{ DOWNLOAD AS PDF }
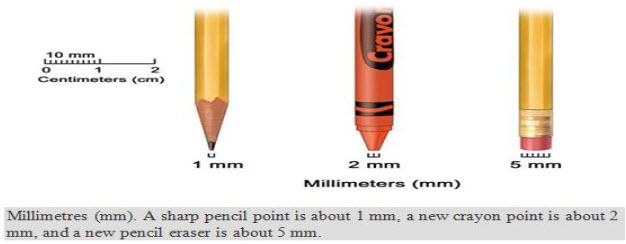
About Authors:
M.Sushma*, B.Vamsikrishna, M. Babu, R. Mohanraj
Department of Pharmacy Practice,
Raghavendra Institute of Pharmaceutical Education & Research (RIPER),
Anantapuram, Andhra Pradesh, INDIA
sushma.banthi@gmail.com
Abstract
Cervical cancer is a disease in which cancer cells form in the tissues of a woman's cervix. Globally, cervical cancer is the second most common cancer in women, and the fifth deadliest. Most common symptoms are increased vaginal discharge, Pelvic pain, Pain during sex. There are 4 stages of cervical cancer stage I, II, III, IV based on stage treatment is given. Diagnosis is done by pap smear, cone biopsy and cervical examining is done by colposcopy. Treatment options for women with cervical cancer are surgery, radiation therapy, Chemotherapy, and combination of these methods. Cervical cancer can be prevented by getting the HPV vaccine. Two types of vaccines are approved, Gardasil and Cervarix. They prevent against most types of HPV infection that cause cervical cancer, also Practice safer sex. Using condoms during sex reduces the risk of HPV and other sexually transmitted infections (STIs).
Background[1]
Cancer begins in cells, the building blocks that make up tissues. Tissues make up the cervix and other organs of the body. Normal cervical cells grow and divide to form new cells as the body needs them. When normal cells grow old or get damaged, they die, and new cells take their place. Sometimes, this process goes wrong, they buildup of extra cells often forms a mass of tissue called a growth or tumour.
Based on the Growths on the cervix it can be 2 types[21]:
|
Characteristics |
Benign |
Malignant |
|
Differentiation/anaplasia |
Well differentiated; structure may be typical of tissue of origin. |
Some lack of differentiation with anaplasia; structure is often atypical. |
|
Rate of growth |
Usually progressive and slow; may come to a standstill or regress;mitotic figures are rare and normal. |
Erratic and may be slow to rapid; mitotic figures may be numerous and abnormal. |
|
Local invasion |
Usually cohesive and expansible well-demarcated masses that do not invade or infiltrate surrounding normal tissues. |
Locally invasive, infiltrating the surrounding normal tissues; sometimes may be seemingly cohesive and expansible. |
|
Metastasis |
Absent |
Frequently present; the larger & more undifferentiated the primary, the more likely are metastases. |
Definition
Cervical cancer is a disease in which cancer cells form in the tissues of a woman's cervix[6]. It begins in cells on the surface of the cervix. Over time, the cervical cancer can invade more deeply into the cervix and nearby tissues[5][6]. Cervical cancer cells can spread by breaking away from the cervical tumour. They can travel through lymph vessels to nearby lymph nodes. Also, cancer cells can spread through the blood vessels to the lungs, liver, or bones. After spreading, cancer cells may attach to other tissues and grow to form new tumors that may damage those tissues.
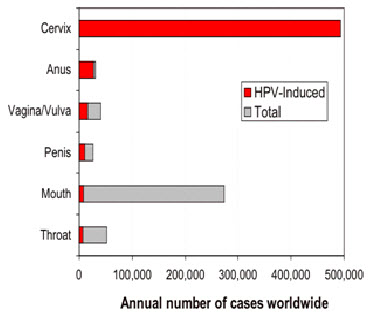
Cervical Cancer and Its anatomy
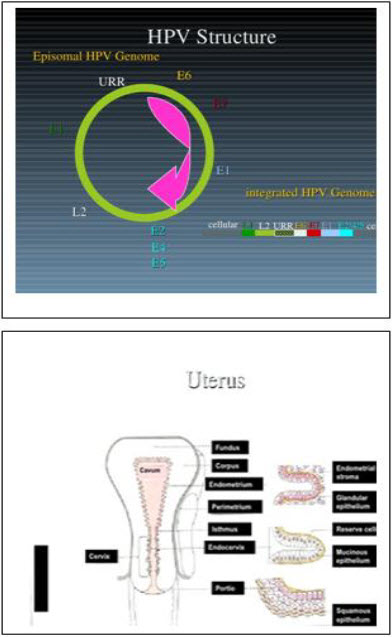
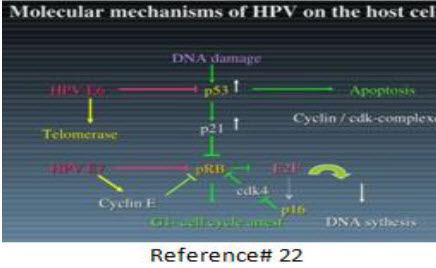
Human Papilloma Virus (HPV)
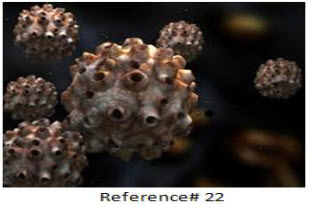
It is a virus from the papilloma virus family that affects human skin and moist membranes that line the body, such as the throat, mouth, fingers, anus and cervix. There are over 100 types, of which 40 can affect the genital area[5][6]. Most known HPV types cause no symptoms to humans, while a small number can increase the risk of developing several cancers, such as that of the cervix, penis, vagina, anus and oropharynx. According to recent studies, HPV infection can also raise cardiovascular disease risk.The HPV 16 and 18 strains, which are known to cause nearly all cases of cervical cancer, also raise the risk of developing oropharyngeal (throat) cancer[5][6].
Epidemiology
Incidence and mortality rate of cervical cancer
According to national cancer institute, estimated New cases-12, 340 and Deaths- 4030 from cervical cancer in the US in 2013. Globally, cervical cancer is the second most common cancer in women, and the fifth deadliest. In 2008, en estimated 473,000 women developed cervical cancer, and 253, 500 died of the disease. If every female were vaccinated against the HPV virus, hundreds of thousands of lives each year would be saved.
Clinical manifestations
Most of the time, early cervical cancer has no symptoms. Symptoms that may occur include[1]:
· Abnormal vaginal bleeding between periods, after intercourse, or after menopause
· Vaginal discharge that does not stop, and may be pale, watery, pink, brown, bloody, or foul-smelling
· Periods that become heavier and last longer than usual[1]
When the cancer grows larger, women may notice abnormal vaginal bleeding:
· Bleeding that occurs between regular menstrual periods, after sexual intercourse, douching, or a pelvic exam.[5]
· Menstrual periods that last longer and are heavier than before.
· Bleeding after going through menopause
· Increased vaginal discharge.[1]
· Pelvic pain.
· Pain during sex.
· Digital concept image of HPV / human papilloma virus.
Cervical cancer, infections, or other health problems may cause these symptoms. A woman with any of these symptoms should tell her doctor so that problems can be diagnosed and treated as early as possible.Cervical cancer may spread to the bladder, intestines, lungs, and liver. Often there are no problems until the cancer is advanced and has spread. Symptoms of advanced cervical cancer may include:
· Back pai
· Bone pain or fractures
· Fatigue
· Leaking of urine or faeces from the vagina
· Leg pain
· Loss of appetite
· Pelvic pain
· Single swollen leg ,Weight loss
Stages and treatment protocols of cervical cancer:
The stage is based on where cancer is found.
These are the stages of invasive cervical cancer[1][3]:
Carcinoma in Situ:
Stage 0
In carcinoma in situ (stage 0), abnormal cells are found in the innermost lining of the cervix. These abnormal cells may become cancer and spread into nearby normal tissue.
Treatment protocols for cervical cancer are provided below, including treatment by stage, chemo radiation therapy, and chemotherapy.
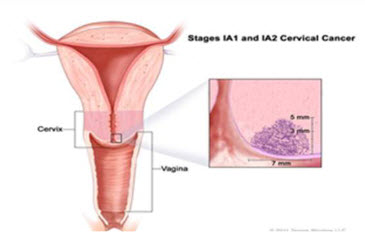
Stage IA1 disease:
Cancer cells are found only in the cervix.Primary treatment of early stage cervical cancer is surgery or radiation therapy Treatment recommendations include extra fascial hysterectomy, modified radical trachelectomy or hysterectomy with pelvic node dissection.[9]
Stage IA2 disease:
Patients with stage IA2 tumors are treated with radical hysterectomy or radical trachelectomy with pelvic lymph node dissection. Alternative options include brachy therapy with or without pelvic radiation therapy (total point A dose: 75-80 Gy)[10]
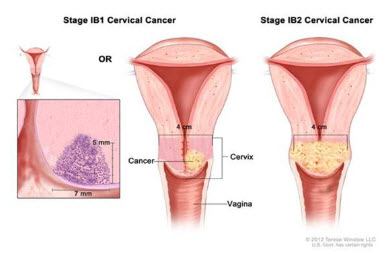
Stage IB and IIA:
Patients with stage IB or IIA disease can be treated with surgery (radical trachelectomy, pelvic lymphadenectomy, radical hysterectomy plus bilateral pelvic lymph nodes dissection), pelvic radiotherapy or chemo radiation[11, 12, 13, 14, 15, 16, 17, 18, 19, 20]. If lymph nodes are positive, then a hysterectomy is not recommended; instead patient should receive chemo radiation
Patients with stage IB or IIA may also be given pelvic radiotherapy and brachy therapy with or without concurrent cisplatin-based chemotherapy[1, 11, 12, 7, 13, 14, 15, 16, 17, 18, 19, 10]
Cisplatin 40 mg/m2 IV once weekly (not to exceed 70 mg/wk) plus radiation therapy 1.8-2 Gy per fraction (minimum 4 cycles; maximum 6 cycles) orCisplatin 50-75 mg/m2 IV on day 1 plus 5-fluorouracil (5-FU)1000 mg/m2 continuous IV infusion on days 2-5 and days 30-33 (total dose 4000 mg/m2 each course). Cisplatin 50-75 mg/m2 IV on day 1 plus 5-FU 1000 mg/m2 continuous IV infusion over 24 h on days 1-4 (total dose 4000 mg/m2 each cycle) every 3wk for a total of 3-4 cycles
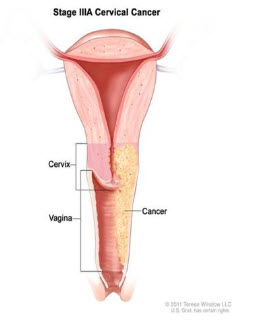
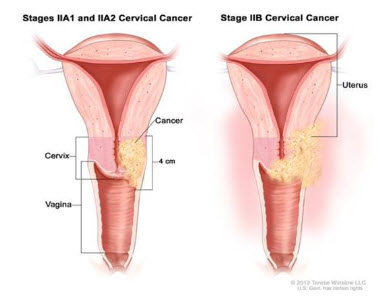
Stage IIB, IIIA, IIIB, and IVA:
The tumour has grown through the cervix and invaded the upper part of the vagina. It may have invaded other nearby tissues but not the pelvic wall or the lower part of the vagina[3]
Treatment recommendations for advanced disease include concomitant chemo radiation and brachy therapy[10, 11, 12, 13, 14, 15, 16, 17, 18, 19]
Cisplatin 40 mg/m2 IV once weekly (not to exceed 70 mg/wk) plus radiation therapy 1.8-2 Gy per fraction (minimum 4 cycles; maximum 6 cycles) or Cisplatin 50-75 mg/m2 IV on day 1 plus 5-fluorouracil (5-FU) 1000 mg/m2 continuous IV infusion on days 2-5 and Days 30-33 (total dose 4000 mg/m2 each course). Cisplatin 50-75 mg/m2 IV on day 1 plus 5-FU 1000 mg/m2 continuous IV infusion over 24 h on days 1-4 (total dose 4000 mg/m2 each cycle) every 3wk for a total of 3-4 cycles
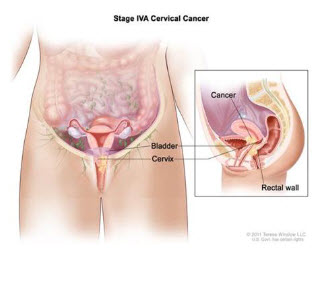
Stage IVB:
The tumour has invaded the bladder or rectum. Or, the cancer has spread to other parts of the body, such as the lungs.
Systemic therapy for stage IV recurrent or metastatic disease[10] [20, 11, 12, 13,14]:
Paclitaxel 135 mg/m2 IV over 24h (dosing at 175 mg/m2 IV over 3h is also acceptable) followed by cisplatin 50 mg/m2 IV on day 1 every 3wk or
Topotecan 0.75 mg/m2 IV (or 0.6 mg/m2 IV if prior radiation therapy) on days 1-3 followed by cisplatin 50 mg/m2 IV on day 1 every 3wk or Paclitaxel 175 mg/m2 IV over 3h on day 1 every 3 wk.
Second-line therapy for stage IV recurrent or metastatic disease:
National Comprehensive Cancer Network (NCCN) recommends agents such as bevacizumab, docetaxel, gemcitabine, ifosfamide, 5-FU, mitomycin, irinotecan, and topotecan, which are listed as category 2B (recommendations based on lower level of evidence)[10]Category 3 (recommendations based on any level of evidence) recommended drugs include pemetrexedand vinorelbine[10]
The rates below come from the 7th edition of the AJCC staging manual from data collected by the National Cancer Data Base, and are based on people diagnosed between 2000 and 2010[3].
|
Stage |
5-Year Observed Survival Rate |
Stage |
5-Year Observed Survival Rate |
|
IA |
93% |
IIIA |
35% |
|
IB |
80% |
IIIB |
32% |
|
IIA |
63% |
IVA |
16% |
|
IIB |
58% |
IVB |
15% |
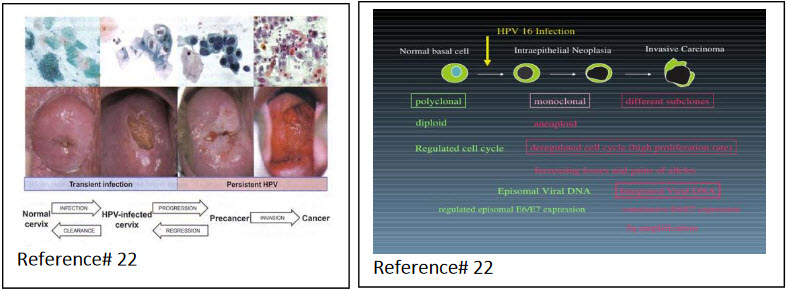
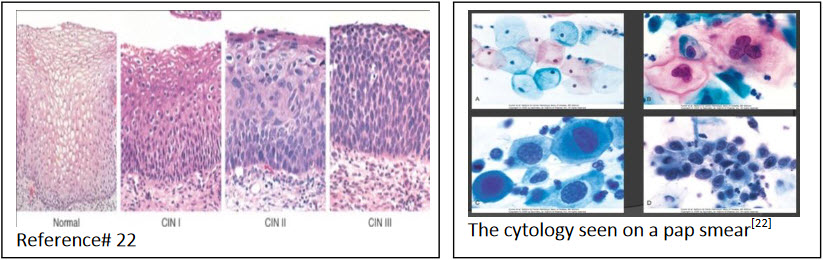
Pathophysiology:
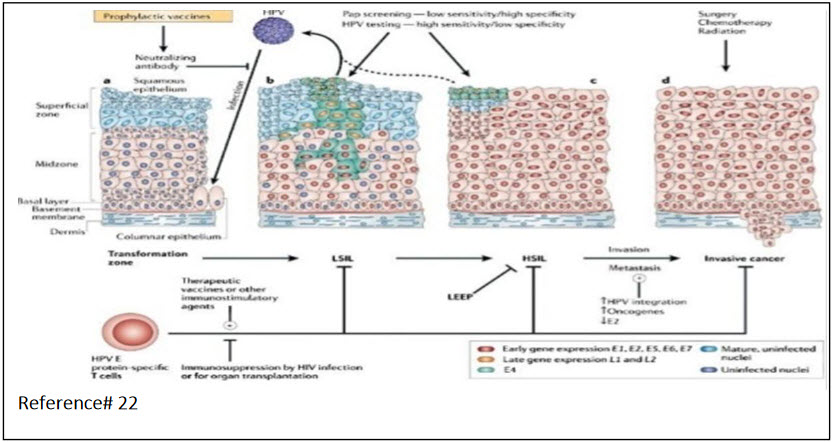
Histology:
Diagnosis:
Precancerous changes of the cervix and cervical cancer cannot be seen with the naked eye. Special tests and tools are needed to spot such conditions.
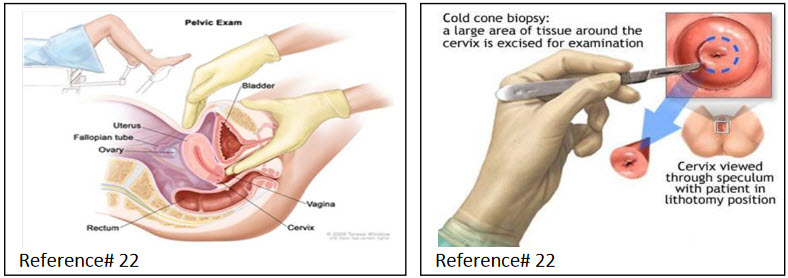
Pap smears screen for precancers and cancer, but do not make a final diagnosis[1]. If abnormal changes are found, the cervix is usually examined under magnification. This procedure is called colposcopy. Pieces of tissue are surgically removed (biopsied) during this procedure[1]. The tissue is sent to a laboratory for examination. A procedure called cone biopsy may also be done.

Lab tests: scraping a sample of cells from the cervix. For a Pap test, the lab checks the sample for cervical cancer cells or abnormal cells that could become cancer later if not treated. For an HPV test, the same sample is tested for HPV infection[1][9]. HPV can cause cell changes and cervical cancer.
Cervical exam: The doctor uses a colposcopy to look at the cervix. The colposcope combines a bright light with a magnifying lens to make tissue easier to see.
Tissue sample: The removal of tissue to look for cancer cells is a biopsy. Most women have cervical tissue removed in the doctor's office, and usually only local anaesthesia is needed. If cervical cancer is diagnosed, more tests are advised. These help determine how far the cancer has spread. This is called staging. Tests may include:
Chest x-ray:
· CT scan of the pelvis[8][1]
· Cystoscopy
· Intravenous pyelogram (IVP)
· MRI of the pelvis
· Stages of cervical cancer.
Treatment[2]:
· The stage of the cancer
· The size and shape of the tumour
· The woman's age and general health
· Her desire to have children in the future
· Early cervical cancer can be cured by removing or destroying the precancerous or cancerous tissue[2]. There are various surgical ways to do this without removing the uterus or damaging the cervix, so that a woman can still have children in the future.
Types of surgery for early cervical cancer include:
· Loop electrosurgical excision procedure (LEEP) -- uses electricity to remove abnormal tissue[11][1]
· Cryotherapy -- freezes abnormal cells
· Laser therapy -- uses light to burn abnormal tissue.
Treatment options for women with cervical cancer are:[1][2]
· Surgery[1]
· Radiation therapy[1]
· Chemotherapy
· A combination of these methods
· The choice of treatment depends mainly on the size of the tumour and whether the cancer has spread. The treatment choice may also depend on whether you would like to become pregnant someday.
Radiation: External radiation therapy: External radiation uses a machine that directs the rays at the pelvis or other tissues where the cervical cancer has spread[1]. This type of cancer treatment is given at a hospital or clinic, usually for 5 days per week over the course of several weeks[2][9].
Internal radiation therapy[2]: In this method, a thin tube filled with a radioactive substance is placed inside the vagina[1]. With this type of cervical cancer treatment, you will need to stay in the hospital during your treatment, which can last from a few minutes up to three days. The internal radiation therapy may be repeated a few times over the course of several weeks.
Hysterectomy for Cervical Cancer Treatment:A hysterectomy is an operation that removes the uterus, or womb.There are two types of hysterectomy: total and radical. In a total hysterectomy, your surgeon will remove your cervix and uterus[1]. In a radical hysterectomy, your surgeon will also remove tissue surrounding the cervix, part of the vagina, and possibly other parts of the reproductive system such as the fallopian tubes, ovaries, or lymph nodes, depending on the extent of your cervical cancer[1][2].
The operation may be performed in one of three ways; healing time varies depending on the method used[11].
|
Abdominal hysterectomy. |
The uterus is removed through an incision in the abdomen. |
|
Vaginal hysterectomy. |
The uterus is removed through the vagina. |
|
Laparoscopic hysterectomy. |
The operation is performed using surgical instruments inserted through small incisions. |
Risk factors[1][5]:
· HPV infection
· Cigarette smoking,
· AgeMultiparty
· Oral contraceptives,
· Other STD’s
· Poor nutritional status.
Prevention[1][4][5]
Cervical cancer can be prevented by doing the following:
· Get the HPV vaccine. Two types of vaccines are approved, Gardasil and Cervarix. They prevent against most types of HPV infection that cause cervical cancer.
· Practice safer sex. Using condoms during sex reduces the risk of HPV and other sexually transmitted infections (STIs).
· Limit the number of sexual partners you have. Avoid partners who are active in high-risk sex.
· If you smoke, quit. Smoking increases your chance of getting cervical cancer.
· Get regular Pap smears as often as your health care provider recommends. Pap smears can help detect early changes, which can be treated before they turn into cervical cancer.
Recommended age[1][5][9]:
The cervical cancer vaccine is recommended for girls and boys ages 11 to 12, although it can be given as early as age 9. It's important for girls and boys to receive the vaccine before they have sexual contact and are exposed to HPV. Once infected with HPV, the vaccine might not be as effective or might not work at all. Also, response to the vaccine is better at younger ages than it is at older ages.If the three-dose series of vaccines isn't completed by ages 11 to 12, the Centers for Disease Control and Prevention (CDC) recommends that girls and women through age 26 and boys and men through age 21 receive the vaccine. However, men can receive the HPV vaccine through age 26 if desired. Both vaccines are given as a series of three injections over a six-month period. The second dose is given one to two months after the first dose, and the third dose is given six months after the first dose.
Contraindicated[5][8]:
The cervical cancer vaccine isn't recommended for pregnant women or people who are moderately or severely ill. Tell your doctor if you have any severe allergies, including an allergy to yeast or latex. Also, if you've had a life-threatening allergic reaction to any component of the vaccine or to a previous dose of the vaccine, you shouldn't get the vaccine.
Nutrition:
Eating well is important before, during, and after cancer treatment. You need the right amount of calories to maintain a good weight[1]. You also need enough protein to keep up your strength. Eating well may help you feel better and have more energy.Sometimes, especially during or soon after treatment, you may not feel like eating. You may be uncomfortable or tired[1]. You may find that foods don't taste as good as they used to. In addition, poor appetite, nausea, vomiting, mouth blisters, and other side effects of treatment can make it hard for you to eat[2].
Outlook (Prognosis)[2] [18]:
Type of cervical cancer-some types does not respond well to treatment
1. Stage of cancer
2. Age and general health
3. If the cancer comes back after treatment
4. Two vaccines, Gardasil and Cervarix, are available to prevent HPV infection.
5. The prognosis of cervical cancer depends upon the stage and type of cervical cancer and the tumour size.
6. Precancerous conditions can be completely cured when followed up and treated properly. Most women are alive in 5 years for cancer that has spread to the inside of the cervix walls but not outside the cervix area. The 5-year survival rate falls as the cancer spreads outside the walls of the cervix into other areas.
Possible Complications[7] [6]:
· Women who have treatment to save the uterus have a high risk of the cancer coming back.
· Surgery and radiation can cause problems with sexual, bowel, and bladder function.
References:
1. medicinenet.com ... cancer az list …. cervical cancer index
2. macmillan.org.uk/Cancerinformation/Cancertypes/Cervix/Treatingcervicalcancer/ Treatmentoverview.aspx
3. cancer.org/cancer/cervicalcancer/detailedguide/cervical-cancer-survival
4. cancerresearchuk.org/cancer-help/type/cervicacancer/treatment/radiotherapy/cervical-cancer-radiotherapy-side-effects
5.cervical-cancer.emedtv.com/cervical-cancer-articles.html
6.Jhingran A, Russell AH, Seiden MV et al. Cancers of the cervix, vulva, and vagina. In: Abeloff MD, Armitage JO, Niederhuber JE, et al. eds. Abeloff’s Clinical Oncology.4thed. Philadelphia, PA: Elsevier Churchill-Livingstone; 2008:chap 91.
7.National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines): Cervical cancer. Version 2.2013. Available at nccn.org/professionals/physician_gls/pdf/cervical.pdf. Accessed November 16, 2012.
8.Noller KL. Intraepithelial neoplasia of the lower genital tract (cervix, vulva): Etiology, screening, diagnostic techniques, management. In: Katz VL, Lentz GM, Lobo RA, Gershenson DM, eds. Comprehensive Gynecology. 6th ed. Philadelphia, PA: Elsevier Mosby; 2012:chap 28.
9.NCCN Clinical Practice Guidelines in Oncology: Melanoma. V 3.2013. Available at bit.ly/mknnJ5. Accessed September 9, 2013.
10.Boss EA, van Golde RJ, Beerendonk CC, et al. Pregnancy after radical trachelectomy: a real option?Gynecol Oncol. Dec 2005;99(3 Suppl 1):S152-6. [Medline].
11.Chen Y, Xu H, Li Y, et al. The outcome of laparoscopic radical hysterectomy and lymphadenectomy for cervical cancer: a prospective analysis of 295 patients. Ann Surg Oncol. 2008;15:2847-55.
12.Koliopoulos G, Sotiriadis A, Kyrgiou M, et al. Conservative surgical methods for FIGO stage IA2 squamous cervical carcinoma and their role in preserving women's fertility. Gynecol Oncol. May 2004;93(2):469-73.[Medline].
13.Lowe MP, Chamberlain DH, Kamelle SA, et al. A multi-institutional experience with robotic-assisted radical hysterectomy for early stage cervical cancer. Gynecol Oncol. May 2009;113(2):191-4. [Medline].
14.Marchiole P, Benchaib M, Buenerd A, et al. Oncological safety of laparoscopic-assisted vaginal radical trachelectomy (LARVT or Dargent's operation): a comparative study with laparoscopic-assisted vaginal radical hysterectomy (LARVH). Gynecol Oncol. Jul 2007;106(1):132-41. [Medline].
15.Nezhat FR, Datta MS, Liu C, et al. Robotic radical hysterectomy versus total laparoscopic radical hysterectomy with pelvic lymphadenectomy for treatment of early cervical cancer. JSLS. Jul-Sep 2008;12(3):227-37. [Medline].
16.Plante M, Renaud MC, Hoskins IA, et al. Vaginal radical trachelectomy: a valuable fertility-preserving option in the management of early-stage cervical cancer. A series of 50 pregnancies and review of the literature. Gynecol Oncol. Jul 2005;98(1):310. [Medline].
17.Ramirez PT, Slomovitz BM, Soliman PT, et al. Total laparoscopic radical hysterectomy and lymphadenectomy: the M. D. Anderson Cancer Center experience. Gynecol Oncol. Aug 2006;102(2):252-5.[Medline].
18.Rotman M, Sedlis A, Piedmonte MR, et al. A phase III randomized trial of postoperative pelvic irradiation in Stage IB cervical carcinoma with poor prognostic features: follow-up of a gynecologic oncology group study. Int J Radiat Oncol Biol Phys. May 1 2006;65(1):169-76. [Medline].
19.Sedlis A, Bundy BN, Rotman MZ, et al. A randomized trial of pelvic radiation therapy versus no further therapy in selected patients with stage IB carcinoma of the cervix after radical hysterectomy and pelvic lymphadenectomy: A Gynecologic Oncology Group Study. Gynecol Oncol. May 1999;73(2):177-83.[Medline].
20.Chemoradiotherapy for Cervical Cancer Meta-Analysis Collaboration. Reducing uncertainties about the effects of chemoradiotherapy for cervical cancer: a systematic review and meta-analysis of individual patient data from 18 randomized trials. J Clin Oncol. Dec 10 2008;26(35):5802-12. [Medline].
21.Robbins pathological basis of disease; seventh 2005-kumar;page no: 281-282
22. medicine.net (images)
REFERENCE ID: PHARMATUTOR-ART-2193
|
PharmaTutor (ISSN: 2347 - 7881) Volume 2, Issue 6 Received On: 21/04/2014; Accepted On: 28/04/2014; Published On: 01/06/2014 How to cite this article: M Sushma, B.Vamsikrishna, M.Babu, R. Mohanraj; A Review on Role of Human Papilomma Virus (HPV) In Cervical Cancer; PharmaTutor; 2014; 2(6); 21-30 |
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE









