{ DOWNLOAD AS PDF }
ABOUT AUTHORS
Sabya Sampad Swain, Nadugopal Bhuyan, Chaitanya Prasad Meher
Gayatri institute of science & technology (GIST), Gunupur, Rayagada, Orissa
swainsabhya@gmail.com
ABSTRACT
Rheumatoid arthritis is most common disease in India as well as outside India. The Centers for Disease Control and prevention estimates that more than 40 million Americans have some form of arthritis or chronic joint disorder out of them 7 million Americans suffer from arthritis in its most debilitating forms. Arthritis foundation classified rheumatic diseases as inflammatory disorders affecting more & more individuals than any chronic illness. Osteoarthritis is the most common form of arthritis in the United States, affecting about 12% of Americans between the ages of 25 and 74. Rheumatoid arthritis is thought to affect well over 2 million Americans (two to three times more females more than males), whereas juvenile arthritis affects 71,000 children under 16 years of age, 61,000 of whom are females. The presented article is concern with a brief idea about rheumatoid arthritis.
[adsense:336x280:8701650588]
REFERENCE ID: PHARMATUTOR-ART-2408
|
PharmaTutor (Print-ISSN: 2394 - 6679; e-ISSN: 2347 - 7881) Volume 4, Issue 5 Received On: 16/12/2015; Accepted On: 21/12/2015; Published On: 01/05/2016 How to cite this article: Swain SS, Bhuyan N, Meher CP; A Short Review on Rheumatoid Arthritis (RA); PharmaTutor; 2016; 4(5); 35-40 |
INTRODUCTION
Arthritis: Arthritis is concern with the Inflammation of one or more joints characterized by swelling, warmth, redness of the overlying skin, pain & restriction of motion. Over 200 disease may cause arthritis including rheumatoid arthritis, osteoarthritis, gout, tuberculosis & other infection. Most common types of arthritis are as follows[1].
1. Adult Rheumatoid Arthritis: it’s occurs between 25 and 50 years of age. It’s affects women three times more than men.
2. Juvenile Rheumatoid Arthritis (Still’s Disease): it’s occur before 7 years of age.
3. Osteoarthritis: Second most frequent type of arthritis. This type affects the hyaline cartilage in weight bearing joints. Usually occurs because of destruction of bone coverings at the joints due to repeated use or trauma.
4. Ankylosing Spondylitis: Most prevalent in males with the age of onset ranging from 20 to 40 years of age. It’s affects the axial skeleton and large peripheral joints of the body. Common symptoms include recurrent back pain and early morning stiffness.
Rheumatoid Arthritis
It is the second most common form of arthritis after osteoarthritis. Rheumatoid arthritis is a common autoimmune disease that is associated with progressive disability, systemic complications, early death, and socioeconomic costs. it (RA) is an inflammatory disease that exerts its greatest impact on those joints of the body that are lined with synovium, a specialized tissue responsible for maintaining the nutrition and lubrication of the joint. The distribution of joints affected (synovial joints) is characteristic. It typically affects the small joints of the hands and the feet, and usually both sides equally in a symmetrical distribution, though any synovial joint can be affected. In patients with established and aggressive disease, most joints will be affected over time [2]. As it progresses the ligaments supporting the joints are damaged & there is erosion of the bone, leading to deformity of the joints. Tendon sheaths can be affected, leading to tendon rupture, onset can be any age, & there is considerable range of severity. Women are at greater risk.
CHARACTERISTICS :
Rheumatoid arthritis is characterized by
• Synovial inflammation and hyperplasia (“swelling”)
• Autoantibody production (rheumatoid factor and anti–citrullinated protein antibody [ACPA])
• Cartilage and bone destruction (“deformity”)
• Cardiovascular, pulmonary, psychological, and skeletal disorders.
Morphology
Joints : RA causes a broad spectrum of morphological alteration. The more severe are manifested in the joints. Initially the synovium becomes grossly edematous thickened & hyperplastic transferring it’s smooth contour to one covered by delicate & bulbous fronds. The characteristic histologic feature includes
• Infiltration of synovial stroma by dense perivascular inflammatory cells consisting of B-cells, CD4 + T cell, plasma cells, macrophages
• Increase vascularity owing to vasodilation & angiogenesis with superficial hemosiderin deposit.
• Aggregation of organizing fibrin covering portion of the synovium & floating in the joint space.
• Accumulation of neutrophils in the synovial fluid but not deep in the synovial stroma
• Osteoclastic activity in underlying bone allowing the synovium to penetrate into the bone forming juxtra articular erosions,subchondral cysts & osteoporosis & pannus formation. Which growth over the articular cartilage causes it’s erosion
[adsense:468x15:2204050025]
PATHOPHYSIOLOGY

The presence of an infectious agent such as mycoplasma, Epstein borr virus (EBV), cytomegalvo virus (CMV) or rubella virus either locally in the synovial fluid or systemic infection some time prior to the attack of rheumatoid arthritis. The proposed event in immunopathogenesis of RA consist of following sequences
In response to antigenic response in a genetically predisposed individual (HLA-DR) CD4 + T cell are activated . the cells elaborate cytokines the important ones being tumor necrosis factor (TNF)-α , interferon-Y & interleukin-1. These cytokines activate endothelial cells B lymphocytes & macrophages. Activation of B-cells releases IgM antibody against IgG (i.e. anti IgG) this molecule is termed as rheumatoid factor (RF). IgG &IgM immune complexes trigger inflammatory damage to the synovium, small blood vessel & collagen. Activated endothelial cells express adhesion molecules which stimulates collection of inflammatory cells. Activation of macrophages releases more cytokines which cause damage to joint tissue & vascularization of cartilage called pannus formation. Eventually damage & destruction of bone & cartilage are followed by fibrosis & ankylosis producing joint deformities.
FACTORS ASSOCIATED FOR PATHOGENESIS OF RA[3]
• Cigarette smoking.
• Tumor necrosis factor (TNF)-a activity.
• Abnormal and inappropriate B-lymphocyte activity, i.e. abnormal antibody production.
• Detection of circulating autoantibodies against IgFc, these autoantibodies have been termed ‘rheumatoid factor’, and they may be involved in the inappropriate presentation of antigens to T cells by B cells.
• Abnormal activity of certain signaling pathways in synovial tissue, e.g. the Wnt signaling pathway, which is involved in embryonic development and cell renewal. In patients with RA, it has been reported that the synovial cells have abnormally high activity of the Wnt gene, as well as a number of other genes for several of the cytokines, cell adhesion molecules and chemokine’s.
Diagnosis of rheumatoid arthritis can be done by detection of serum RF, morning stiffness for 1 hour or longer for 6 weeks or more , arthritis in three or more joints persisting for 6 weeks or more, persistence for 6 weeks or more of symmetrical arthritis , persistence for 6 weeks or more of arthritis of the hand joints, rheumatoid nodules, observation, using hand radiographs, of changes, erosion or unequivocal bony decalcification.
PHARMACOTHERAPY OF RHEUMATOID ARTHRITIS [4,5]
The goals of drug therapy in RA are: Ameliorate pain, swelling and joint stiffness , Prevent articular cartilage damage and bony erosions , Prevent deformity and preserve joint function. NSAIDs are the first line drugs and afford symptomatic relief in pain,swelling, morning stiffness, immobility, but do not arrest the disease process. Though mild/early cases are still mostly treated only with NSAIDs, the current recommendation is to add DMARDs as soon as the diagnosis of RA is confirmed.
1. Anti-inflammatory analgesics (aspirin & other NSAID) :

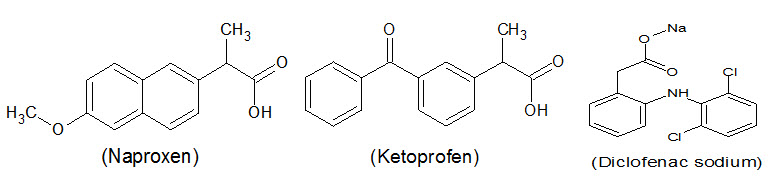
These drugs act symptomatically , relives pain, decrease the swelling & help the joint movement. This facilitates the practicing of exercises design to promote the maintenance of function & the prevention of deformities. No NSAID is consistently more effective than any other. But some patient may not tolerate a particular drug. Aspirin still remains a useful drug & in high dose it is as effective as any other NSAID , but causes GI adverse reaction especially in elderly patient. It is usually given in the dose of 3-5 gm daily to maintain therapeutic blood levels of 20-30 mg. enteric coated aspirin causes less gastric irritation & may be preffered. Aspirin & indomethacin can may be given as rectal suppositories so as to avoid gastric irritation. Other NSAID that may be used are diclofenac 75-100 mg twice daily, naproxen 250 mg twice daily, ketoprofen 50 mg thrice daily given with food, a single dose of naproxen 500mg taken at bed time may also effective. Patient who are not able to tolerate the above drugs may be prescribed a COX-2 inhibitor.
2. Glucocorticoids : They have potent immunosuppressant and antiinflammatory activity: can be inducted almost at any stage in RA along with first or second line drugs, if potent antiinflammatory action is required while continuing the NSAID ± DMARD. Symptomatic relief is prompt, but they do not arrest the rheumatoid process, though joint destruction may be slowed and bony erosions delayed. Long-term use of corticosteroids carries serious disadvantages. Prednisolone is used in the dose of 1mg/kg/day. Low dose of prednisolone (5-10mg/day) may be especially useful in pregnant & elderly patient as an alternative to DMARD.

NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT editor-in-chief@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE
Disease modifying antirheumatic drugs (DMARDs) :
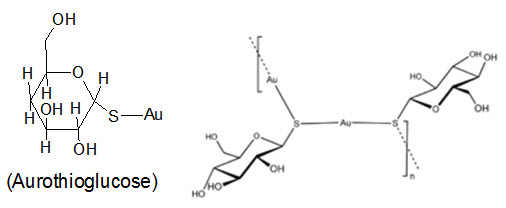
Gold salts :Gold is considered to be the most effective agent for arresting the rheumatoid process and preventing involvement of additional joints. Water soluble gold preparation like sodium aurothiomalate, aurothiosulphate & aurthioglucose have been shown to produce some beneficial effect in RA. Gold salt can cause various toxic manifestation effect such as dermatitis, nephropathy, oral ulceration, bone marrow depression & liver damage. This toxicity is treated with prednisolone (10-20 mg daily)dimercaprol & the chelating agent d-penicillamine. Gold is heavily bound to plasma and tissue proteins, especially in kidney : stays in the body for years. It is rarely used now.
Auranofin: It is an orally active gold compound containing 29% gold, with a bioavailability of 25%. Plasma gold levels and efficacy are lower than with injected gold sod. thiomalate, but it is less toxic. Main adverse effect is diarrhoea (30% incidence) and abdominal cramps. Others are pruritus, taste disturbances, mild anaemia and alopecia. Auranofin is used infrequently. Dose: 6 mg/day in 1 or 2 dose.

Chloroquine and hydroxychloroquine : It have been shown toproduce moderatebenefit in RA. These are antimalarial drugs found to induce remission in upto 50% patients of RA, but take 3–6 months. Their advantage is relatively low toxicity, but efficacy is also low; bony erosions are not prevented.

d-penicillamine :This is a copper containing chelating agent with a gold-like action in RA, but less efficacious; bony erosions do not heal.it causes selectively reduces the serum levels of certain immunoglobulins It is not favoured now because it does not offer any advantage in terms of toxicity, which is similar to that of gold. Loss of taste, systemic lupus and myasthenia gravis are the other adverse effects.it started in the dose of 125 mg daily. Paradoxically penicillamine sometimes induces a multiple of autoimmune syndromes involving a variety of organ system.

Sulphasalazine : This drug used in the treatment of ulcerative colitis. It has been found to be useful & much safer than gold salts in the treatment of RA.It is a compound of sulfapyridine and 5-amino salicylic acid (5-ASA. In addition, it suppresses the disease in significant number of RA patients. Efficacy of sulfasalazine in RA is modest and side effects are few, but neutropenia/thrombocytopenia occurs in about 10% patients and hepatitis is possible. It is used as a second line drug for milder cases. The dose required 1-2 gm. /day.

Methotrexate(Mtx): It acts by it’s ability to act as immunosuppressant. Much lower dose is needed –this explain it’s lower degree adverse effect in RA. Onset of symptom relief is relatively rapid (4–6 weeks), therefore preferred for initial treatment. Mtx is now the DMARD of first choice and the standard treatment for most patients, including cases of juvenile RA. Response is more predictable and sustained over long-term. Toxicity is low & mainly consist of ulceration of mucous membrane of bucal cavity, nausea, hepatotoxicity can rarely occur. Dose for RA is 7.5-15 mg orally,once a weak. Pregnancy , breast feeding, presence of peptic ulcer infection are among contraindication.

Chlorambucil: It is used for RA as well as alkylating agent in cancer. It acts by damaging the DNA & thus preventing cell replication in inflamed joint. This drug is rarely used when other DMARDs fail.

Azathioprine: This purine antimetabolite acts after getting converted to 6-mercaptopurine which causes suppression of immunoglobulin production & lymphocyte. It excreated rapidly & in few excreated slowly. It is usually given along with corticosteroids, it has a steroid sparing effect, for which it is primarily used now, especially in cases with systemic manifestations.

Leflunomide: This is a immunomodulatory drug. It acts by inhibits proliferation of activated lymphocytes in patients with active RA. Arthritic symptoms are suppressed and radiological progression of disease is retarded. Leflunomide is rapidly converted in the body to an active metabolite which inhibits dihydroorotate dehydrogenase and pyrimidine synthesis in actively dividing cells. Antibody production by B-cells may be depressed. The adverse effect associated with leflunomide are diarrhoea, headache, nausea, rashes, loss of hair, thrombocytopenia, leucopenia, increased chances of chest infection and raised hepatic transaminases. It is contraindicated in children and pregnant/ lactating women. Leflunomide is an alternative to Mtx or can be added to it, but the combination is more hepatotoxic. Combination with sulfasalazine improves benefit.

Cyclosporine:This drug is also used for treatment of RA but used only where most other DMARDs have failed. It causes inhibition of macrophages.

TNFα blocking factor : Cytokine are proteinaceous structure behaving like endocrines produced by various cell notably by the macrophages & lymphocytes. Tumor necrosis factor (TNF) is one of the cytokines whose amino acid sequence is known are called ‘interleukines’. These leads to inflammation.
Monoclonal antibodies (MAB) : These are produced by specially treated β- lymphocytes.
Individual drugs blocking TNFα action:
Adalimumab: it is an FDA approved drug. This is a recombinant monoclonal anti-TNF antibody is administered s.c. 40 mg every 2 weeks. thus it reduces inflammationin the joints affected by RA. Combination with methotrexate is advised to improve the response and decrease antibody formation.
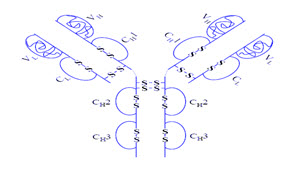
Infliximab: It is also FDA approved drug. It is a monoclonal antibody which can bind both with soluble as well as membrane bound TNF-α. It is usually combined with methotrexate which improves the response and decreases antibody formation against infliximab.
Etanercept: it is for treatment of RA & psoriatic arthritis as usual it suppresses the activity of TNF-α. It is a recombinant fusion protein of TNF receptor and Fc portion of human IgG. Pain, redness, itching and swelling occur at injection site and chest infections may be increased.

IL-1 antagonist- Anakinra: The naturally occurring IL-1 is produced during inflammation. It is bind with IL-1 receptor to produce other ILs which propmote inflammation. It is a recombinant human IL-1 receptor antagonist. Though clinically less effective than TNF inhibitors, it has been used in cases who have failed on one or more DMARDs.
Miscellaneous
Abatacept: It is an artificially prepared protein given in resistant cases of RA. Which has some adverse effect such as increased succeptibility to infection, anaphylaxis
Rituximab : It is a monoclonal antibody, combined therapy of rituximab & methotrexate has been approved for treatment of RA.
CONCLUSION
This disease may also result low red blood cell count, inflammation around the heart & lungs. As the pathology progress the inflammatory activity leads to tendon tethering & erosion & destruction of the joint surface, impairs range of movement & leads to deformity.
REFERENCES
1. T.L.Lemke, D.A.Williams ,Foye’s principle of medicinal chemistry, 6th edition, , page no.956
2. National Institute for Health and Clinical Excellence. Rheumatoid arthritis the management and treatment of rheumatoid arthritis in adults. CG79. London: NICE; 2009.
3. Scottish Intercollegiate Guidelines Network. Management of Early Rheumatoid Arthritis. SIGN Publication No. 48. Edinburgh: SIGN, 2000.
4. K.D.Tripathy, Essential of medical pharmacology, 6th edition, page no. 202-205
5. A summary medical pharmacology, Sujit.K. Choudhury, page no-287-290
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT editor-in-chief@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE









