{ DOWNLOAD AS PDF }
 ABOUT AUHTOR
ABOUT AUHTOR
*A. Bharath kumar, T. Mubeena, Y. Charitha
Annamacharya college of Pharmacy
Rajampet, Andhra pradesh, India
*abharatpharma@gmail.com
ABSTRACT:
Diabetic neuropathy is a debilitating disorder that occurs in of Patients with diabetes. The primary types of diabetic neuropathy are sensorimotor and autonomic. Patients may present with one type of diabetic neuropathy or may develop combinations of neuropathies when its severity was more. Diabetes is metabolic disorder which causes the abnormal elevations of blood glucose levels in the body. The diabetic neuropathy was neurological affecting disorder. Diabetic neuropathies are a family of nerve disorders caused by diabetes. People with diabetes can, over time, develop nerve damage throughout the body. The symptoms such as pain, tingling, or numbness and loss of feeling in the hands, arms, feet, and legs. About 60 to 70 percent of people with diabetes have some form of neuropathy.The diabetes people develop nerve problems at any time, but risk rises with age and longer duration of diabetes. Regular monitoring blood sugar levels normal levels and foot care practices we can Prevent the diabetic neuropathy complications in the community.
[adsense:336x280:8701650588]
REFERENCE ID: PHARMATUTOR-ART-2479
|
PharmaTutor (ISSN: 2347 - 7881) Volume 5, Issue 3 Received On: 31/10/2016; Accepted On: 08/12/2016; Published On: 01/03/2017 How to cite this article: Kumar AB, Mubeena T, Charitha Y;A Review on Prevention and Management of Diabetic Neuropathy; PharmaTutor; 2017; 5(3); 15-20 |
INTRODUCTION
Diabetic neuropathies are nerve damaging disorders associated with diabetes mellitus.These conditions are thought to result from diabetic microvascular injury involving small blood vessels that supply nerves (vasa nervorum) in addition to macrovascular conditions that can culminate in diabetic neuropathy. Peripheral Diabetic Neuropathy (PDN), the most common complication of diabetes, is defined as a symmetrical, lengthdependent distal sensorimotor polyneuropathy, a consequence of metabolic and microvascular alterations[1].
Causes of peripheral neuropathy
• Alcoholism. Poor dietary choices made by person consuming the alcoholic products can lead to cause the vitamin deficiencies.
• Autoimmune diseases. These include Sjogren's syndrome, lupus, rheumatoid arthritis, Guillain-Barre syndrome, chronic inflammatory demyelinating polyneuropathy and necrotizing vasculitis cause the neuropathic complicaations
• Diabetes : person with diabetes it may affects the neuronal functions.
• Exposure to poisons : Toxic substances include heavy metals or chemicals.
• Medications. cancer medications that can cause peripheral neuropathy.
• Infections : These include certain viral or bacterial infections, including Lyme disease, shingles, Epstein-Barr virus, hepatitis C, leprosy, diphtheria and HIV.
• Inherited disorders : Disorders such as Charcot-Marie-Tooth disease are hereditary types of neuropathy.
• Trauma or pressure on the nerve : Traumas,such as from motor vehicle accidents, falls or sports injuries, can sever or damage peripheral nerves.
• Tumors : Growths, cancerous (malignant) and noncancerous (benign), can develop on the nerves or press nerves.
• Vitamin deficiencies : B vitamins — including B-1, B-6 and B-12 — vitamin E and niacin are crucial to nerve health.
• Bone marrow disorders :These include abnormal protein in the blood(monoclonal gammopathies), a form of bone cancer (osteosclerotic myeloma), lymphoma and amyloidosis.
• Other diseases. These include kidney disease, liver disease, connective tissue disorders.
Classification of diabetic neuropathy
• "Hyperglycemic neuropathy"
• Symmetric polyneuropathy
• Sensory/autonomic polyneuropathy
• Acute painful diabetic neuropathy
• Focal and multifocal neuropathy Cranial neuropathy
• Thoraco-abdominal neuropathy
• Focal limb neuropathies
• Diabetic amyotrophy Mixed forms
• Symmetric polyneuropathies
• Chronic sensory or sensorimotor
• Autonomic Symmetric,
• lower limb,
• motor Focal
• multifocal neuropathies
Diagnosis of diabetic peripheral neuroapthy
• The diagnosing diabetic peripheral neuropathy the physician typically assesses the appearance of the feet, presence of ulceration, and ankle reflexes.The most useful physical examination findings for large fiber neuropathy are an abnormally decreased vibration perception to a 128-Hz tuning fork (likelihood ratio (LR) range, 16–35) or pressure sensation with a 5.07 Semmes-Weinstein monofilament (LR range, 11–16)[2].
Physical examination
• Vital signs and pain index
• Supine and standing blood pressure for postural hypotension
• Cardiovascular examination to look for arrhythmias, absent or diminished pulses, edema, or delayed capillary refilling
• Cutaneous examination to look for extremity hair loss, skin or nail changes (including callus), and pretrophic (red) areas, especially between toes
• Neurologic examination using the 5.07 Semmes-Weinstein (10-g) nylon filament test (10-g monofilament test)
• Inspection of feet for asymmetry, loss of arch height, or hammer toes
Epidemology
• Globally diabetic neuropathy affects approximately 132 million people as of 2010 (1.9% of the population).
• Diabetes is the leading known cause of neuropathy in developed countries, and neuropathy is the most common complication and greatest source of morbidity and mortality in diabetes patients.It is estimated that the prevalence of neuropathy in diabetes patients is approximately 20%.
Signs and Symptoms
The differential diagnosis of diabetic nephropathy is vast, but it includes the following in a patient with known diabetes mellitus:
• Primary or secondary glomerular disease
• Nephrosclerosis
• Renovascular hypertension
• Renal artery stenosis
• Renal vein thrombosis
• Multiple myeloma
• Cholesterol embolization
• Chronic obstruction
• Interstitial nephritis
• Amyloidosis
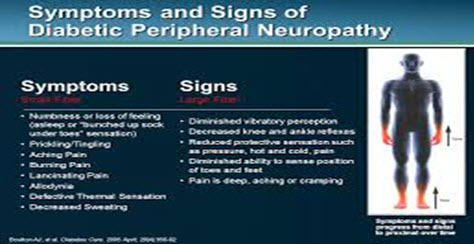
Fig 1:symptoms of diabetic peripheral neuropathy
Neuropathy Affecting Nerve parts in the body
Peripheral neuropathy affecting sites
• toes
• feet
• legs
• hands
• arms
Autonomic neuropathy affecting sites
• heart and blood vessels
• digestive system
• urinary tract
• sex organs
• sweat glands
• eyes
• lungs
Proximal neuropathy affecting sites
• thighs
• hips
• buttocks
• legs
Focal neuropathy affecting sites
• eyes
• facial muscles
• ears
• pelvis and lower back
• chest
• abdomen
• thighs, legs,feet
Pathophysiology of diabetic peripheral neuropathy
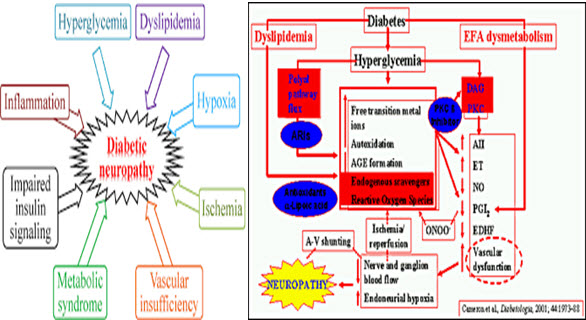
Fig 2: Pathophysiology of diabetic peripheral neuropathy
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT editor-in-chief@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
Prevention of diabetic Peripheral neuropathy:
It includes strict optimization of blood sugar levels, cessation of smoking and alcohol intake, control of hyperlipidemia and hypertension. It has been seen that daily intake of antioxidantsnutritional foods dietary fibers have a role in the prevention of peripheral neuropathy[3].
Simple measures like heat, ice, massage, manipulative therapies (e.g. chiropractic, osteopathy), physiotherapy
Treating the primary cause- e.g. improve diabetic control; supplement thiamine; reduce/stop alcohol consumption. Treating the primary cause includes interventional techniques such as surgery for disc prolapses or spinal stenosis; or nerve translocation surgery (e.g. carpal tunnel release)
Stimulating inhibitory mechanisms in the periphery or in the spinal cord: e.g. acupuncture TENS,electrical peripheral nerve or dorsal column or central (deep-brain) stimulation.[3]
Inhibition or prevention of ascending nerve transmission in the peripheral nervous system, in the dorsal root ganglion or spinal cord: e.g. nerve blocks, neurolysis or rhyzolysis
Alter pain processing at the cortical level, e.g. cognitive therapies, biofeedback, hypnosis, meditation. It is currently unclear the exact way in shich these therapies alter sensation, but is assumed to involved both descending inhibition and alteration of sensitivity to ascending stimulus.
Physiotherapy
Physiotherapists are an essential part of the multidisciplinary team, and invaluable aid to patients with neuropathic pain. They can challenge beliefs about pain and damage, pain and movement and promote normal movement and discourage pain behaviours such as fear-avoidance of movement[4].
Acupuncture
Acupuncture is the practice of treating illness by the placement of needles into specific points along “meridian” lines. It is an essential part of the treatment plan in traditional Chinese medicine.
Acupuncture is recommended by NICE for the treatment of uncomplicated low back pain in primary care in the first 12 months
Transcutaneous Electrical Nerve Stimulation (TENS)
Transcutaneous electrical nerve stimulation (TENS) is a non-invasive treatment modality developed Dr Norman Shealy in the 1960s. The principle by which TENS is thought to work is that stimulation of the Abnerve fibres causes interference with and temporary interruption to pain transmission in the c-fibres and Adfibres at the dorsal horn and spinal levels.
The TENS unit is a small box containing a battery-operated pulse-generator, the frequency and intensity of which can be controlled by the user. The pulses are then transmitted to the user’s skin via adhesive electrode pads[5].
Nerve Blocks and Neurolysis
If a single nerve or nerve root can be found which is responsible for the patient’s pain, a nerve block may be considered. The purpose of nerve blocks is to temporarily (or permanently) interrupt nerve transmission and relieve pain- thereby allowing the patient to move more normally.
Spinal Cord Stimulation (SCS) :It is an invasive treatment for chronic pain based on electrical stimulation of the dorsal columns of the spinal cord. Mechanisms being not known, believed to involve spinal and supraspinal effects. It is a proven effective therapy for various types of mixed neuropathic conditions but the effectiveness of SCS treatment for PDN is not well established.
Other physical therapy modalities include pain modulators like hot and cold packs, ultrasound, short wave diathermy, low-frequency currents (diadynamic currents, interferential currents) and techniques like high voltage galvanic stimulation[6].
Ultrasound and short wave diathermy: Ultrasound and short wave diathermy which are deep heating agents like are not recommended in the treatment of neuropathic pain.
They are helpful especially in joint contractures, and adhesions. It increases the flexibility of collagen fibers and circulation of connective tissues which help functional restoration. It may provide to decrease neuropathic pain[10].
Massage: Massage is also not recommended. In AIDS patients with neuropathic pain, massage therapy has been applied but there have been no significant changes on pain intensity.
Management of Diabetic Peripheral Neuropathy
|
Pregabalin, 300–600 mg/day Level B |
Venlafaxine, 75–225 mg/day
|
Amitriptyline, 25–100 mg/day
|
|---|---|---|
|
Gabapentin, 900–3600 mg/day |
Dextromethorphan, 400 mg/day Duloxetine, 60–120 mg/day |
Tramadol, 210 mg/day Oxycodone, mean 37 mg/day, max 120 mg/day |
|
Sodium valproate, 500–1200 mg/day |
Morphine sulphate, titrated to 120 mg/day
|
Capsaicin, 0.075% qid
|
Tricyclic antidepressants
TCAs include imipramine, amitriptyline, desipramine and nortriptyline.These drugs are effective at decreasing painful symptoms.
Serotonin-norepinephrine reuptake inhibitors
The SSNRI duloxetine (Cymbalta) is approved for diabetic neuropathy,[12] while venlafaxine is also commonly used.
Selective serotonin reuptake inhibitor
SSRIs include fluoxetine, paroxetine, sertraline and citalopram and are not recommended to treat painful neuropathy because they have been found to be no more efficacious than placebo in several controlled trials[7].
Antiepileptic drugs gabapentin and the related pregabalin, are emerging as first-line treatment for painful neuropathy. Gabapentin compares favorably with amitriptyline in terms of efficacy and is clearly safer.Carbamazepine (Tegretol) is effective but not necessarily safe for diabetic neuropathy. Its first metabolite,oxcarbazepine, is both safe and effective in other neuropathic disorders, but has not been studied in diabetic neuropathy. Topiramate has not been studied in diabetic neuropathy.
Natural remedies.
Vitamin B1,B12 in the Methylcobalamine,high doses of alpha-lipoic acid as well as the amino acid l-arginine which is proven to help with nitric oxide production and subsequent vaso dilation which can help reduce inflammation and associated pain[8].
Analgesics
The patient is treated with Duloxetine + extended release morphine ± naproxen ± hydroxyzine oxycodone ± morphine or hydromorphone.
Photo therapy
Monochromatic infrared photo energy treatment (MIRE) has been shown to be an effective therapy in reducing and often eliminating pain associated with diabetic neuropathy.The studied wavelength of 890nm is able to penetrate into the subcutaneous tissue where it acts upon a specialized part of the cell called the cytochrome C. The infrared light energy prompts the cytochrome C to release nitric oxide into the cells. The nitric oxide in turn promotes vaso dilation which results in increased blood flow that helps nourish damaged nerve cells. Once the nutrient rich blood able to reach the affected areas (typically the feet, lower legs and hands) it promotes the regeneration of nerve tissues and helps reduce inflammation thereby reducing and/or eliminating pain in the area[9].
CONCLUSION
Diabetic neuropathy can affect any part of the nervous system.This nerve disorder should be suspected in all patients with diabetes and in patients.Diabetic neuropathy also can causes the motor deficits and cardiac,endocrine,urinary tract disorders.Strict glycemic control and good daily foot care are key to preventing complications of diabetic neuropathy.Approaching the Pharmacological and non Pharmacological we can prevent the diabetic neuropathy complications.
REFERENCES
1.Greenbaum D: Observations on the homogeneous nature and pathogenesis of diabetic neuropathy. Brain 87:215-232, 1964
2.Thomas PK, Tomlinson DR: Diabetic and hypoglycemic neuropathy. In Peripheral Neuropathy. Dyck PJ, Thomas PK, Griffin JW, Low PA, Poduslo JF, Eds. Philadelphia, W.B. Saunders, 1993, p. 1219-1250.
3. lewelyn JG, Thomas PK, Fonseca V, King RHM, Dandona P: Acute painful diabetic neuropathy precipitated by strict glycaemic control. Acta Neuropathol 72:157-163, 1986.
4. The Diabetes Control and Complications Trial Research Group: The effect of intensive treatment of diabetes on the development and progression of longterm complications in insulin-dependent diabetes mellitus. N Engl J Med 329:977-986,1993.
5. Vinik AI. Diagnosis and management of diabetic neuropathy. Clin Geriatr Med.1999; 15(2): 293-320. 21.Vera Bril. Treatments for diabetic.
6. Thomas PK. Classification, differential diagnosis and staging of diabetic peripheral neuropathy. Diabetes. 1997; 46(Suppl. 2): S54-57.
7.Qutenza (NGX-4010): Full prescribing information. http://www. neurogesx.com/ngx_4010. Accessed January 12, 2010.
8. Sindrup SH, Gram LF, Brøsen K, Eshøj O, Mogensen EF. The selective serotonin reuptake inhibitor paroxetine is effective in the treatment of diabetic neuropathy symptoms. Pain. 1990; 42(2): 135-144.
9. Mary Margaret Huizinga, Amanda Peltier. Painful Diabetic Neuropathy: a management centered review. Clinical Diabetes. 2007; 25: 1.
10. Hamza MA, White PF, Craig WF, Ghoname ES, Ahmed HE, Proctor TJ, et al. Percutaneous electrical nerve stimulation: a novel analgesic therapy for diabetic neuropathic pain. Diabetes Care. 2000; 23(3): 365-370.
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT editor-in-chief@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE









