{ DOWNLOAD AS PDF }
About Authors:
M. Sushma*, T. V. V. Vidyadhar, R. Mohanraj, M. Babu
Department of Pharmacy Practice,
Raghavendra Institute of Pharmaceutical Education & Research, RIPER,
K R Palli Cross, Near S.K University, Anantapur District, Andhra Pradesh, 515721.
*sushma.banthi@gmail.com, vishnuvaravidyadhar@gmail.com
Abstract:
Gas gangrene is described as an infection of muscle tissue by toxin-producing clostridia. Gas gangrene is also known as “Clostridial myonecrosis”, gained recognition for its wartime incidence, during which only a paucity of civilian cases occurred during wars. Blood is major component in which its absences favour the development of gas gangrene. Such conditions were seen in the cases like atherosclerosis, diabetes, peripheral arterial disease. Depending on this blood supply and attack of infection the gas gangrene can be classified into Dry gangrene and Wet gangrene. This gas gangrene presents clinically with Dry and Cold skin with Pain and Swelling associated with Blisters. There are a typical causes and pathogenesis involving different type of toxins for the formation of gas gangrene. The treatment is approached by using a type ofMaggot therapy, Antibiotics, Oxygen therapy. Surgery also preferred in the treatment.
Introduction:
Gangrene is the destruction of tissue in the body where body tissue dies. It develops when the blood supply is lost to an affected body part because of various factors such as infection, underlying illness, vascular disease, or trauma. Gangrene can involve any body part, but the most commonly affected areas are the extremities (feet, arms, legs, hands)damaging organs and muscles. Gas-gangrene is a "serious infectious disease characterized by a local widespread serious and emphysematous phlegmonous inflammation, frequently associated with gangrene. There are different types of gangrene and all require immediate medical attention.
Definition:
Gas gangrene is a rapidly progressive, life-threatening, toxaemic infection of skeletal muscle caused by a dangerous strain of bacteria called “Clostridium”[2]. The organism exists naturally in the soil and gastrointestinal tract, thriving in anaerobic areas. Once it infects the muscle, it produces toxins that cause muscle death and an anaerobic environment essential to the survival of the bacterium. It is the toxins, not the bacteria, which cause.
Once established, the infection rapidly spreads to involve additional muscle, and gas may even be palpable in the affected area. It is a true medical emergency, and death can result in as little as 1 day [1].
Epidemiology[2]:
In 2003 there were only 22 recorded deaths in the U.S. During World War I, gas gangrene complicated 6% of open fractures and 1% of all open wounds.
|
World War I, |
randomly 5% |
|
World War II |
0.7% |
|
The Korean War, |
0.2% |
|
The Vietnam War |
0.02% |
Gas gangrene can be classified as posttraumatic, postoperative, or spontaneous. Posttraumatic gas gangrene accounts for 60% of the overall incidence; most cases involve automobile collisions.[3] Necrotizing fasciitis and gas gangrene were the most frequent, major and lethal complications observed in a review of 72 cases of complications caused by liposuction. In the US, about 900 to 1,000 cases of gas gangrene occur annually. [4]
Morbidity: Gas gangrene is undoubtedly an infection that carries a very high mortality/morbidity rate. The reported mortality rates vary widely, with a rate of 25% in most recent studies. The mortality rate approaches 100% in individuals with spontaneous gas gangrene and in those in whom treatment is delayed.[5]
Sex: Gas gangrene has no reported sexual predilection, and the sex of the individual does not affect the outcome.
Age: Although age is not a prognostic factor in gas gangrene, advanced age and comorbid conditions are associated with a higher likelihood of mortality.
Aetiology of Gangrene[2][15]:
Blood plays a very important role in maintaining health. When blood cannot travel freely throughout the body, the cells cannot survive, infection can develop, and tissue can die from gangrene. Any condition that affects blood flow increases your risk of gangrene, including:
- Atherosclerosis
- Diabetes
- Peripheral arterial disease
- Trauma
- Raynaud's phenomenon
Clinical manifestations:
- Infection spreads rapidly
- High blood pressure &sweating
- Cold and numb skin
- Pain may or may not be present.
- Swelling and pain at the site of infection
- Change in skin colour from red to brown to black
- Blisters or sores that produce a bad-smelling discharge (pus)
- Fever and feeling unwell
- A crackling noise that comes from the affected area when pressed
Classification/Gangrene Types[15]:
|
Dry gangrene |
Wet gangrene |
|
Definition Gangrene that develops as a result of arterial obstruction and is characterized by mummification of the dead tissue and absence of bacterial decomposition. Dry Gangrene is a condition in which especially affects fingers and toes. More common in people with autoimmune diseases and diabetes. However, dry gangrene can lead to wet gangrene if it becomes infected usually does not cause sepsis or cause the patient to die. |
Definition Wet gangrene is a condition mostly occurs in wet parts of the body like mouth, lungs, intestine and outer openings of sex organs Injury from burns, or trauma where a body part is crushed or squeezed, can rapidly cut off blood supply to the affected area, causing tissue death and increased risk of infection. A condition caused by relatively acute vascular occlusion–e.g., burns, freezing, crush injuries and thromboembolism, resulting in liquefactive necrosis. |
|
Reference # 18 |
Reference # 18 |
|
Causes for dry gangrene: Slow reduce or block blood flow conditions. Various external injuries like burns, accidents, wounds or surgery, Frostbite. Dry gangrene can also occur quickly due to rapid blockage in very small blood vessels. |
Causes of wet gangrene: May be bacterial infection in a part of the body where blood supply is blocked due to an illness or injury. This bacterial infection kills the tissues & turns into thick liquid mass. The bacteria grow fast producing toxic products that enter the blood stream (sepsis), leads to death. |
|
Symptoms: Numb sensation and coldness. Discolour, (reddish to brown finally black). If immediate loss of blood supply then first turn pale or bluish and then black The area shrinks and becomes dry. If not treated, chance of auto-amputation. |
Symptoms: Initial redness and then signs of decay (rotten tissue, pus, local oozing of fluid). Swelling and pain in infected area. A very bad smell from the infected area. A moist and black appearance of the infected area.
|
|
Management of dry gangrene: Dry gangrene is usually treated by surgically removing the dead part, such as a toe,the patient is treated with antibiotics to prevent infection in other parts. Medicines, which prevent blood from clotting, may also be given to reduce chances of blockade of blood vessel due to a blood clot. |
Management of wet gangrene: Wet gangrene is a medical emergency, and requires immediate attention. Debridement: Surgical removal of the dead and Sometimes infected arm or leg needs to be cut off (amputation). Such patients with amputation require rehabilitation therapy. Treatment with antibiotics Hyperbaric oxygen: Oxygen is given under pressure to the patient inside a chamber; this improves the oxygen supply to the affected area. |
Types of wet gangrene include[15][16]:
|
Internal gangrene |
Gas gangrene |
Fournier's gangrene |
|
If gangrene occurs inside the body, then it is referred to as internal gangrene. |
Gas gangrene is rare, but dangerous. It occurs when infection develops deep inside the body, such as inside muscles or organs, usually as a result of trauma. |
Fournier's gangrene: is also a rare condition, Fournier's gangrene is caused by an infection in the genital area. |
|
This is usually related to an infected organ such as the appendix or colon would be expected to have severe abdominal pain in the vicinity of the gangrene. Internal gangrene usually is painful in the area of the gangrene. |
The bacteria that causes gas gangrene, called clostridia, release dangerous toxins or poisons that spread throughout the body along with gas which can be trapped within body tissue. |
Men are affected more often than women. If the infection gets into the bloodstream, a condition called sepsis, it can be life-threatening. |
|
Reference # 19 |
Reference # 20 |
Reference # 21 |
Causes:
- Intramuscular or subcutaneous injections with insulin, epinephrine, quinine, heroin or cocaine are rare antecedent events leading to gas gangrene.
- A patient developed gas gangrene after injecting cocaine. Clostridium Septicum was isolated in both blood and wound cultures.
- PostoperativeClostridial infections follow cases of colon resection; ruptured appendix; bowel perforation; and biliary or other GI surgery, including laparoscopic cholecystectomy and colonoscopy[2][9]. It has also been reported following liposuction procedures.[16] Septic back-street abortions are the main cause of uterine gas gangrene.
- In a large series of non-traumatic C Septicum myonecrosis, malignant tumors were identified in 92% of patients; of these, 58% had colonic adenocarcinomas.[6][7]
- Non-clostridial organisms have been isolated in 60-85% cases of gas gangrene like Escherichia coli, Proteus species, Pseudomonas aeruginosa, and Klebsiella pneumonia.[8][9][10]
Pathogenesis:
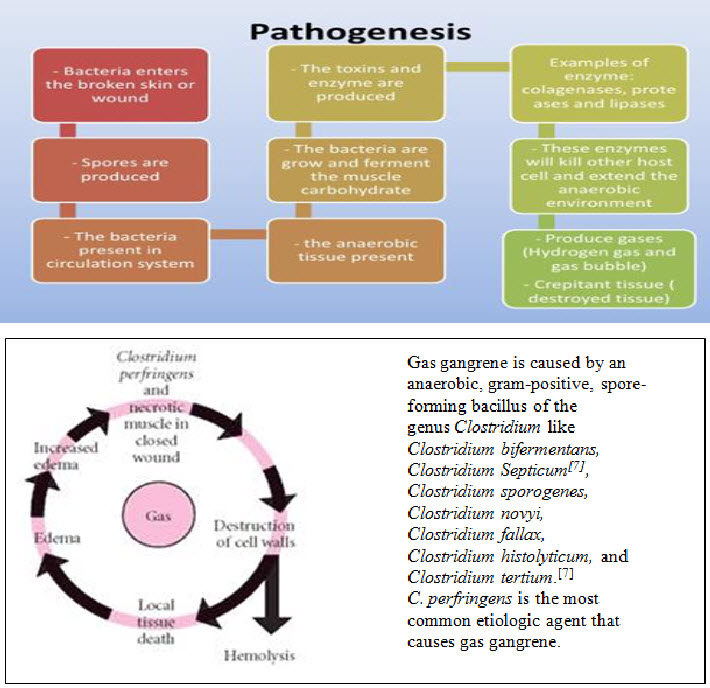
The most important exotoxins and their biologic effects are as follows[2][7]:
|
Alpha toxin - Lethal,* |
lecithinase, necrotizing, haemolytic, cardio toxic |
|
Beta toxin - Lethal,* |
Necrotizing |
|
Delta toxin - Lethal,* |
Haemolysin |
|
Epsilon toxin - Lethal,* |
Permease |
|
Iota toxin - Lethal,* |
Necrotizing |
|
Phi toxin |
Haemolysin, cytolysin |
|
Kappa toxin - Lethal,* |
collagenase, gelatinase, necrotizing |
|
Lambda toxin |
Protease |
|
Mu toxin |
Hyaluronidase |
|
* Nu toxin - Lethal,* |
deoxyribonuclease, haemolytic, necrotizing |
*Lethal as tested by injection in mice
Morphologic features:
Grossly, the affected area is swollen, oedematous, and painful & crepitant due to accumulation of gas bubbles with in the tissue. Subsequently the effected tissues become dark black and foul smell.
CONTRASTING FEATURES OF DRY & WET GANGRENE:
|
Dry gangrene |
Features |
Wet gangrene |
|
Commonly limbs |
Site |
Most common in bowel |
|
Arterial occlusion |
Mechanisms |
More commonly venous obstruction, less often arterial |
|
Organ dry ,shrunken & black |
Macroscopic |
Part moist, soft swollen, rotten & dark |
|
Limited due to very little blood supply |
Putrefaction |
Marked due to stuffing of organ with blood. |
|
Present at the junction between healthy & gangrenous part |
Line of demarcation |
No clear line of demarcation |
|
Bacteria fail to survive |
Bacteria |
Numerous present |
|
Generally better due to little septicaemia |
Prognosis |
Generally poor due to profound toxaemia |
Diagnosis:[11][12]
- Blood test
- Imaging Test (CT scan)(MRI)
- Surgery
- Fluid/tissue culture.
Differential diagnosis:[11][13]
- Abdominal Abscess
- Abdominal Trauma, Penetrating
- Abortion
- Clostridial Cholecystitis
- Sepsis, Bacterial
- Septic Shock
- Streptococcus Group A Infections
- Toxic Shock Syndrome
- Vibrio Infections
Laboratory Studies:[11][13]
- Rapidly developing haemolyticanaemia with an increased lactate dehydrogenase (LDH) level is common in patients with gas gangrene.
- One study reported the usefulness and good sensitivity of Gram stain (86%) in the diagnosis of clostridial gas gangrene in survivors of Wenchuan earthquake.[12]
- Less than 1% of blood cultures in patients with gas gangrene grow clostridial species.
- Radiography can help delineate the typical feathering pattern of gas in soft tissue; however, gas may not be present in patients with gas gangrene. Conversely, the simple presence of gas in soft tissue does not confirm the diagnosis of gas gangrene.
- CT scanning is also helpful, especially in abdominal cases of gas gangrene. A recent study with the new-generation CT scanners reported 100% sensitivity to detect necrotizing soft tissue infections; however, it excluded patients taken to surgery prior to CT scanning and did not explore surgically all clinically suspected cases.[13]
- Studies on MRI to detect necrotizing soft tissue infection have reported lower sensitivity (80-90%) and limited specificity[14].
- Ultrasound, although attractive as rapid bedside test, has not been well studied in this clinical scenario. In a cadaveric model of soft tissue gas, it showed excellent sensitivity in detecting gas and its localization.[15]
Other Tests:
- Rapid detection of alpha-toxin or sialidases (i.e., neuraminidases) in infected tissues through enzyme-linked immunosorbent assay (ELISA) is not widely available but represents a potential diagnostic tool. ELISA can provide results in as little as 2 hours when the test is applied to wound exudate, tissue samples, or serum.
- Although not widely available for clinical practice, in vitro amplification of the alpha-toxin or DNA by polymerase chain reaction (PCR) has been used to isolate clostridial species
Gangrene Warning:
If infection from gangrene gets into the blood, you may develop sepsis and go into septic shock. This can be life-threatening if not treated immediately[15]. Symptoms may include:
- Low blood pressure
- Rapid heartbeat
- Shortness of breath
- Change in body temperature
- Light-headedness
- Body pain and rash
- Confusion
- Cold, clammy, and pale skin
Gangrene Treatments:
- Treatment done by Antibiotics[17]( penicillin )(Clindamycin)
- Hyperbaric oxygen therapy
- Surgery (Amputation)
- Treatment for gangrene involves removing the dead tissue, treating and preventing the spread of infection, and treating the condition that caused gangrene to develop. The sooner you receive treatment, the better your chance of recovery.
Depending on the type of gangrene, treatment may include:
Maggot therapy: Maggots provide a non-surgical way to remove dead tissue. When used to treat gangrene, maggots from fly larvae are placed on the wound, where they consume the dead and infected tissue without harming healthy tissue. They also help fight infection and speed up healing by releasing substances that kill bacteria.
Antibiotics[17]: Antibiotics are used to treat and prevent infections. These are usually given by intravenous injection into a vein.
|
Gas gangrene Length of therapy: 10-28 days |
||
|
Penicillin G |
Usual dose: 0.5-4mu q 4-6h Max dose per day: upto 30 million units |
Renal dosing: > 50/usual dose 10-50/75% of usual dose <10/20-50%of usual dose |
|
Ceftriaxone |
Usual dose: 1-2g iv pb q24h Severe-2g iv pb q12h |
Renal dosing: no dosage adjustments required for renal failure PD -750mg iv pb q12h |
|
Clindamycin |
Usual oral dose: 150-450mg po q6h Usual IV dose: 600mg ivpb q6-8h or 900mg ivpb q8h Max daily dose: 4800mg |
Renal dosing: no dosage adjustments required for renal failure
|
|
Erythromycin |
Usual oral dose: 500mg -1g po q12h Usual IV dose : 250mg to 1g q6h.Max 4g/day |
>10/no change < 10/50-75% of usual dose. Max 2g/day |
|
Cefatoxime |
Mild infection: 1-2g iv pb q 12h Moderate:1-2g ivpb q8h Severe:2g ivpb q6-8h Life threatning:2g iv pb q4h |
>50/oral dose 10-50/q8-12h <10/q24h |
Oxygen therapy: Hyperbaric oxygen therapy may be used in some cases of wet gangrene or ulcers related to diabetes or peripheral artery disease.
During treatment, the patient is put in a specially designed chamber filled with oxygen at a higher pressure than oxygen found in the outside air. The theory is that this high level of oxygen saturates the blood and encourages healing of the dying tissue. Oxygen therapy may also reduce the growth of bacteria that cannot thrive in an oxygen-rich environment.
In order to prevent gangrene from occurring again, the cause of any blood supply blockage must be determined so that the underlying condition can be treated. Often vascular surgery, such as bypass surgery or angioplasty, is needed to restore blood flow. Medication to prevent blood clots may be used in some cases.
Fasciotomy for compartment syndrome may be necessary and should not be delayed in patients with extremity involvement.
Copious irrigation should be performed with sterile normal saline solutions and/or 3% liquid hydrogen peroxide.
Debridement of all wounds should be performed as soon as possible, with removal of badly damaged, contaminated, and necrotic tissue, especially in patients who might have been contaminated by soil, farm land, or dirty water.
Perform daily debridement as needed to remove all necrotic tissue until the wound has clean and healthy granulation tissue.
Amputation of the extremity may be necessary and lifesaving.
Abdominal involvement requires excision of the body wall musculature.
Uterine gas gangrene following septic abortion usually necessitates hysterectomy.
Prevention of Gasgangrene:
- Avoiding tobacco use and external trauma like frostbite can help prevent gangrene.
- Patients with diabetes should keep sugar levels under control and keep notice of their feet for any signs of cuts, infection, or redness.
- Patients with diabetic neuropathy
- Any wound or burn should be treated immediately, especially in the case of diabetics.
- Those who notice coldness and redness of a local area should immediately visit a doctor. Early diagnosis of any blockage in the blood vessel can prevent dry gangrene.
Further Inpatient Care:
- Daily or repeated surgical debridement
- Daily or repeated HBO therapy, if available
- Intensive supportive care
- Haemodialysis for renal failure, if indicated
Further Outpatient Care:
- Gas gangrene is one of the most devastating infections. Patients who survive the infection often sustain extremity amputation or massive loss of muscles, skin, and soft tissues, requiring extensive reconstructive surgery and physical rehabilitation.
- Patients with spontaneous gas gangrene may have occult malignancies of the GI tract. Carefully instruct these patients and monitor their cases appropriately.
Complications:
- Massive hemolysis, which may require repeated blood transfusion
- Disseminated intravascular coagulation (DIC), which may cause severe bleeding and may complicate aggressive surgical debridement
- Acute renal failure,sepsis
- Acute respiratory distress syndrome
- Shock, stupor
Patient counselling[7]:
- Avoid suturing wounds due to a crush injury or open fractures with devitalized muscle and soil contamination.
- Provide warnings and instructions of wound care to rescuers and health care workers about clostridial infections, including tetanus and gas gangrene, in injured victims of natural disasters such as earthquake or tsunami.
- Educate patients with spontaneous gas gangrene about the strong association with occult malignancies, especially malignancies of the GI tract.
- Educate intravenous drug users about potential fatal complications of gas gangrene due to injection of contaminated heroin or other chemicals.
Conclusion:
It is concluded that traumatic gas gangrene especially those caused by gunshot injuries are the type most commonlyseen in our locality and that delay in receiving appropriate treatment worsens its prognosis particularly, limb salvage.
REFERENCE
1.Chapnick EK, Abter EI. Necrotizing soft-tissue infections. Infect Dis Clin North Am. Dec 1996;10(4):835-55. [Medline].
2.De A, Varaiya A, Mathur M, Bhesania A. Bacteriological studies of gas gangrene and related infections. Indian J Med Microbiol. Jul-Sep 2003;21(3):202-4. [Medline]. [Full Text].
3.Brown PW, Kinman PB. Gas gangrene in a metropolitan community. J Bone Joint Surg [Am]. Oct 1974;56(7):1445-51. [Medline].
4.Stevens DL, Bisno AL, Chambers HF, Everett ED, Dellinger P, Goldstein EJ. Practice guidelines for the diagnosis and management of skin and soft-tissue infections. Clin Infect Dis. Nov 15 2005;41(10):1373-406. [Medline].
5.Stevens DL, Musher DM, Watson DA, et al. Spontaneous, nontraumatic gangrene due to Clostridium septicum. Rev Infect Dis. Mar-Apr 1990;12(2):286-96. [Medline]
6.Ustin JS, Malangoni MA. Necrotizing soft tissue infections. Crit Care Med. Apr 28 2011;[Medline].
7.De A, Varaiya A, Mathur M, Bhesania A. Bacteriological studies of gas gangrene and related infections.Indian J Med Microbiol. Jul-Sep 2003;21(3):202-4. [Medline]. [Full Text].
8.Hart GB, Lamb RC, Strauss MB. Gas gangrene. J Trauma. Nov 1983;23(11):991-1000. [Medline].
9.Nichols RL, Smith JW. Anaerobes from a surgical perspective. Clin Infect Dis. May 1994;18 Suppl 4:S280-6. [Medline].
10.Chen E, Deng L, Liu Z, Zhu X, Chen X, Tang H. Management of gas gangrene in Wenchuan earthquake victims. J Huazhong Univ Sci Technolog Med Sci. Feb 2011;31(1):83-7. [Medline].
11.Zacharias N, Velmahos GC, Salama A, Alam HB, de Moya M, King DR. Diagnosis of necrotizing soft tissue infections by computed tomography. Arch Surg. May 2010;145(5):452-5. [Medline].
12.Hopkins KL, Li KC, Bergman G. Gadolinium-DTPA-enhanced magnetic resonance imaging of musculoskeletal infectious processes. Skeletal Radiol. Jul 1995;24(5):325-30. [Medline].
13.Butcher CH, Dooley RW, Levitov AB. Detection of subcutaneous and intramuscular air with sonography: a sensitive and specific modality. J Ultrasound Med. Jun 2011;30(6):791-5. [Medline].
14.Determann C, Walker CA. Clostridium perfringens gas gangrene at a wrist intravenous line insertion. BMJ Case Rep. Oct 9 2013;2013:[Medline].
15.MedlinePlus: "Gangrene." (emedicine.medscape.com/article/214992-overview)NHS web site: "Gangrene."
16.Merck Manual of Medical Information-Second Home Edition: "Gas Gangrene."Radiopaedia.org: "Fournier gangrene."
17. globalrph.com/antibiotic/gangrene.htm
18. gangrenepictures.org/
19. clinicalscienceblogshabira.wordpress.com/2013/02/
20. bookdrum.com/books/all-quiet-on-the-western-front/9780449213940/bookmarks-26-50.html?bookId=1915
21. dermquest.com/image-library/image/5044bfd1c97267166cd67179?_id=5044bfd1c97267166cd67179
REFERENCE ID: PHARMATUTOR-ART-2155
|
PharmaTutor (ISSN: 2347 - 7881) Volume 2, Issue 5 Received On: 09/03/2014; Accepted On: 14/03/2014; Published On: 01/05/2014 How to cite this article: M Sushma, TVV Vidyadhar, R Mohanraj, M Babu; A Review on Gas Gangrene and its Management; PharmaTutor; 2014; 2(5); 65-74 |
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE









