Progression of kidney disease to ESRD generally occurs over months to years and is assessed by the rate of decline in eGFR. There are approximately 1 million nephrons per kidney, each maintaining its own single nephron eGFR. Progressive loss of nephron function results in adaptive changes in remaining nephrons to increase single nephron eGFR.
Over time, the compensatory increase in single nephron eGFR leads to hypertrophy and an irreversible loss of nephron function from sustained increases in glomerular pressure (Song EY et al., 2013).
Glomerular capillary hypertension: Glomerulosclerosis (glomerular arteriolar damage) develops from prolonged elevation of glomerular capillary pressure and increased glomerular plasma flow leading to a continuous cycle of nephron destruction. A more rapid rate of decline in kidney function has been associated with black race, lower baseline eGFR, male gender, older age, and smoking
Progressive disease is typically identified by persistent proteinuria, decreasing kidney function, and the development of glomerulosclerosis. As the leading causes of ESRD in the United States, diabetes, hypertension, and glomerular diseases have been the focus of research to identify their associated mechanisms of kidney damage.
Excess filtration of glucose and contact with glomerular and tubular cells result in increased cellular osmotic pressure and thickening of the capillary basement membrane. The resulting glomerulopathy may or may not result in proteinuria. Systemic hypertension is a potent stimulus for the progression of kidney disease because of its association with increased single nephron eGFR.
Proteinuria: Proteinuria, one of the initial diagnostic signs, may also contribute to the progressive decline in kidney function, with a more rapid rate of progression associated with higher protein excretion. Immunologic and hemodynamic mechanisms have been identified to explain the glomerular injury and increase in renal plasma flow associated with proteinuria and high protein intake. Inflammatory cytokines may be responsible for fibrosis and renal scarring ultimately resulting in loss of nephron function (Mary Anne Koda-Kimble et al., 2008).
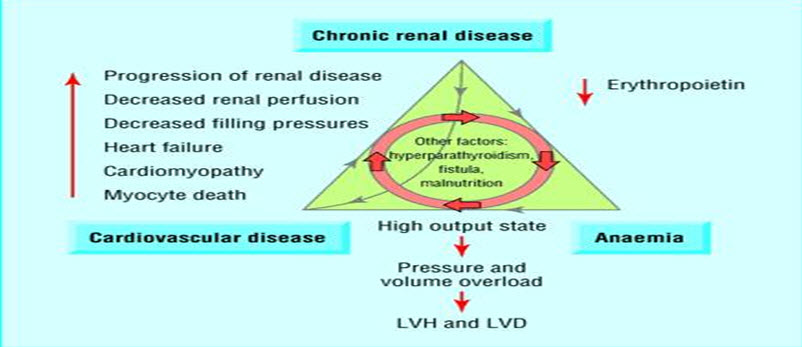
(LVH=left ventricular hypertrophy; LVD=left ventricular dilatation)
Fig.1: Triad of chronic kidney disease, anemia, and cardiovascular disease (James L. Holly MD, 2013)
Increased low-density lipoprotein (LDL) cholesterol, total cholesterol, and apolipoprotein B, as well as decreased high-density lipoprotein (HDL) cholesterol, have been observed in patients with progressive kidney disease.
Accumulation of apolipoproteins in glomerular mesangial cells contributes to cytokine production and infiltration of macrophages and has been implicated in the progression of CKD, primarily in the presence of previous kidney disease or other risk factors such as hypertension
LDL is thought to promote glomerular damage by initiating a series of cellular events in mesangial cells and through oxidation to a more cytotoxic derivative once within these cells. Although serum total cholesterol, triglycerides, and apolipoprotein B all correlate with the rate of decline in eGFR, it is not clear that they directly increase the rate of progression of kidney disease, particularly when present with concomitant conditions that also cause kidney damage. (Joseph T. DiPiro et al., 2011).
Anemia in CKD can result from multiple mechanisms (iron, folate, or vitamin B12 deficiency; gastrointestinal bleeding; severe hyperparathyroidism, systemic inflammation, and shortened red blood cell survival), decreased erythropoietin synthesis is the most important and specific etiology causing CKD-associated anemia. Erythropoietin is a glycoprotein secreted by the kidney interstitial fibroblasts and is essential for the growth and differentiation of red blood cells in the bone marrow. In CKD, tubular atrophy generates tubulointerstitial fibrosis, which compromises renal erythropoietin synthetic capacity and results in anemia (Ratcliffe PJ 1993).
CLINICAL PRESENTATION
CKD development and progression are insidious. Patients with stage 1 or 2 CKD usually do not have symptoms or metabolic derangements seen with stages 3 to 5, such as anemia, secondary hyperparathyroidism, cardiovascular disease (CVD), malnutrition, and fluid and electrolyte abnormalities that are more common as kidney function deteriorates. (Barbara G. Wells et al., 2015).
During stages 4 and 5, patients may develop the more severe signs and symptoms associated with advanced kidney disease, often referred to as the uremic syndrome (Mary Anne Koda-Kimble et al., 2008).
Uremic symptoms (fatigue, weakness, shortness of breath, mental confusion, nausea, vomiting, bleeding, and anorexia) are generally absent in stages 1 and 2, minimal during stages 3 and 4, and common in patients with stage 5 CKD who may also experience itching, cold intolerance, weight gain, and peripheral neuropathies (Barbara G. Wells et al., 2015).
DIAGNOSIS:
Physical examination: CKD patient includes a few specific points beyond general rules. Patient’s general health, nutritional status, appetite, and weight changes should be determined in each visit. Blood pressure and pulse should be assessed both in upright and supine positions for determining orthostatic changes.
Hypertensive or diabetic changes in the eye should be examined by fundoscopy. Patients should be examined for signs of hypovolemia or volume overload. Skin should be evaluated for finding an underlying disease and signs of CKD (anemia, pruritus, sallow appearance).
A careful evaluation of the cardiovascular system is important. The abdomen should be palpated for large kidneys and bladder distention. Abdominal bruits should be noted for potential renovascular disease.
Costovertebral tenderness may be a sign of infection and/or stone disease in kidneys. In men, rectal examination is required for determining prostatic enlargement (Kidney Disease. 2013)
Laboratory examination: The most reliable and practical means available to determine baseline kidney function and monitor progression of kidney disease over time is eGFR.
Serum creatinine, Creatinine clearance, and GFR estimating equations these are the most common methods used for assessing kidney function in clinical practice (Stevens LA et al., 2015).
Creatinine is an endogenous substance that is derived from the breakdown of muscle creatine phosphate. It is excreted primarily by glomerular filtration; thus, creatinine clearance (ClCr) has been used as a reasonable surrogate for eGFR (Mary Anne Koda-Kimble et al., 2008).
Creatinine clearance: Mesurements of creatinine clearance (ClCr) require accurate collection of 24 h urine samples with a serum creatinine sample midway through this period (Roger Walker. 2012).
ClCr = (U x V)/S
U is the urine creatinine concentration (µmol/L)
V is the urine flow rate (mL/min) and S is the serum creatinine concentration (µmol/L)
Cockroft–Gault formula (Mary Anne Koda-Kimble et al., 2008).
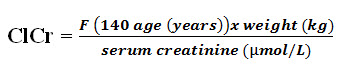
F = 1.04 (females) or 1.23 (males)
Serum creatinine: Serum creatinine is commonly measured by alkaline picrate (Jaffé method), enzymatic, or high-performance liquid chromatography (HPLC) methods. These different methods of measuring serum creatinine are recently standardized to the isotope dilution mass spectrometry (IDMS)
eGFR: GFR estimating equations based on serum creatinine were developed in order to eliminate several limitations of serum creatinine use. These equations were derived from different studies and populations and usually combine serum creatinine levels with other determinants of GFR like age, gender, and race and body size. The most common equations used are the Cockcroft- Gault, the Modifi cation of Diet in Renal Disease (MDRD) Study, and the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equations (Roger Walker. 2012).
eGFR (mL/min/1.73m2) = 186 x [serum creatinine (µmol/L)/88.4]–1.154 x [age] –0.203 x [0.742 if female] x [1.212 if African-American]
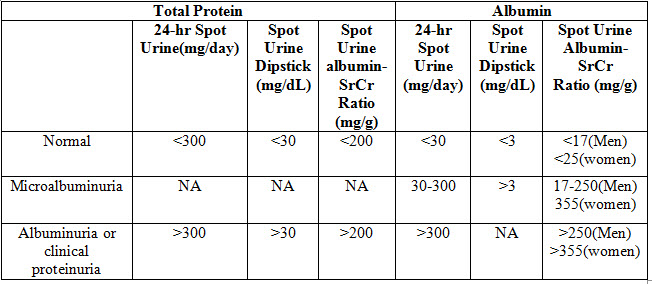
Proteinuria: In patients who have (or are at risk for) kidney disease, additional assessment of kidney function should include evaluation of urinary protein excretion, which has been shown to be predictive of disease progression.
Microalbuminuria is defined as an albumin excretion rate of 20 to 200 mcg/minute or 30 to 300 mg/24 hour. Specific assays with increased sensitivity relative to standard assays are required for detecting quantities of protein in the range defined as microalbuminuria. Proteinuria is defined as a total protein excretion rate >200 mcg/minute or >300 mg/24 hour (referred to as albuminuria if albumin is the only protein measured). Total protein includes albumin and other proteins, such as low molecular weight globulins and apoproteins (Myers GL. 2006).
Table:2 Diagnosis criteria from National Kidney Foundation. NKF-K/DOQI Clinical Practice Guidelines for Chronic Kidney Disease.
TREATMENT
Goals of therapy:
• To delay the progression of CKD, thereby minimizing the development or severity of associated complications including cardiovascular disease and ultimately limiting the progression to ESRD (Joseph T. Dipiro et al., 2011).
• To avoid conditions that might worsen renal failure.
• To treat the secondary complications of CKD (renal anemia and bone disease).
• To relieve symptoms.
• To implement regular dialysis treatment and/or transplantation at the most appropriate time (Roger Walker. Cate Whittlesea, 2012).
• The primary goal is to sustain a good quality of life and prevent adverse outcomes by aggressively managing complications of advanced CKD (Joseph T. DiPiro et al., 2011).
NON-PHARMACOLOGICAL
Dietary recommendations: Assessment of dietary intake of patients with CKD is important. Inadequate caloric intake and malnutrition are common problem among patients with advanced CKD (especially eGFR < 25). Protein. In general, an adequate protein intake of 0.8 g/kg per day is recommended for patients with CKD. High protein intake (> 1.3 g/kg/day) has been linked with CKD progression and should be avoided (The UMHS Clinical Guideline on Chronic Kidney Disease 2013).
Potassium, phosphorous, and sodium: Patients with CKD should be educated to be aware the intake of foods high in potassium (most important in the patients with hyperkalemia), phosphorous and sodium.
While the DASH diet has been proven efficacious for treatment of hypertension, hypertensive patients with CKD should follow caution when using the DASH diet due to its high intake of potassium and phosphate.
At all stages, CKD patients with hyperkalemia (> 5.5) should be advised to follow a low-potassium diet. Several web-based resources exist for patients regarding foods high in potassium and phosphorus (The UMHS Clinical Guideline on Chronic Kidney Disease, 2013; Joseph T. DiPiro et al., 2011).
Avoidance of nephrotoxic medications: Medications can cause or worsen kidney dysfunction and these effects are exacerbated in patients with underlying CKD. Many commonly used drugs, including over-the-counter medications, can cause nephrotoxicity (Joseph T. DiPiro et al., 2011).
Drugs that have been associated with nephrotoxicity should be used cautiously in these patient populations and concurrent use of multiple nephrotoxic agents should be avoided.
Physical activity: The NKF/KDOQI Guidelines recommend engaging in exercise for 30 minutes most days of the week. Data from the National Health and Nutrition Examination Survey III (NHANES III) have shown that physical activity was associated with lower mortality in patients with CKD of stage G3 or worse. Additionally, increased physical activity may lead to better control of hypertension, diabetes, and depression. Both aerobic and resistance exercises are beneficial (National Kidney Foundation. KDOQI Clinical Practice Guideline for Diabetes and CKD, 2012).
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT editor-in-chief@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
PHARMACOLOGICAL THERAPY
ANTI-HYPERTENSIVE THERAPY: Elevated blood pressure is often more difficult to control for patients with CKD than for those with normal kidney function.The association between BP and kidney disease is difficult to establish because hypertension is both a cause and a result of kidney failure. Hypertension, whether the primary cause of kidney disease or a coexisting disease in the presence of other aetiologies, can promote kidney damage through transmission of elevated systemic pressure to glomeruli. The result is glomerular capillary hyper perfusion and hypertension leading to progressive kidney damage as nephron destruction continues.
Antihypertensive therapy prevents kidney damage and slows the rate of progression of CKD in both diabetic and no diabetic patients. The added benefit of reduced cardiovascular mortality further supports the use of antihypertensive therapy in patients at risk for progressive CKD (Mary Anne Koda-Kimble et al., 2008).
The latest national guidelines from the Joint National Commission on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure VII (JNC VII) and the Kidney Disease Quality Outcome Initiative (K/DOQI) recommend blood pressure <130/80 as the goal of treatment for patients with CKD (Peralta CA et al., 2005; Andrew S. Levey et al., 2004).
First line hypertensive agents: Used includes Angiotensin Converting Enzyme Inhibitors (ACEI) or Angiotensin Receptor Blocker (ARB), when the GFR is >20ml/min/1.73m2.
Second and third line agents: If GFR is ≥ 40 ml/min/1.73 m2, then a thiazide diuretic and/or CCB is added if anti-Renin Angiotensin Aldosterone System (RAAS) agent is first line. A loop diuretic, e.g. Bumetanide or furosemide (twice daily dosing) or torsemide (once daily dosing) and/or CCB, is added in case of a GFR < 40ml/min and if anti-RAAS agent is started as first line therapy.
Fourth line agents: If heart rate is >80bpm a Beta blocker or alpha/beta blocker is addedwhereas if heart rate is < 80 bpm consider adding angiotensin receptor antagonist (ARA) (spironolactone or eplerenone), if protienuria present (Peralta CA et al., 2005).
Fig 2: Hypertension management algorithm for patients with CKD (Joseph T. DiPiro et al., 2011).

Anti-Hypertensive Drugs
Angiotensin-converting enzyme inhibitors [ACE] and angiotensin receptor blockers [ARBs]: ACE inhibitors reduce circulating angiotensin II and ARBs block binding to the angiotensin II receptor, which results in vasodilatation and reduced sodium retention. The role of ACE inhibitors in hypertensive patients with renal insufficiency is complicated, the current evidence base supports the principle that all diabetic patients with micro/macro albuminuria and CKD should be treated with ACE inhibitors or ARBs regardless of blood pressure. There is also evidence that in non-diabetic patients with proteinuria, the use of these drugs can reduce proteinuria and thus reduce progression of CKD.
Calcium channel blockers [CCBs]: For patients without proteinuria, calcium channel blockers (CCBs) are the agents of choice. They produce vasodilatation principally by reducing Ca2+ influx into vascular muscle cells. CCBs also appear to promote sodium excretion in hypertension associated with fluid overload. The mechanism is unclear but may relate to the finding that high sodium levels can cause vasoconstriction by interfering with calcium transport. Both verapamil and diltiazem (non-dihydropyridine CCBs) block conduction across the atrioventricular node and should not be used in conjunction with β-blockers.
Diuretics: Diuretics are of use in patients with salt and volume overload, which is usually indicated by the presence of edema. This type of hypertension may be particularly difficult to treat. The choice of agent is generally limited to a loop diuretic. Potassium sparing diuretics are usually contraindicated owing to the risks of developing hyperkalemia, and thiazides become ineffective as renal failure progresses. In combination with ACE inhibitors, spironolactone can significantly reduce proteinuria; however, the combination of these agents clearly raises the risk of significant hyperkalemia and care must be taken.
Β-Blockers: β-Blockers are commonly used in the treatment of hypertension in CKD. They exhibit a range of actions including a reduction of renin production. Consequently, β-blockers have a particular role in the rational therapy of hypertension without fluid overload. However, β-blockers can reduce cardiac output, cause peripheral vasoconstriction and exacerbate peripheral vascular disease. It is advisable to use the more cardio selective β-blockers atenolol or metoprolol. Atenolol is excreted renally and consequently should require dosage adjustment in renal failure.
Selective α1-blockers: These vasodilators produce a variety of actions that may be of benefit in hypertension associated with CKD. Sympathetic adrenergic activity can lead to sodium retention.
Centrally acting drugs: Methyldopa and clonidine are not commonly used as antihypertensives in CKD because of their adverse side effect profiles. If they are used in renal failure, initial doses should be small because of increased sensitivity to their effects (Andrew S. Levey et al., 2004).
Vasodilators: The vasodilators hydralazine and minoxidil have been used to treat hypertension in CKD with varying degrees of success but are usually only used when other measures inadequately control blood pressure (Roger Walker. Cate Whittlesea, 2012).
DIABETIC CHRONIC KIDNEY DISEASE
Intensive Insulin Therapy:
Several large prospective studies performed in the 1990s showed the benefits of blood glucose control in both the development and progression of micro vascular complications. The Largest of these studies, the DCCT enrolled 1,441 Patients with type 1 diabetes mellitus who were randomized to conventional blood glucose control or to intensive glucose control. Conventional control consisted of up to two insulin injections per day guided by blood glucose levels. Intensive control consisted of three or more times daily injections or external insulin pump to a goal haemoglobin A Renal Disorders = 6.0% (=0.06).The main outcome measure of efficacy was retinopathy, a marker of micro vascular disease often associated with diabetic nephropathy among individuals with type 1diabetes mellitus. Roughly half of the patients had mild retinopathy. Intensive insulin control reduced the risk of new occurrences of retinopathy by 76% among those without baseline retinopathy and reduced the risk of progressive retinopathy by 54% among those with baseline retinopathy. Intensive therapy was also associated with a 39% reduction in the development of “micro albuminuria” (urinary albumin excretion=40 mg/day) and a 54% reduction in the development of “frank albuminuria” (urinary albumin excretion =300 mg/day) compared with conventional therapy. The beneficial effect of intensive therapy on the development of proteinuria persisted even 7 to 8 years after completion of the randomized phase of the DCCT. Individuals initially randomized to the intensive therapy had a 59% reduction in the development of new micro albuminuria, and 84% reduction in the development of albuminuria compared with the conventional group. In the intensive therapy group, follow-up after 30 years of diabetes demonstrated a lower cumulative incidence of diabetic nephropathy (9% vs 25%).However, at least one episode of hypoglycaemia occurred in 65% of intensive insulin therapy patients as compared with 35% in the standard treatment group (Joseph T. DiPiro et al., 2011).
END STAGE RENAL DISEASE [ESRD]:
As ESRD becomes inevitable, the appropriate dialysis modality must be selected based on patient preference and options for vascular access for HD or peritoneal access for PD. Early planning for dialysis therapy and timely initiation may lower patient morbidity and mortality. Kidney transplantation is an option for all patients with ESRD without specified contraindications if a suitable organ match is available.
Pharmacotherapy:
Pharmacotherapy in patients with ESRD involves interventions to manage comorbid conditions and complications. The extent of medication use, including medications administered during dialysis therapy, contributes to the potential for drug interactions, adverse reactions, and no adherence to therapy. The effect of decreased kidney function on absorption, distribution, metabolism, and elimination of pharmacologic agents, in addition to the contribution of dialysis to drug removal, further complicates pharmacotherapy in this population (Mary Anne Koda-Kimble et al., 2008).
Other Interventions to Limit Disease Progression:
Hyperlipidaemia Treatment: Although several drugs are available for lipid lowering, the ß-hydroxy-ß-methylglutaryl coenzyme A (HMG-CoA) reductase inhibitors, or statins, and gemfibrozil have been most often used in dyslipidemic patients with CKD with and without proteinuria. The primary goal of treatment is to decrease the risk for progressive atherosclerotic cardiovascular disease. Additionally, a prior meta-analysis of 13 studies of lipid-lowering agents also showed a reduction in the rate of CKD progression by 0.156 mL/min per month. Mechanisms for this effect are unknown, but statins may reduce proteinuria, inflammation and fibrosis.
Anaemia Treatment: Prolonged anaemia is associated with left ventricular hypertrophy and heart failure. It has been suggested that anaemia may increase the rate of CKD progression. Researchers have coined the phrase “cardio renal anaemia syndrome” To describe the interrelationship between anaemia, heart failure and CKD. Tissue hypoxia associated with anaemia could be a stimulus for continued renal injury in those with stages 3 to 5 CKD. Although, at present, no definitive studies have been performed, some have hypothesized that the treatment of heart failure and anaemia may reduce the progression of both heart failure and CKD (Joseph T. DiPiro et al., 2011).
CURRENT RESEARCH STATUS ON CKD:
Jay Shah et al (2017) carried out a prospective observational study on Drug utilization pattern of antihypertensive agents in patients of hypertensive nephropathy in a tertiary care hospital Evaluation of the prescriptions demonstrates that a total of 63.3% males and 36.7% females with mean age of 58.9±11.9 years were enrolled out of which 70% patients were on multidrug therapy while only 30% were on monotherapy. Though only 16.67% patients were prescribed generic drugs but it did not affect the economic condition of the patient as most of enrolled patients belong to upper middle class (Shah J. Balraj A, 2017).
Neethu Joseph et al (2017) carried out prospective observational study A Study on Prescription Pattern of Antihypertensive Agents in Chronic Renal Failure Patients and Assessment of Medication Adherence. There is a strong relationship between Hypertension (HTN) and Chronic Kidney Disease (CKD). HTN is an important cause and highly prevalent in CKD patients, contributing to the high cardiovascular risk for this particular population. This study aims in the management of HTN in CKD patients. The objective of the study is to assess prescription pattern of antihypertensive agents in Chronic Kidney Disease patients and to assess the medication adherence. A total of 120 CKD patients with HTN were the participants of this study. Among 120 participants 72.5% were males and 27.5% were females. 34.2% were found between the age group of 60-69 years. Among the population, 50% of patients were smokers. The recorded value of systolic blood pressure was 172.17±21.309 and diastolic blood pressure was 97.33±13.704. It was found that 89 74.16% of patients were prescribed with Calcium channel blockers. The most commonly prescribed Calcium channel blockers was Amlodipine 50% and most participants were treated with Multi-drug therapy. Medication adherence of the participants had a significant difference between first visit & follow up at 5% level of significance with p value o.ooo. In CKD patients the use of antihypertensive drugs did not diverge from the National Kidney Foundation Kidney Disease, Outcome Quality Initiative guidelines. The Pharmacist can play a major role in the medication adherence of CKD Patients (Neethu Joseph et al., 2017).
Ansuman Abhisek et al (2016) Carried out a prospective study on drug utilization of anti-hypertensive in ckd patients .Total 100 case records were analyzed. Mean age was 55.37±13.41 years. Male-female ratio was 2.7. Maximum number of patients were from age group 51-60 years (43%) followed by age group 41-50 years (29%). All the patients (100%) were hypertensives, among which 42% patients of the study population were diabetic with hypertension and rest of the patients (58%) were non-diabetic with hypertension. Routinely prescribed anti-hypertensives are CCB, β blockers, diuretics, α blockers, ACEI and centrally acting sympatholytics. Among them, Calcium Channel Blockers (32.47%) were most frequently used followed by β Blockers (24.78%), Diuretics (23.50%), Centrally Acting Sympatholytics (10.25%), α Blockers (7.69%) and ACE Inhibitors (1.28%). Hypertension in CKD patients was very difficult to manage. Approximately, two-third of the patients (66%) had BP >140/90 mmHg with anti-hypertensive therapy. Targeted blood pressure control was present in (34%) of the patients (Abhisek PA et al., 2016).
Noah Jarari et al (2016) carried out a study on review on prescribing patterns of antihypertensive drugs. Hypertension continues to be an important public health concern because of its associated morbidity, mortality and economic impact on the society. It is a significant risk factor for cardiovascular, cerebrovascular and renal complications. It has been estimated that by 2025, 1.56 billion individuals will have hypertension. The increasing prevalence of hypertension and the continually increasing expense of its treatment influence the prescribing patterns among physicians and compliance to the treatment by the patients. A number of national and international guidelines for the management of hypertension have been published. Since many years ago, diuretics were considered as the first-line drugs for treatment of hypertension therapy; however, the recent guidelines by the Joint National Commission (JNC8 guidelines) recommend both calcium channel blockers as well as angiotensin-converting enzyme inhibitors as first-line drugs, in addition to diuretics. Antihypertensive drug combinations are generally used for effective long-term management and to treat comorbid conditions. This review focuses on the antihypertensive medication utilization, their cost factors, adherence to treatment by patients, and physicians’ adherence to guidelines in prescribing medications in different settings including Indian scenario. The antihypertensive medication prescribing pattern studies help in monitoring, evaluation and necessary modifications to the prescribing habits to achieve rational and cost-effective treatment. Additionally, periodic updating of recommended guidelines and innovative drug formulations, and prescription monitoring studies help in rational use of antihypertensive drugs, which can be tailored to suit the patients' requirements, including those in the developing countries (Noah Jarari et al., 2016).
Ajay Kumar Lal Das et al (2015) carried out a study on Prescribing Pattern of Antihypertensive drugs was analyzed on all diabetic patients reporting to medicine OPD. Results: Out of n=446 patients, 242 were males and 204were females. Mean age of group was 48.6 years. 46.18% patients were on monotherapy and remaining patients were on combination antihypertensive drugs. There were total 796 antihypertensive drug exposures. Patient needed mean antihypertensive drug of 1.78. Angiotensin receptor blockers were the most commonly prescribed drugs. Angiotensin inhibitors (angiotensin receptor blockers and ACE inhibitors) were utilized in 71% patients. Hypertension control was achieved in 37.66% patients. About 81.2%) aware about disease (Ajay Kumar Lal Das 2015).
Anju Madhwar et al (2015) carried out a prospective observational study. A total of 60 patients aged 40-79 years taking treatment for hypertension with associated nephropathy were enrolled in the study. All the relevant data were collected and drug utilization pattern of antihypertensive agents was determined. The study evaluated the percentage of use of multidrug therapy, drugs prescribed from Essential Drug List (EDL) and prescriptions with generic name. The cost of antihypertensive drugs used per day was calculated and linked with socioeconomic status of the patients. Results: Evaluation of the prescriptions demonstrates that a total of 63.3% males and 36.7% females with mean age of 58.9±11.9 years were enrolled out of which 70% patients were on multidrug therapy while only 30% were on monotherapy. The most common drug prescribed was amlodipine and around 60% drugs were from EDL 2011. Though only 16.67% patients were prescribed generic drugs but it did not affect the economic condition of the patient as most of enrolled patients belong to upper middle class. Conclusion: The prescriptions analysed were in accordance to guidelines of JNC-8 (Joint National Committee – 8) and most of the prescriptions were found to be rational and it also shows that management of hypertensive nephropathy needs combination therapy (Anju Madhwar et al., 2015).
Soumya Santra et al (2015) carried out a cross-sectional, observational study that was conducted over a period of 6 months The Mean age of CKD patients was 45.81 ± 11.16 with male predominance (58%). CKD Stage I -II comprised of the maximum number (28%) of patients. Polypharmacy was executed in 83% of these patients. Hypertension (95%), diabetes (87%), and anemia (86%) are the most common co-morbidities. The five most frequently prescribed drugs were diuretics (100%), anti-ulcer agents like proton pump inhibitors and H 2 blockers (98%), anti-hypertensives (95%), vitamins and minerals supplements including calcium (92%), and hematinics (85%). Infectious diseases like respiratory tract infection (37%) and urinary tract infection (34%) had shown to have a high prevalence in CKD patients. Cefoperazone, metronidazole, piperacillin + tazobactam were the most prescribed parenteral antibiotics. Azithromycin and levofloxacin were the extensively used oral antibiotics (Soumya Santra et al., 2015).
Elahe Elhami et al (2015) carried out a Retrospective observational study was conducted from March 2010 to August 2015 in 120 diabetic patient with CKD admitted to General Medicine at KIMS hospital, Bangalore. This study results were about (39.78%) of the patients are been prescribed with ACEI’s in accordance with the JNC 7 guideline. and most of drugs were found to be rational and it also shows the management of hypertension in DM patients with CKD needs combination therapy (Elahe Elhami, 2015).
Bhanu Priya B et al (2015) carried out a cross sectional study conducted in patients with Chronic Kidney Disease in a tertiary care hospital over a period of 6 months in 2014. The information regarding demographic details and antihypertensive drugs prescribed were collected from the patient’s case records and the data was compiled and subjected to statistical analysis.Total of 95 case records was analyzed. CKD was more common in males, with male to female ratio of 4:1. 49.47% of the patients belonged to the age group of 40 – 60 years followed by 31 – 40 years (26.32%). Among the antihypertensives calcium channel blockers, diuretics, centrally acting antihypertensives, β blockers, α blockers, vasodilators, α+β blockers and ACE inhibitors were routinely used (Bhanu Priya B. Basavanna P L, 2015)
Rajiv Ahlawat et al (2012) carried out a cross section study on Drug Utilization Evaluation of Antihypertensive agents in nephrology department in tertiary care hospital. Patients diagnosed with CKD according to KDIGO guideline were included in the study. Medications were classified into different groups on the basis of Anatomic Therapeutic Chemical (ATC) classification. A total of 408 patients diagnosed with CKD were included in study. The average age of the patients was 53.8 (6.4). Of all, 18% of the patients were on dialysis. It was found that 42% of the patients belonged to end stage of renal disease. The mean (SD) of drugs was found to be 6.57 (2.3). Only 19% of the drugs prescribed out of Indian National List of Essential Medicine (NLEM). No drug was found to be prescribed by generic name. Out of total 2,681 drugs prescribed, most commonly prescribed were cardiovascular drugs (33.9%). Further, it was also found that 14.7% of the patients were prescribed with antimicrobials. Among all, 22.3% of the patients were vaccinated with hepatitis B vaccine. Five most commonly prescribed drugs were calcium carbonate, vitamin D, iron, torsemide and amlodipine (13.9%, 12.2%, 11.5%, 8.1% and 6.1%, respectively). Ninety-five percent of the patients were prescribed phosphate binder (PB). Calcium carbonate was the most commonly used PB prescribed to 91.1% of the patients. Sevelamer was prescribed to only 18 patients (Rajiv Ahlawat et al., 2012).
Arshad H. Mohd et al (2012) carried out a Prospective observational study on prescribing patterns of antihypertensives in geriatric patients a total of 100 prescriptions were analyzed during the six-month study period. 72% of the patients were in the age group of 65-67 years and this was found to be higher in men 69%. During the study period 80% of the patients were Pre-Hypertensive systolic (80-89 mmHg) and Diastolic (120-139 mmHg) followed by Stage-I Hypertension and Stage-II Hypertension. The most common drug classes involved in the study was Calcium Channel Blockers 37% followed by Angiotensin II receptor antagonists 21% and the most commonly prescribed drugs in the study population were Amlodipine 37%, Losartan 11% and Telmisartan 10%. The most common anti-hypertensive fixed dose combination therapy involved in the study was Telmisartan + Hydrochlorothiazide 15% and most common two drug combination therapy involved in the study was Amlodipine + Atenolol 7% followed by Metoprolol + Amlodipine 1% (Arshad H. Mohd et al., 2012)
Al Ramahi R et al (2012) carried out a prospectively studied cohort study on Medication prescribing patterns among chronic kidney disease patients in a hospital in Malaysia on 600 patients in two phases with 300 patients in each phase on Medication prescribing patterns among chronic kidney disease patients in a hospital prospectively studied a cohort of 600 patients in two phases with 300 patients in each phase. The first phase was carried out from the beginning of February to the end of May 2007, and the second phase was from the beginning of March to the end of June 2008. Patients with CKD who had an estimated creatinine clearance ≤ 50 mL/min and were older than 18 years were included. A data collection form was used to collect data from the patients' medical records and chart review. All systemic medications prescribed during hospitalization were included. The patients were prescribed 5795 medications. During the first phase, the patients were prescribed 2814 medication orders of 176 different medications. The prescriptions were 2981 of 158 medications during the second phase. The mean number of medications in the first and second phases was 9.38 ± 3.63 and 9.94 ± 3.78 respectively (P-value = 0.066). The top five used medications were calcium carbonate, folic acid/vitamin B complex, metoprolol, lovastatin, and ferrous sulfate. The most commonly used medication classes were mineral supplements, vitamins, antianemic preparations, antibacterials, and beta-blocking agents. This study provides an overview of prescription practice in a cohort of hospitalized CKD patients and indicates possible areas of improvement in prescription practice (Al-Ramahi R, 2012).
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT editor-in-chief@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
METHODOLOGY
PLAN OF WORK:
A study was carried out to evalute the Drug utilisation of anti hypertensive drugs used in in patient with Chronic kidney disease . All the Antihypertensivedrugs containing prescription were monitored to know the frequency extent of Antihypertensivedrugs use and also the conditions in which it was prescribed.
A. To evaluate the clinical use of Antihypertensive drugs in CKD.
B. To compare the utilization of different types of Anti-hypertensive therapies.
C. To assess blood pressure.
D. To assess medication adherence in CKD patients.
Literatures which support the study were collected and were reviewed for study on clinical use of antihypertensive therapy in Chronic kidney Disease. A standard data entry format for collecting patient’s details was designed and during the ward rounds the entire patient data with special reference to the antihypertensivedrugs prescribed were recorded in the format.
STUDY SITE:
In-Patient of Nephrology Department at Gleneagles Global Hospitals, Bairamalguda, LB Nagar, Hyderabad.
The study was conducted in the Nephrology Department, Gleneagles Global Hospitals. It is a 300 bedded multispecialty hospital which has intensive care units with 50 beds, General wards with 80 beds and twin sharing rooms with 96 beds and medical sharing with 74 beds providing its health care services with around 40 physicians, 8 surgeons and around 30 Duty medical officers and 1 clinical pharmacist located in Bairamalguda, LB Nagar, Hyderabad. It has rendered its services in the entire state. It is a massive building with expertise in various fields in hospital services.
STUDY DESIGN:
A hospital based prospective observational study was carried out on 184 in-patients in general medicine wards.
The data was collected which contains patients demographics (age, sex), date of admission, date of discharge, history of present illness, past medical history, diagnosis, name of the drugs, dosage regimen (form, dose, route, frequency and duration). The knowledge assessment questionnaire form contains about 13 questions to assess the knowledge of patient towards the medications used.
SAMPLE SIZE:
A total of 184 in-patients from the in-patient of Nephrology department in Gleneagles Global Hospital, who were prescribed Anti-hypertensive drugs those who fulfilled the exclusion and inclusion criteria were selected for the study.
STUDY PERIOD:
The study was carried out for a period of six months.
STUDY CRITERIA:
Inclusion Criteria
• Patients aged between 18 years to 90years.
• Patients of either sex with a prescription of mentioned drugs.
• Patients with and without co-morbidities.
• Smoking status.
• Alcoholic status.
• Dialysis Patients
Exclusion Criteria
• Pregnancy patients
• Patient below 18 years of age
• Patients with renal transplant.
• Surgical conditions like kidney stone, tumors and trauma.
STUDY APPROVAL
The study was approved by Ethical Committee of Sree Dattha Institute of Pharmacy. Permission for collection of data and to accompany physician in the Nephrology Department was taken from the Head of the nephrology Department before starting the study. The authors were permitted to utilize the hospital facilities and make a follow up with prescriptions in the department.
SOURCES OF DATA:
Patient Profile Form:
• Patient demographic details (age, sex, alcoholic status, smoking status)
• Chief complaints
• History of present illness
• Past medical and medication history
• Family history
• Final diagnosis
• Name of the drugs
• Dosage regimen (form, dose, route, frequency and duration)
• Date on which pharmacotherapy was initiated
• Laboratory data
Knowledge Assessment Questionnaire Contains The Following Questions:
• Are you anemic?
• Are you a smoker?
• Do you smoke now?
• When did you quit smoking?
• Do you consume alcohol?
• Have you ever felt you should stop consuming alcohol?
• Did you suffer with pedal edema?
• Do you have hypertension?
• From how long you are suffering with hypertension?
• What is the medication you’re using for hypertension?
• From how long you’re suffering with chronic kidney disease?
• Did doctor did any change in antihypertensive drugs after you diagnosed with chronic kidney disease?
• From how long you’re going through hemodialysis?
DETERMINATION OF PRESCRIBING PATTERNS:
A suitable data collection form was designed and used.
Data was collected with respect to:
• Demographic details: name, age, sex
• Condition and reasons for hospital admission were recorded
• Drug data: Brand and generic name of the drugs prescribed, dose, route of administration, frequency and their follow up for few days was recorded.
STATISTICAL SOFTWARE:
• SPSS Programme.
RESULTS
Population Description: A total of 184 patients with presumed/confirmed CKD. The Mean for Age is 59.29 and the standard deviation was 15.145. Of the population, 72.80% were males and 27.10% were females, 60% were smokers and 40% were non-smokers. The main demographic and clinical characteristics, co-morbidities have been described later.
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT editor-in-chief@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
Table: 3 Distribution of subjects based upon age in CKD (%)
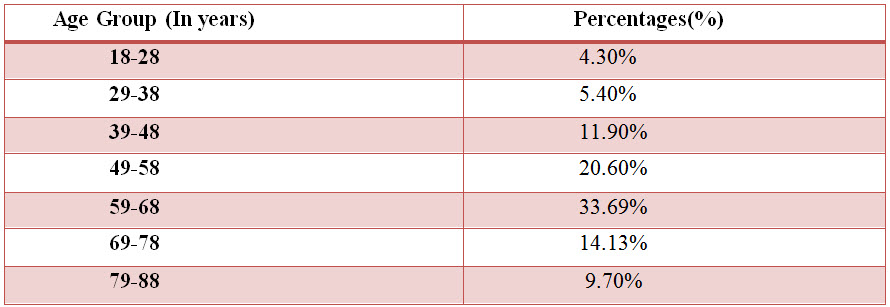
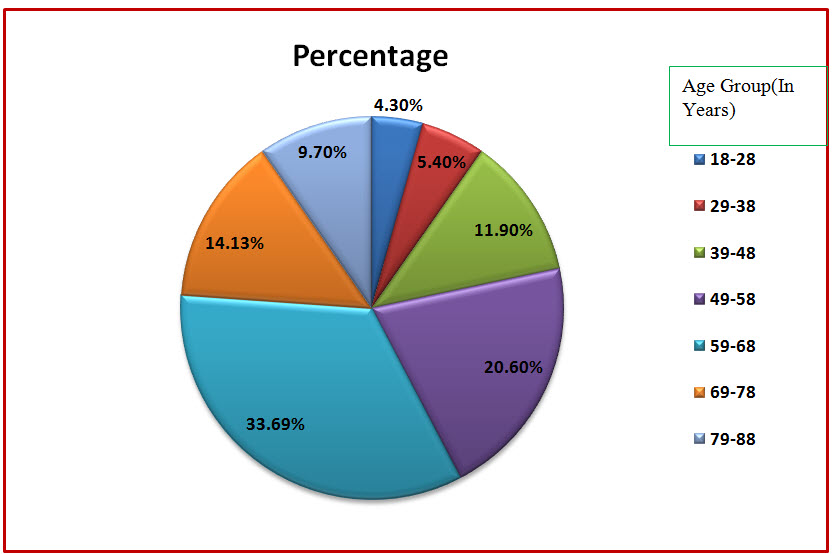
Figure: 3 Pie chart presentation of distribution of subjects based upon age in CKD (%)
Among the study population, 62 individuals belonged to the age group of 59-68 years, 38 individuals belonged to the age group of 49-58 years, 26 individuals belonged to the age group of 69-78 years, 22 individuals belonged to the age group of 39-48 years, 18 individuals belonged to the age group of 79-88 years, 10 individuals belonged to the age group of 29-38and 8 individuals belonged to 18-28.
Table 4: Statistical Presentation of the age group data by Column Statistics
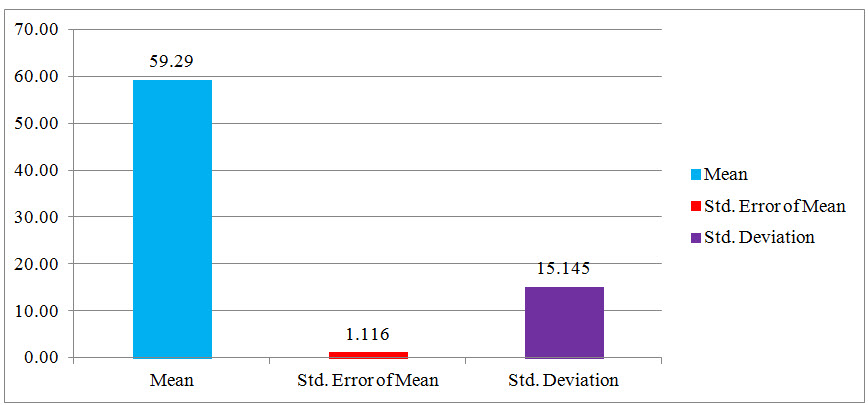
Fig: 4 Column Statistical Presentation of the age group data
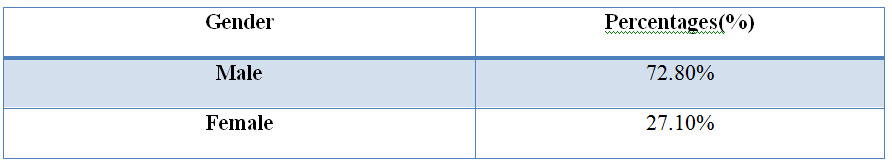
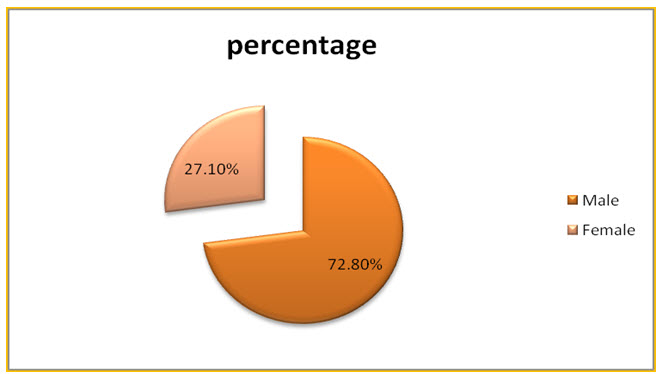
Figure: 5 Pie chart presentation of distribution of subjects based on gender in CKD (%).
Among the study population, 134 individuals were found to be males and 50 individuals were females.
Table: 6 Distribution of subjects based upon social history in CKD (%).
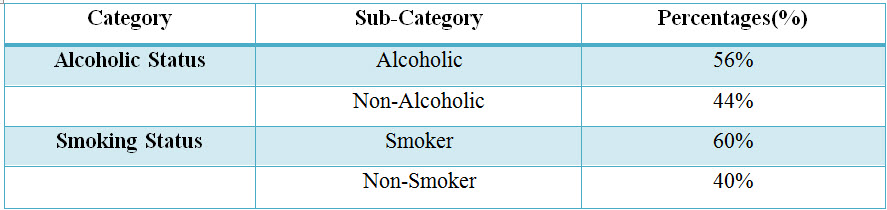
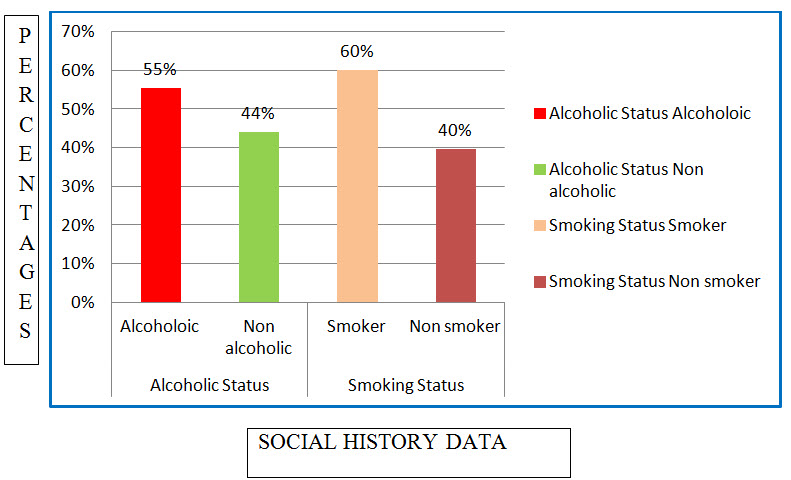
Figure: 6 Column presentation of distribution of subjects based upon social history in CKD (%)
Among the study population, 102 individuals were alcoholics and 111 of individuals were Smokers and an 82 individuals were non-alcoholics and 73 individuals were non-smokers.
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT editor-in-chief@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
Table: 8 Results of CKD Severity Assessment (%)
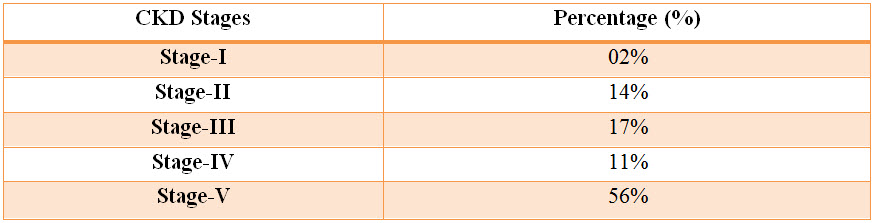
Figure: 8 Column presentation of results of CKD Severity Assessment
Among the study population, 02% of patients resulted with Stage-I severity, 14% of patients resulted with Stage-II severity, 17% of patients resulted with Stage-III severity and 11% of patients resulted with Stage-IV severity and 56% of patients resulted with Stage-V severity.
Table: 9 Percentage of stages of hypertension in CKD patients:
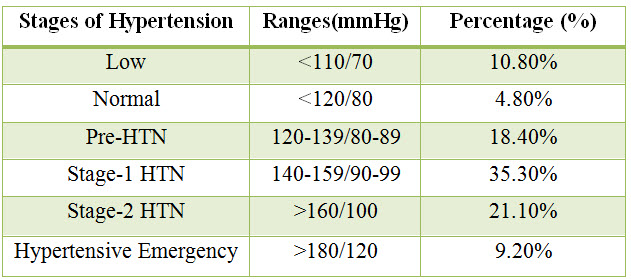
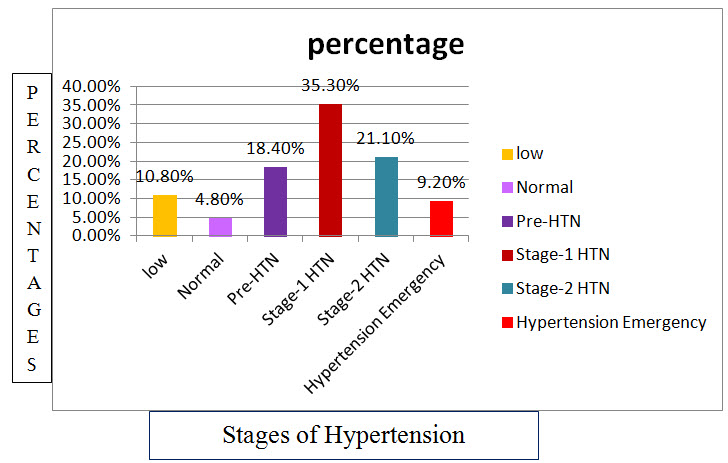
Figure: 9 Column presentation of percentage of stages of hypertension in CKD patients.
Among the study population, 10.8% of patients resulted with low blood pressure, 4.8% of patients resulted with normal blood pressure,18.4% of patients resulted with pre-HTN, 35.3% of patients resulted with stage-1 HTN ,21.1% of patients resulted with stage-2 HTN and 9.20% of patients resulted with hypertensive emergency.
Statistical Presentation of the Data
Table: 10 Table for one Stastical presentation of Blood pressure
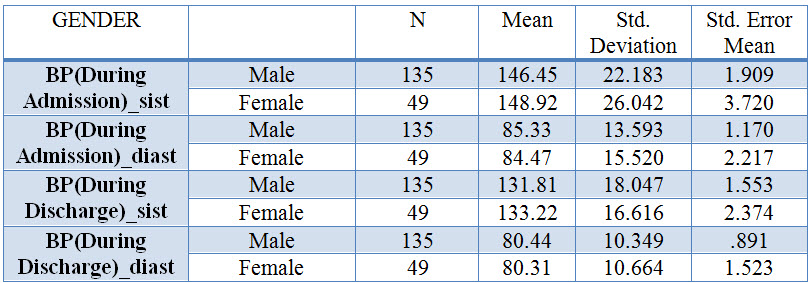
Table: 11 T-Test: Paired Two Sample for Means
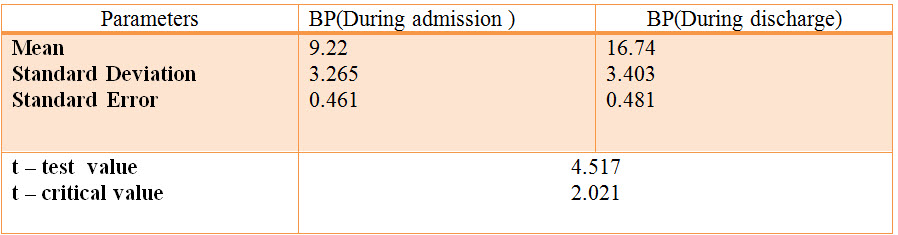
Degree of freedom: 183
Calculated paired t-value: 4.517
Table value of t at 5% level of significance: 2.021
The above table shows that the blood pressure (During Admission) mean is 9.22and the Blood pressure (During discharge) is 16.74. The calculated value of t is 4.517 which is very much higher than the tabulated‘t’ value 2.021 at 183 degree of freedom with 5% level of significance. Hence it shows that there is a significance difference between the knowledge score of Blood pressure (During Admission) and Blood pressure (During Discharge).
Table: 12 Percentage of anti-hypertensive drug classes used in CKD.
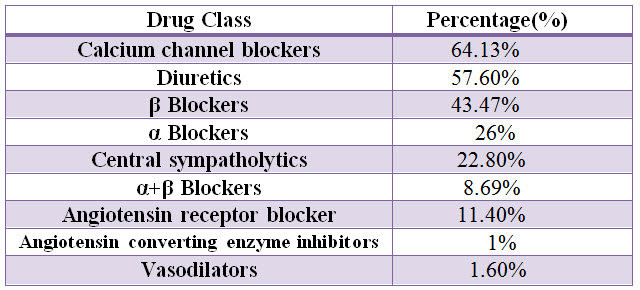
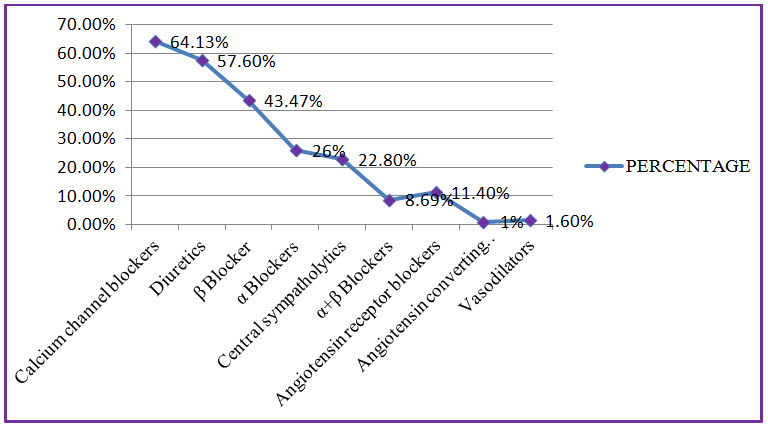
Figure: 10 Line presentation of percentage of class of anti-hypertensive drugs used in CKD.
Among the study population, most commonly used class of antihypertensives are Calcium channel blockers with percentage of 64.13%, Diuretics with percentage of 57.60%, β blockers with percentage of 43.47%.
Table: 13 List and percentage of Calcium channel blockers used in CKD:

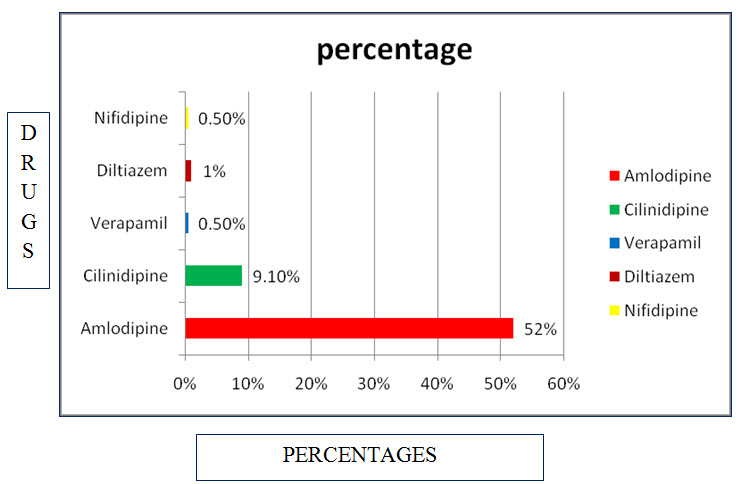
Figure 11 : Bar presentation for use of calcium channel blockers in CKD.
Among study population most commonly used calcium channel blockers are Amlodipine with percentage of 52%, and Cilindipine with percentage of 9.10%.
Table: 14 List and percentage of Diuretics used in CKD

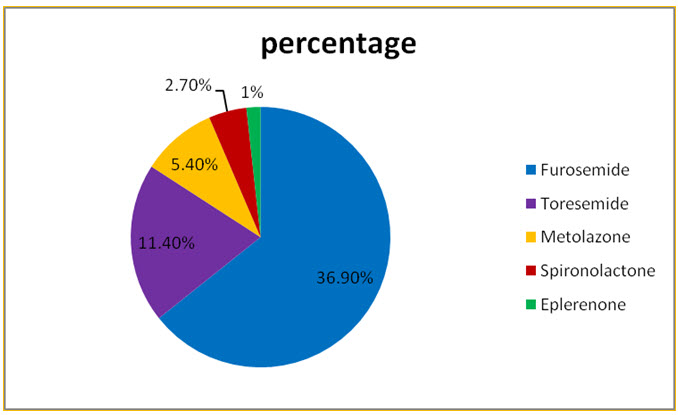
Figure: 12 Pie presentation for percentage of Diuretics used in CKD
Among study population commonly used Diuretics are Furosemide with percentage of 36.90% and Toresemide 11.40%.
Table: 15 List and percentage of adrenergic antagonists used in CKD.
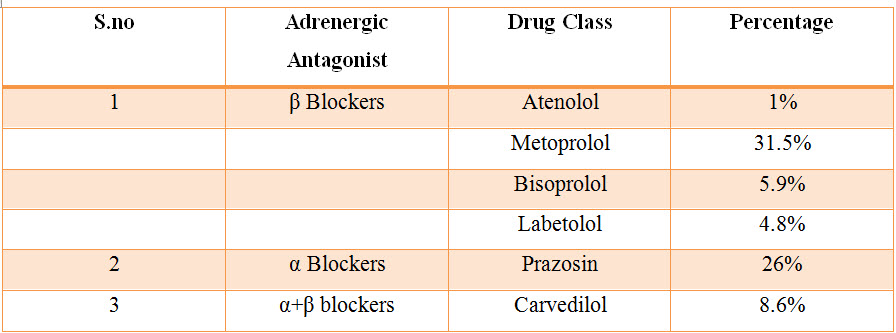
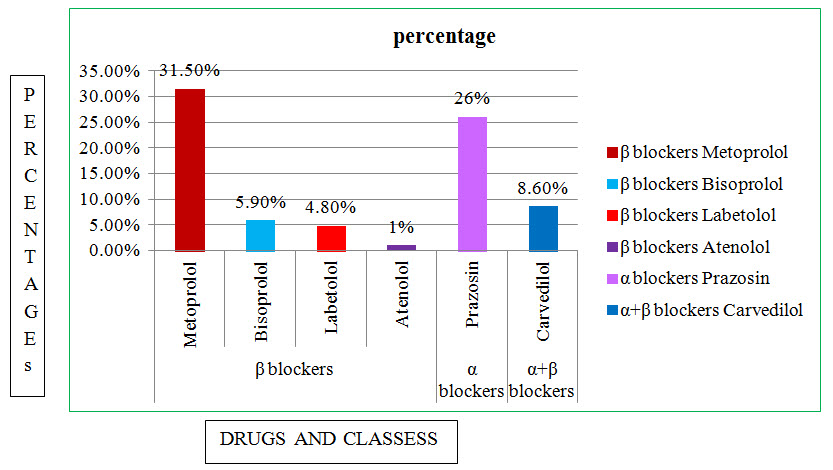
Figure: 13 Column presentation of Adrenergic antagonists used in CKD.
Among the study population most commonly used Adrenergic Antagonist are in β Blockers are Metoprolol with percentage of 31.50%,In α blockers are prazosin with percentage of 26%,In α+β blocker are Carvedilol with percentage of 8.60%.
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT editor-in-chief@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
Table: 16 List and percentage of ARB’s and ACE’s used in CKD.

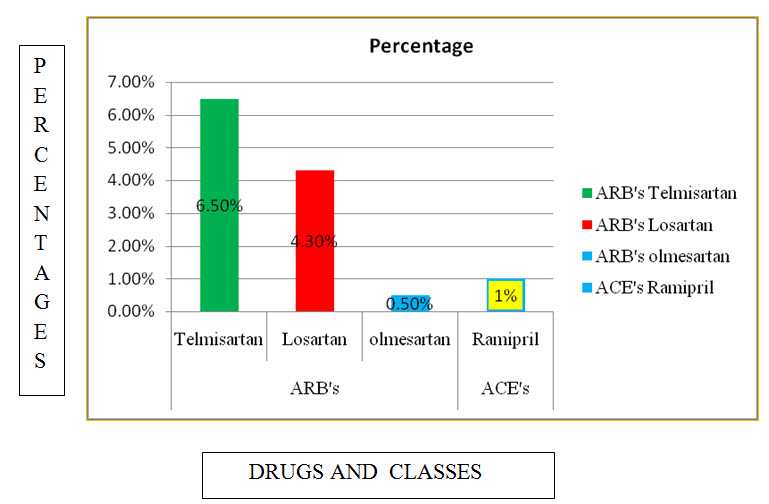
Figure:14 Coloumn presentation of percentage of ARB’s and ACE’s used in CKD.
Among the study population most commonly used ARB’s are Telmisartan with percentage of 6.50%, and ACE’s are Ramipril with percentage of 1%.
Table: 17 List and Percentage of Central sympatholytics and Vasodilators used in CKD.
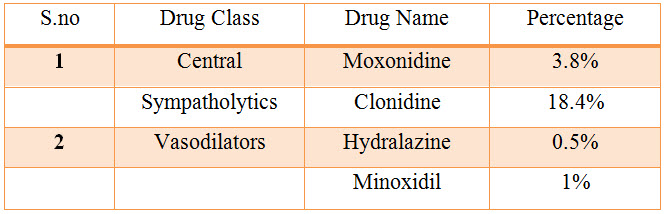
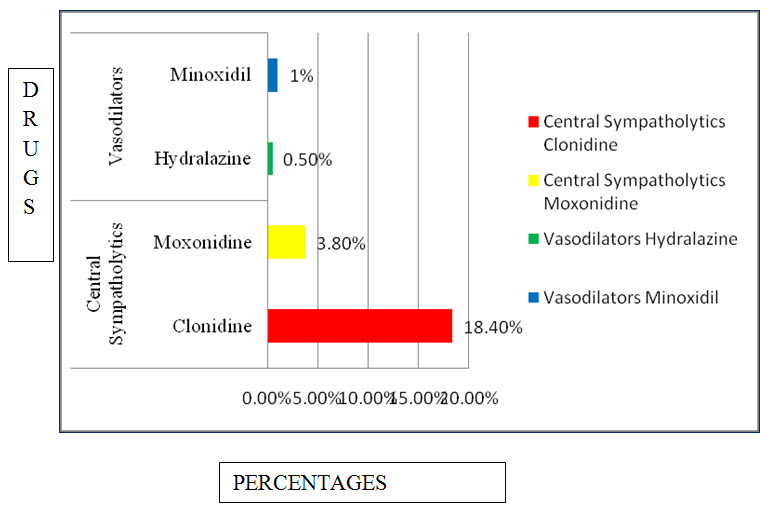
Figure: 15 Bar presentation of percentage of central sympatholtyic and vasodilators used in CKD.
Among the study population most commonly used central sympatholytics are Clonidine with percentage of 18.40%, Vasodilators are Minoxidil with percentage of 1%.
Table:18 Percentage of Antihypertensive combination used in CKD
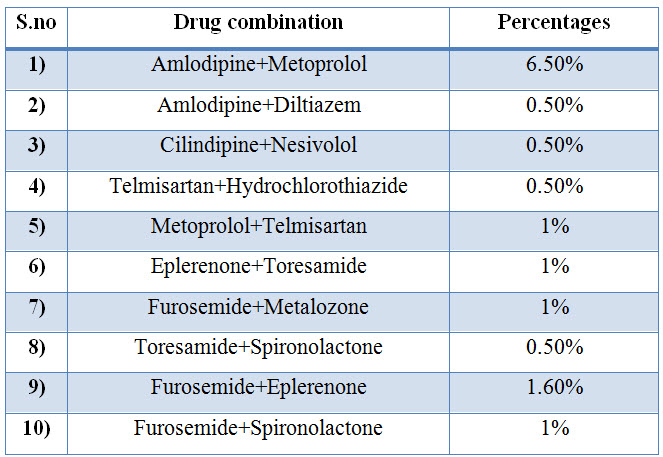
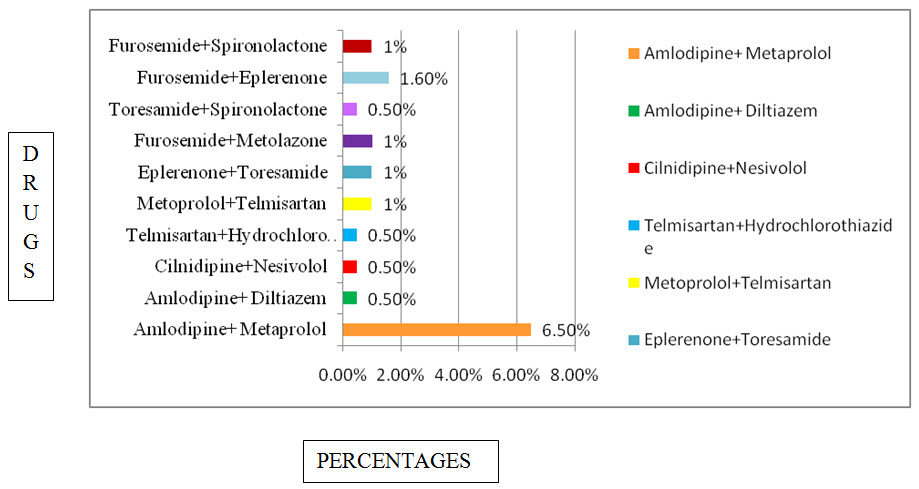
Figure:16 Bar presentation for percentage of Antihypertensive combination used in CKD
Among the study population most commonly used Antihypertensive combinations are Amlodipine + metoprolol with percentage of 6.50%,and Furosemide+Eplerenone with percentage of 1.60%.
Table:19 Percentage of types of anti-hypertensive therapies prescribed in CKD patients:


Figure: 17 Pie chart presentation of percentage of types of anti-hypertensive therapies in CKD patients.
Among the study population 8.15% of patients are prescribed with monotherapy of antihypertensives, 34.87% of patients are prescribed with dual therapy of anti-hypertensives, 25.94% of patients are prescribed with three drug anti-hypertensive therapy and 11.95% of patients are prescribed with four drug anti-hypertensive therapy.
Table : 20 List and percentage of Medication Adherence in CKD patients

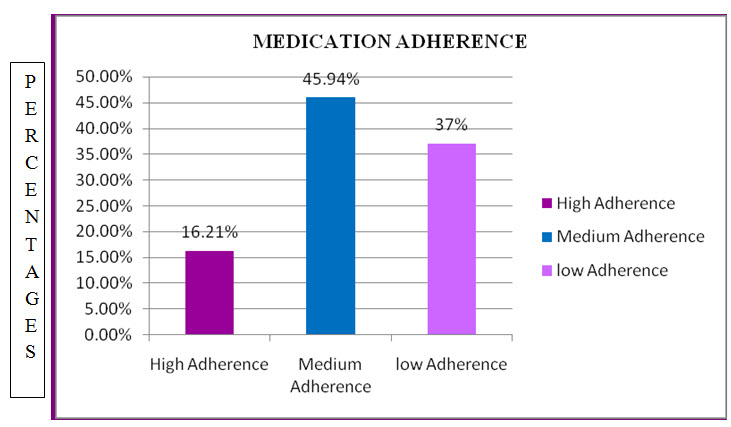
Figure :18 Column presentation for percentage of Medication adherence Among study population the medication adherence have been done .In which patients with High Adherence are with percentage of 16.21%,Medium Adherence are with percentage of 45.94%, Low Adherence are with percentage of 37%.
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT editor-in-chief@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
DISCUSSION
Our study tried to find utilization of various antihypertensive drugs in chronic kidney disease patients and awareness about hypertension.
The age groups between 18-90 years were admitted during the period of study. The age group between 79-88 years were found to be 9.70% whereas in the study conducted previously only below 78 years of age were admitted during their period of study (Neethu Joseph et al., 2017). The majority of patients were between 59-68 years of age group (33.69%). There is a significant difference between the different age groups.
The sex wise distribution resulted that majority of the patients were of male sex which was as high as 72.80%. The females accounted for around 27.10%. Whereas in the study conducted previously males where more prevalent 69 (69%) and 31 (31%) females (Neethu Joseph et al., 2017). This only confirmed the finding of the previous study conducted that males accounted for the majority of the disease burden.
The alcoholic status distribution resulted that majority of the patients were alcoholic which was as high as 56%. The non-alcoholics accounted for around 44%.There is not much significant difference between alcoholics and non-alcoholics.
Yacoub R et al., conducted a cross sectional study on Association between smoking and Chronic Kidney Disease and concluded that Smoking significantly increases the risk of CKD when compared to nonsmokers (Arshad H. Mohd et al., 2012). The smoking status distribution added to the evidence of the previous study that the impact of smoking is directly related to the worsening of the CKD. In present study, the smokers accounted for around 60% and non-smokers accounted for 40% making smoking as a potential risk hazard for CKD patients.
In the present study the percentage of co-morbid condition in CKD Patients were Hypertension (100%), Anemia (43.24%), Diabetics mellitus (62.70%), Hypothyroidism (9.72%), Bronchial Asthma (4.87%). In the previous study the percentage of comorbid condition are Hypertension (66.66%), CKD (100%), cardiac disease (83.33%), foot ulcer (8.3%), cellulitis (14.16%), neurological disorders (10.83%) and anemia (22.5%) (Bhanu Priya B. Basavanna P L, 2015).
Hypertension (HTN) and CKD is cyclic in nature and has been found to occur in 85% to 95% of patients with CKD (stages III–V) (Rajiv Ahlawat et al., 2012). In the present study according to The Kidney Disease Outcomes Quality Initiative (KDOQI) mostly seen Stage in CKD was Stage-V (56%), Stage-III (17%), Stage-II (14%), Stage-IV (11%), followed by Stage-I (02%).
The target blood pressure in CKD patients should be maintained below 140/90 mmHg. High systolic pressure increases the myocardial work, while low diastolic pressure reduces myocardial circulation and increases the myocardial ischemia leading to cardiovascular morbidity and mortality Control of hypertension in CKD patients was difficult to bring under control. More than two-third of the patients (66%) had BP >140/90 mmHg. About one-third of the patients (34%) had BP control <140/90 mmHg. Intensive BP control was present in around one-tenth of total patients (11%) (Al-Ramahi R, 2012). In present study patients were having 33% of BP >140/90 and 57% of BP<140/90 and intensive BP control was around 9.20%.
In the present study the most commonly prescribed anti-hypertensives were found to be CCBs 64.13%, Diuretics 57.60%, Beta blockers 43.47%, α blockers 26%,α+β blockers 8.69%, Angiotensin receptor blockers 11.40%, Angiotensin converting enzymes inhibitors 1%, Central Sympatholytics 22.80%, vasodilators 1.60%. Bhanu Priya B et al., conducted a study on Pattern of antihypertensive drug utilization among chronic kidney disease, among the patients, most commonly prescribed was CCBs (39.5%), followed by diuretics (25.12%) (Arshad H. Mohd et al., 2012).
Calcium channel blockers cause vascular smooth muscle relaxation, especially in arterial beds and produce negative inotropic and chronotropic effects (Bhanu Priya B. Basavanna P L, 2015). In the present study most commonly used calcium channel blockers are Amlodipine with percentage of 52%, and Cilindipine with percentage of 9.10%.
Cilnidipine though has its longer duration of action of 24 hours, also prevents reflex tachycardia as it selectively acts on both L and N type of calcium channels, still Amlodipine (L type of calcium channel blocker) was prescribed because of free supply by the Government of the State (Neethu Joseph et al.,2017).
Diuretics act primarily by increasing sodium excretion and decrease the blood pressure and also by facilitating the response of other antihypertensive agents in CKD.
Thiazide and loop diuretics increase the delivery of sodium to the distal tubule, thereby increasing urinary potassium excretion. So, potassium-sparing diuretics are generally used as an adjunct to other diuretics for prevention and treatment of diuretic induced hypokalemia and in patients with edematous states.
In present study most commonly used Diuretics are Furosemide with percentage of 36.90% and Toresemide 11.40%.
Beta blocker is preferred in hemodialysis patients due to over activity of renin-angiotensin-aldosterone system, increased levels of sympathetic activity in hemodialysis patients. Beta blockers have been suggested to be cardio protective in hemodialysis patients (Neethu Joseph et al., 2017).
In present study most commonly used Adrenergic Antagonist are β Blockers are Metoprolol with percentage of 31.50%, In α blockers are prazosin with percentage of 26%, In α+β blocker are Carvedilol with percentage of 8.60%.
Increased glomerular capillary pressure induces glomerular injury, and ACE inhibitors reduce this parameter both by decreasing arterial blood pressure and by dilating renal efferent arterioles (Bhanu Priya B. Basavanna P L, 2015).
ARBs act by expressing insurmountable antagonism due to slow dissociation kinetics of the compounds from the AT1 receptor.
In present study most commonly used ARB’s are Telmisartan with percentage of 6.50%, and ACE’s are Ramipril with percentage of 1%.
Centrally acting antihypertensives lowers BP without compromising the renal blood flow or glomerular filtration rate (Arshad H. Mohd et al 2012).
In present study most commonly used central sympatholytics are Clonidine with percentage of 18.40%, Vasodilators are Minoxidil with percentage of 1%.
In present study most commonly used Antihypertensive combinations are Amlodipine + metoprolol with percentage of 6.50%, and Furosemide+Eplerenone with percentage of 1.60%.
The combination of this drug provides added advantage because of different drugs have a different mechanism of action for reduction in blood pressure.
In previous study Most commonly prescribed combinations were (50%) hydrochlorothiazide+enalapril, follow by torsemide+enalapril1 (25%) were the most commonly prescribed two-drug combination therapy in patients (Bhanu Priya B. Basavanna P L, 2015).
In present study mostly used therapys are 8.15% of patients are prescribed with monotherapy of antihypertensives, 34.87% of patients are prescribed with dual therapy of anti-hypertensives, 25.94% of patients are prescribed with three drug anti-hypertensive therapy and 11.95% of patients are prescribed with four drug anti-hypertensive therapy. In previous study Most of the CKD patients with HTN were treated with Multi drug therapy. 59.2% of patients were taking multitherapy and 40.8% of patients were taking monotherapy (Ajay Kumar Lal Das, 2015).
In present study medication adherence have been done .In which patients with High Adherence are with percentage of 16.21%, Medium Adherence are with percentage of 45.94%, Low Adherence are with percentage of 37%. Burnier M et al. conducted a large survey of quantitative studies on Drug adherence in chronic kidney diseases and dialysis. And the review concluded that because of the complexity of treatment and the high pill burden, CKD patients are at very high risk of poor adherence and should definitively be supported in their efforts to maintain a good persistence.
CONCLUSION
In our present study, we performed a randomized, prospective and observational study on patient cohorts in Gleneagles Global Hospital to evaluate the drug utilization pattern of antihypertensive therapy in hypertensive patients with CKD.
The observational study was conducted in 184 patients to evaluate the drug utilization pattern of anti-hypertensive therapy in hypertensive patients with CKD. All patients in the study population have hypertension.
• Amlodipine belonging to the class of calcium channel blocker was found to be the most commonly prescribed anti-hypertensive drug when compared with other antihypertensive modalities in hypertensive patients with CKD.
• Furosemide belonging to the class of diuretics was found to be the second most commonly prescribed anti-hypertensive drug in hypertensive patients with CKD.
• Metoprolol belonging to the class of β-blockers was found to be the third most commonly used anti-hypertensive drug in hypertensive patients with CKD.
• Most of the patients found to have more than two comorbidity conditions. • Most of the patients were in stage-5 of CKD.
• Most of the patients found to be in stage-1 hypertension.
• Amlodipine + Metoprolol which are the combination of anti-hypertensive drugs belonging to CCB’s and β blockers classes respectively were found to be the most commonly prescribed combination in hypertensive patients with CKD.
• Two drug anti-hypertensive therapy is most commonly found in hypertensive patients with CKD.
• High medication adherence was found in the observed population which is calculated based upon morisky medication adherence scale.
Thus from our study we have concluded that the CCB’s, diuretics and β-blockers are the most commonly used anti-hypertensive classes in hypertensive patients with CKD. Use of anti-hypertensives in CKD patients does not deviate from the guidelines laid down by NKF KDOQI guidelines. The patients should be educated about the rational use of drugs to decrease medication adherence.
REFERENCES
1. Abhisek PA., Panda R., Mohapatra J., et al., (2016); Antihypertensive drug utilisation pattern among chronic kidney disease patients undergoing maintenance dialysis in a tertiary care teaching hospital; J. Evolution Med. Dent. Sci; 5(50); 3207-3211.
2. Ajay Kumar Lal Das (2015); A Study on Prescribing Pattern of Antihypertensive drugs in Diabetic patients at a tertiary care teaching hospital; Int J Med Res Prof; 1(3); 118-121.
3. Al-Ramahi R (2012); Medication prescribing patterns among chronic kidney disease patients in a hospital in Malaysia; 23(2); 403-408.
4. Andrew S. Levey., Rocco MV, Anderson S, et al., (2004); K/DOQI clinical practice guidelines on hypertension and antihypertensive agents in chronic kidney disease; American Journal of Kidney Diseases; 43(5); S1–S290.
5. Anju Madhwar., Dharmender Gupta., Sujata Singh., N. A. Ansari (2015); Drug Utilization Evaluation of Antihypertensive agents in nephrology department in tertiary care hospital; Indian Journal of Pharmacy and Pharmacology; 2(1); 10-15.
6. Arshad H. Mohd., Uday V. Mateti., Venkateswarlu Konuru., Mihir Y. Parmar. and Buchi R. Kunduru (2012); A study on prescribing patterns of anti hypertensives in geriatric patients; 3(4); 139-142.
7. Barbara G. Wells., Joseph T. Dipiro., Terry L. Schwinghammer. and Cecily V. DiPiro (2015), “Chronic Kidney Disease”, in Vimal K. Derebail, Abhijit V. Kshirsagar, and Melanie S. Joy, Handbook of Pharmacotherapy-A Pathophysiologic Approach, McGraw-Hill, New York, pp. 787 & pp. 798.
8. Bhanu Priya B. and Basavanna P L (2015); Pattern of antihypertensive drug utilisation among chronic kidney disease patients in a dialysis unit of a tertiary care hospital; International Journal of Biomedical Research; 6(4); 251-254.
9. British Kidney Patient Association (2006); Treatment of Hypertension in Chronic Kidney Disease.
10. Centers for Disease Control and Prevention (2018); Chronic Kidney Disease Surveillance System-United States. GA 30329-4027.
11. Chang A, Kramer H (2012); CKD progression: a risky business. Nephrol Dial Transplant; 27(7); 2607-2609.
12. Elahe Elhami (2015); Drug Utilization Evaluation Of Antihypertensive Drugs In Patients With Renal Failure; World Journal Of Pharmacy And Pharmaceutical Sciences; 5(1); 572-582.
13. Falodia J. and Singla MK (2012); CKD Epidemiology and Risk Factors; Clin Queries Nephrol; 20(1); 249–252.
14. Horowitz B., Miskulin D. and Zager P (2015); Epidemiology of Hypertension in CKD; Adv Chronic Kidney Dis.; 22(2); 88-95.
15. Iseki K (2005); Factors Influencing the Development of End Stage Renal Disease; Clin Exp Nephrol; 9(1); 5-14.
16. James L. and Holly MD (2013); Southeast Texas Medical Associates, LLP; Chronic-Renal-Disease Disease-Management.
17. Joseph T. Dipiro., Robert L. Talbert., Gary C. Yee., Gary R. Matzke., Barbara G. Wells. L. Michael Posey (2011); Chronic Kidney Disease; in Vimal K. Derebail, Abhijit V. Kshirsagar, and Melanie S. Joy, Text book of Pharmacotherapy-A pathophysiologic approach, McGraw-Hill, New York, pp. 775-796
18. Kasper., Braunwald., Fauci., Hauser., Longo. Jameson (2008), “Chronic Kidney Disease”, In; Dennis L. Kasper, Harrison Principles of Internal Medicine, McGraw Hill, New York, pp. 1682 & pp. 1685
19. Kidney Disease (2013); Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease; Kidney Int Suppl; 3; 1-150.
20. Kwakernaak AJ., Zelle DM., Bakker SJ. and Navis G (2013); Central body fat distribution associates with unfavorable renal hemodynamics independent of body mass index; J Am Soc Nephrol; 24(6); 987–994.
21. Lea JP. and Nicholas SB (2002); Diabetes mellitus and hypertension: key risk factors for kidney disease; J Natl Med Assoc; 94(8 Suppl); 7S-15S.
22. Mackenzie HS., Lawler EV. and Brenner BM (1999); Congenital Oligonephropathy: The Fatal Flaw in Essential Hypertension; Kidney Int Suppl; 55(1); S30-S34.
23. Mary Anne Koda-Kimble., Lloyd Yee Young., Brian K. Alldredge., Robin L. Corelli., B. Joseph Guglielmo., Wayne A. Kradjan. and Bradley R. Williams (2008), “Chronic Kidney Disease”, in Amy Barton Pai and Todd A. Conner, Textbook of Applied Therapeutics-The Clinical Use of Drugs, Lippincott Williams & Wilkins, Maryland, USA, pp. 31-1 to 31-10
24. McClellan WM. and Flanders WD (2003); Risk factors for progressive chronic kidney disease; J Am Soc Nephrol; 14(7 Suppl 2); S65-70.
25. Miller JA., Anacta LA. and Cattran DC (1999); Impact of Gender on Renal Response to Angiotensin II; Kidney Int; 55(1); 278-285.
26. Mirrakhimov AE (2012); Obstructive Sleep Apnea and Kidney Disease: is there any direct link?; Sleep Breath; 16(4); 1009-1016.
27. Myers GL., Miller WG., Coresh J., Fleming J., Greenberg N., Greene T. and National Kidney Disease Education Program Laboratory Working Group (2006); Recommendations for improving serum creatinine measurement: a report from the Laboratory Working Group of the National Kidney Disease Education Program; Clin Chem; 52; 5-18.
28. National Kidney Foundation. KDOQI Clinical Practice Guideline for Diabetes and CKD (2012); The National Kidney Foundation’s Kidney Disease Outcomes Quality Initiative (KDOQI) updated recommendations for treating patients with diabetes and CKD because of recent evidence changing previous recommendations; Am J Kidney Dis; 60(5); 850-886.
29. National Kidney Foundation-Hypertension: key risk factor for Chronic kidney disease. National Kidney Foundation's Kidney Disease Outcomes Quality Initiative (NKFKDOQI).
30. Neethu Joseph., Dr Yogananda R., Dr. Bharathi DR., Varsha Padman. Dr. Sandeep (2017); A Study on Prescription Pattern of Antihypertensive Agents in Chronic Renal Failure Patients and Assessment of Medication Adherence; Int. J. Pharm. Sci. Rev. Res; 45(2); 72-75.
31. Neugarten J. and Golestaneh L (2013); Gender and The Prevalence and Progression of Renal Disease; Adv Chronic Kidney D; 20(5); 390-395.
32. Noah Jarari., Narasinga Rao., Jagannadha Rao Peela., Khaled A. Ellafi., Srikumar Shakila., Abdul R. Said., Nagaraja Kumari Nelapalli., Yupa Min., Kin Darli Tun., Syed Ibrahim Jamallulail., Avinash Kousik Rawal., Ranjani Ramanujam., Ramesh Naidu Yedla., DhiliKumar Kandregula., Anuradha Argi. and Laxmi Teja Peela (2016); A review on prescribing patterns of antihypertensive drugs; Clin Hypertens; 22; 7
33. Peralta CA., Hicks LS., Chertow GM., Ayanian JZ., Vittinghoff E., Lin F. Shlipak MG (2005); Control of Hypertension in Adults With Chronic Kidney Disease in the United States; Hypertension; 45(6); 1119-1124.
34. Rajiv Ahlawat., Sanjay D’cruz. and Pramil Tiwari (2012); Drug Utilization Evaluation of Antihypertensive agents in nephrology department in tertiary care hospital; 3(1); 1000149
35. Ratcliffe PJ (1993); Molecular biology of erythropoietin; Kidney Int; 44(6); 887–904.
36. Ridao N., Luño J., García de Vinuesa S., Gómez F., Tejedor A. and Valderrábano F (2001); Prevalence of Hypertension in Renal Disease; Nephrol Dial Transplant; 16 Suppl 1; 70-73.
37. Roger Walker. and Cate Whittlesea (2012), “Chronic Kidney Disease and End-Stage Renal Disease”, in J. Marriott, P. Cockwell and S. Stringer, Textbook of Clinical Pharmacy and Therapeutics, Churchill Livingstone, Edinburgh, pp. 274-284
38. Shah J. Balraj A (2017); Drug utilization pattern of antihypertensive agents in patients of hypertensive nephropathy in a tertiary care hospital: a cross sectional study; Int J Basic Clin Pharmacol; 6(9); 2131-2133.
39. Silbiger S. and Neugarten J (2013); Gender and Human Chronic Renal Disease; Gend Med. 5; Suppl A; S3-S10.
40. Song EY., McClellan WM., Mc Clellan A., Gadi R., Hadley A.C., Krisher J., Clay M. and Freedman B.I (2013); Effect of community characteristics on familial clustering of end-stage renal disease; Am J Nephrolxpp; 30(6); 499-504.
41. Soumya Santra., Divya Agrawal., Sanjay Kumar., Sudhanshu Sekhar Mishra (2015); A Study on the Drug Utilization Pattern in Patients with Chronic Kidney Disease with Emphasis on Antibiotics; 2; 85-89.
42. Stevens LA., Coresh J., Greene T. and Levey AS (2015); Assessing kidney function-measured and estimated glomerular filtration rate; N Engl J Med; 354; 2473-83.
43. The UMHS Clinical Guideline on Chronic Kidney Disease (2013); Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease.
44. Toto RD (2005); Treatment of Hypertension in Chronic Kidney Disease; Semin Nephrol; 25(6); 435-439.
45. Vikse BE., Irgens LM., Leivestad T., Hallan S. and Iversen BM (2008); Low Birth Weight Increases Risk for End-Stage Renal Disease; J Am Soc Nephrol; 19(1); 151-157.
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT editor-in-chief@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE









