{ DOWNLOAD AS PDF }
ABOUT AUTHORS:
Ranjana Joshi*, Shikha Jain, Kirti Jatwa, Monika Thakur, Anies Shaikh
Department of Pharmaceutics,
Mahakal Institute of Pharmaceutical Studies,
Ujjain, Madhya Pradesh, India
ranjanajoshipharma@gmail.com
ABSTRACT:
Prolotherapy is a technique which can be used to treat pain and injuries. Osteoarthritis is a disease acquired from daily wear and tear of joints and also due to injury. Prolotherapy is an injection technique which causes inflammation at the site of injection, new blood vessels form and mature, pain subsides and collagen density and tissue strength are increased. It works by stimulating the body’s own healing mechanism at the site of injection leading to long lasting relief of the injured area. This review focuses on the treatment of osteoarthritis using prolotherapy.
Arthritis is a form of joint disorder that involves inflammation of one or more joints. Arthritis is a joint disorder featuring inflammation. A joint is an area of the body where two different bones meet. A joint functions to move the body parts connected by its bones. Joint pain is referred to as arthralgia.The causes of arthritis depend on the form of arthritis. Causes include injury (leading to osteoarthritis), metabolic abnormalities (such as gout and pseudogout), hereditary factors, the direct and indirect effect of infections (bacterial and viral), and a misdirected immune system with autoimmunity (such as in rheumatoid arthritis and systemic lupus erythematosus).(14)
Classification of arthritis:-
- Osteoarthritis
- Rheumatoid arthritis
- Septic arthritis
- Goutand pseudo-gout
- Juvenile idiopathic arthritis
- Still's disease
- Ankylosing spondylitis
Osteoarthritis
Osteoarthritis is the most common form of arthritis. It can affect both the larger and the smaller joints of the body, including the hands, feet, back, hip or knee. The disease is essentially one acquired from daily wear and tear of the joint. Osteoarthritis can also occur as a result of injury. Osteoarthritis begins in the cartilage and eventually leads to the two opposing bones eroding into each other. Initially, the condition starts with minor pain while walking but soon the pain can be continuous and even occur at night. The pain can be debilitating and prevent one from doing some activities. Osteoarthritis typically affects the weight bearing joints such as the back, spine, and pelvis. More than 30 percent of females have some degree of osteoarthritis by age 65. Risk factors for osteoarthritis include: prior joint trauma, obesity, sedentary lifestyle.(1)(14)(15)
Diagnosis
Diagnosis is made by clinical examination from an appropriate health professional, and may be supported by other tests such as radiology and blood tests, depending on the type of suspected arthritis. All arthritis potentially features pain. Pain patterns may differ depending on the arthritis and the location. Rheumatoid arthritis is generally worse in the morning and associated with stiffness; in the early stages, patients often have no symptoms after a morning shower. Osteoarthritis on the other hand, tends to be worse after exercise. In the aged and children, pain might not be the main presenting feature; the aged patient simply moves less, the infantile patient refuses to use the affected limb.(14)
Elements of the history of the disorder guide diagnosis. Important features are speed and time of onset, pattern of joint involvement, symmetry of symptoms, early morning stiffness, gelling or locking with inactivity, aggravating and relieving factors, and other systemic symptoms. Physical examination may confirm the diagnosis, or may indicate systemic disease. Radiographs are often used to follow progression or help assess severity.(1)
Treatment of arthritis: The treatment of arthritis is very dependent on the precise type of arthritis present. An accurate diagnosis increases the chances for successful treatment. Treatments available include physical therapy, splinting, cold-pack application, paraffin wax dips, anti-inflammatory medications, immune-altering medications, and surgical operations. There is no cure for either rheumatoid orosteoarthritis. Treatment options vary depending on the type of arthritis and include physical therapy, lifestyle changes (including exercise and weight control), orthopedic branching and medications. Surgery may be required in eroding forms of arthritis. Medications can help reduce inflammation in the joint which decreases pain; arthritis can also be treated with prolotherapy
Prolotherapy strengthens the weak connective tissues. It involves injecting the non- active irritant solution into the body. It works on the simple healing mechanism of the body and stimulates the body to repair itself and it is a permanent treatment for chronic pain.(2)(14)
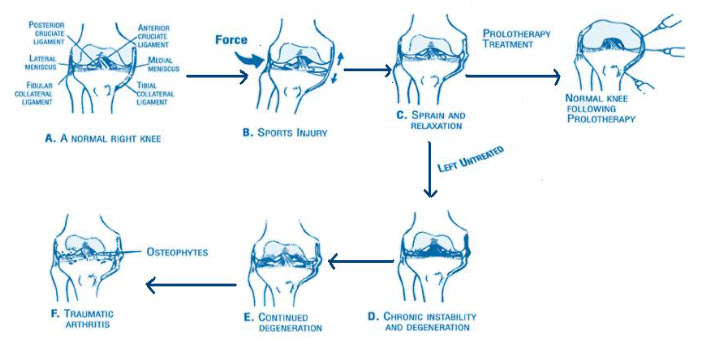
Figure 1 - Mechanism ofdegenerative arthritis.(3)
Prolotherapy
Regenerative Injection Therapy (RIT), also known as Prolotherapy, involves the injection at the enthesis (attachment site) of a damaged ligament or tendon with a substance that either directly or indirectly stimulates the body’s own inflammatory process, or a substance that directly or indirectly acts as a growth factor with the goal of producing the repair of the ligament or tendon with new healthy collagen tissue, the strength fibers of these structures(1)." Proliferative Injection Therapy" involves injecting an non-pharmacological and non-active irritant solution into the body, generally in the region of tendons or ligaments for the purpose of strengthening weakened connective tissue and alleviating musculoskeletal pain.(4)(16)(17)
Prolotherapy is a simple, natural technique that stimulates the body to repair the painful area when the natural healing process needs a little assistance.Prolotherapy is an injection technique that has been shown to cause proliferation of cells and tissue to stabilize and strengthen weakened joints, cartilage, ligaments and tendons. The injected solution intentionally causes controlled irritation in the injected tissue. This irritation is an inflammatory response, which increases the blood supply and thereby stimulates the tissue to heal and regrow new tissue.
Prolotherapy is also known as non-surgical ligament reconstruction, and is a permanent treatment for chronic pain.(4)(16)
What Prolotherapy rapidly produces is collagen and cartilage. Collagen is a naturally occurring protein in the body that is a necessary element for the formation of new connective tissue. These tissues include tendons, ligaments, muscle fascia and joint capsular tissue.
In now over four decades, no serious side effects from Prolotherapy have been reported in the medical literature despite millions of Prolotherapy treatments given. Prolotherapy is not dangerous, Prolotherapy cures chronic pain. The goal of Prolotherapy is to build the tissue back up. It is not effective for all joint pain, for example, Rheumatoid arthritis is not helped by Prolotherapy, but Osteoarthritis and degenerative arthritis often respond well.(16)(24) There are also non-inflammatory varieties of prolotherapy such as direct injection of recombinant polypeptide growth factors, examples of which include injection of erythrocyte growth factor (EGF) for patients with anemia or patients expected to incur blood loss(20,21) and injection of colony stimulating factor (CSF) for patients with leukemia with loss of white blood cells.(21,22)
Principle behind prolotherapy:
Prolotherapy works on a very simple principle: injecting the prolotherapy solution at the sites of pain and weakness, stimulates the body's own healing mechanism to repair and rebuild injured tissue into a stronger, more supportive, less painful tissue than it was before.(16),(17)
Prolotherapy is injection of any substance that acts as a ‘growth factor’, that is, which promotes growth of normal cells, tissues, or organs. The injections typically need to be repeated a number of times over a period of a few months.
The person treated will likely experience a few days of increased swelling and discomfort at the injection site-a necessary part of the healing process. There are three stages in the healing mechanism, they are: Inflammatory, Fibroblastic and Maturation. (5)
Characteristics of Prolotherapy:
1) It promotes the body’s own natural healing ability.
2) The natural functions of the body are regained and optimized.
3) No drugs or surgery are used.
4) It relieves pain.
5) In a double blind human study where neither the patients nor the researchers knew specifically who was receiving the treatment, 88.5% of those injected with the Prolotherapy solutions showed improvement.
6) Results are permanent (though aging continues).
7) It is a conservative treatment.
8) The solutions used are made from natural ingredients.
9) It is considerably less expensive than surgical intervention.
10) Enhancing the body’s innate ability to heal.(5)
Proliferants or injection ingredients for prolotherapy:
Proliferants:
Proliferants are "inflammatory agents" which, by initiating the first step in the wound healing cascade, lead to fibroplasia. Most basically, proliferants used for prolotherapy are substances injected into a ligament which lead to new collagen formation. Once the inflammation has begun and granulocytes and macrophages have been attracted to the injection site, fibroblasts will surely follow and deposit new collagen. The new collagen that is produced at the injection site undergoes contraction and pulls the ligament tighter. Proliferant solutions vary in the mechanism by which they cause localized inflammation but, in general, they all act by causing localized tissue trauma or irritation which initiates an influx of inflammatory cells. The exception to this rule is sodium morrhuate which may act as a chemotactic factor by a more direct mechanism. Injection ingredients for Prolotherapy consist of compounds that alleviate chronic pain. After injection, these substances attach to cell walls to stimulate the body’s reactive healing process.(6)(7)
Irritants:
The first class of proliferant solutions, called irritants or haptens, is exemplified by phenol, guaiacol and tannic acid. Each of these compounds has phenolic hydroxyl groups which are readily oxidized to produce reactive quinone like compounds which are known to directly alkylate the proteins on the surfaces of cells. By attaching themselves or their quinonoid oxidation products to the surfaces of cells at the injection site they either damage the cells directly or render them antigenic. In either case, granulocytes and macrophages are attracted to the injection site and early inflammation occurs; in other words, the wound healing cascade is initiated. Irritants with phenolic hydroxyl groups oxidize spontaneously to reactive quinoid compounds capable of alkylating cells.(6)(7)
Particulates:
Particulates such as pumice flour are irritants of a different type. Small particles, on the order of 1 micron, are noted for their ability to attract macrophages. The macrophages phagocytize small particles in the same way in which they ingest bacteria and cellular debris. This is the principle upon which cell sorters are used to separate macrophages from other cells; the macrophages are allowed to ingest magnetic particles and are then separated from other cells by a magnetic field. Once the macrophages arrive at the injection site, ingesting the pumice granules, they likely secrete polypeptide growth factors which result in fibroplasia and new collagen deposition. Granulocytes also may be attracted to the cellular trauma caused by injection of particulates.(6)
Osmotics:
A second class of proliferants is characterized by osmotic shock.Osmotic shock agents—the most frequently used compound in Prolotherapy—are simple compounds, such as dextrose and glycerine. These agents act by dehydrating cells at the injection site. In osmosis, concentrated solutions cause a net flow of solvent across a semipermeable membrane solution, the osmotic proliferant, causes a net flow of water into the injection site by removing water from living cells. They work by causing cells to lose water, which leads to cellular dehydration and then inflammation, triggering the healing response. Because these ingredients are water-soluble, they’re excreted from the body after producing the desired effect.
Upsetting the delicate balance within these living cells causes severe, but localized, tissue trauma, No doubt many of the cells at the injection site are killed. Cells at the injection site, which are either morbid or dead, release cellular fragments (proteins, membrane fragments) which are attractive for granulocytes and macrophages. Thus, local tissue damage causes an influx of inflammatory cells and initiates the wound healing cascade. Osmotic proliferants, concentrated solutions of simple water soluble compounds, include concentrated glucose, glycerin or zinc sulfate.
(Zinc sulfate may have other activities such as metallation of certain cellular proteins, causing secondary cellular injury; zinc binds very strongly to certain functional groups on proteins, particularly the sulfhydryl groups of cysteine. Glucose may have secondary effects as well. For example, it is known that in diabetics high local glucose concentrations lead to nonspecific glycosylation of some cellular proteins).(6)
Chemotactics:
A third class of proliferants only has one member currently; sodium morrhuate contains the biosynthetic precursor to certain chemotactic agents which attract inflammatory cells. Sodium morrhuate is the sodium salt of the fatty acid component derived from cod liver oil.Chemotactic agents, such as sodium morrhuate, a fatty acid derived from cod liver oil are generally used.(6)
Cold water fish oils are rich in polyunsaturated fatty acids such as arachidonic acid and related 20 carbon polyunsaturated fatty acids. These compounds are direct biosynthetic precursors to the mediators of inflammation such as prostaglandins, leukotrienes and thromboxanes. Cells use these compounds to communicate with other cells. For example, tissue trauma is thought to lead to the production of prostaglandins which promote vasoconstriction and swelling within the local area as well as attract granulocytes. It is thought that both the identity of the compounds produced and their concentration are important for intercellular communication. The documented powerful proliferant action of sodium morrhuate may be due to its arachidonic acid component being directly converted into prostaglandins and related mediators of inflammation.
Practitioners can add cofactors, such as the anti-oxidant mineral manganese. Or they can use a combination of glucosamine sulfate and condroitin sulfate, which may aid arthritic joint repair. Based on the combinations of compounds, these cofactors may increase efficacy.(6)
Proliferant Solution Choice and Preparation
Syringes or bags can be prepared using 1⁄4 volume of 50% dextrose (i.e., 3 ml in a 12-ml syringe) to make 12.5% soft tissue solution, or 1⁄2 volume for 25% joint injection solution(9)
Bottled phenol is obtainable from the manufacturer, allowing for small amounts to be added to ≥ 250 ml of 12.5% dextrose to convert solution to phenol-dextrose. Concentrations of 0.5–0.75 are alternatives to the 1.25% phenol concentration in the Ongley solution; remember to keep the volume of injection low.(9)
Sodium morrhuate is available as a 5% solution. One to 2 ml per 10-ml syringe makes a 0.5–1% concentration. Again, low volumes should be used. Its advantages over phenol are not established.(9)
MECHANISM OF PROLOTHERAPY:
There are many different types of prolotherapy. They range from the use of hypertonic dextrose or sugar (12.5–25%) solution, subcutaneous (under the skin injections) prolotherapy, platelet-rich plasma (concentrated platelet cells taken from the patient’s own blood) prolotherapy, and stem cell (precursor cells for all the other cell types of the body) prolotherapy using either bone marrow or adipose (fat) tissue(9).Prolotherapy strengthens ligaments and tendons by the stimulation of growth factors via the inflammatory healing cascade. An increase of glucose concentration causes an increase in cell protein synthesis, DNA synthesis, cell volume, and proliferation. This, in turn, stimulates ligament size and mass, tendon hypertrophy, extracellular matrix, ligament-bone junction strength, and repair of articular cartilage defects. The increase of glucose concentration from prolotherapy injections causes cells to produce different types of growth factors. These growth factors are pertinent to the repair, health, and growth of tendons, ligaments, and other soft tissues.(8)(10)
Healing Mechanisms:
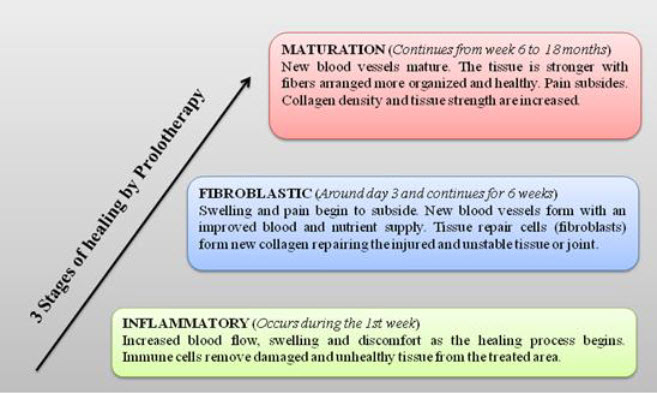
Figure 2 - Three stages of healing(5)
Mechanism:
Prolotherapy works by causing a temporary, low grade inflammation at the site of ligament or tendon weakness (fibro-osseous junction), “tricking” the body into initialing a new healing cascade. Inflammation activates fibroblasts to the area, which synthesize precursors to mature collagen, reinforcing connective tissue. This inflammatory stimulus raises the level of growth factors to resume or initiate a new connective tissue repair sequence to complete one which had prematurely aborted or never started. Prolotherapy is also known as “regenerative injection therapy (RIT),” “non-surgical tendon, ligament, and joint reconstruction” or “growth factor stimulation injection therapy.(9)(13)
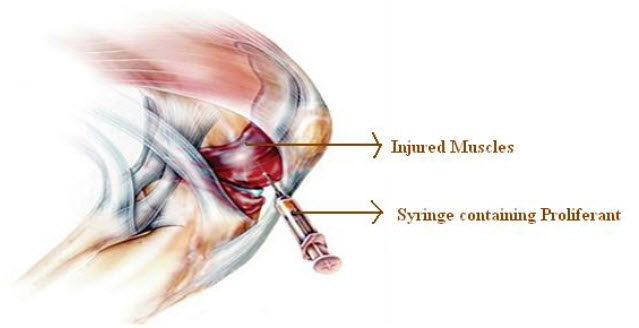
Figure 3 -Injection of proliferant into the muscle
Common injuries treated with prolotherapy(5)
|
CERVICAL SPINE Arthritis, Instability THORACIC SPINE Arthritis, Disc disease, Rib Dysfunction LUMBER SPINE Arthritis,spondylosis,instability SI JOINT Arthritis, Instability PUBIC SYMPHYSIS Osteitis pubis, Instability, Sports Hernia
|
ELBOW Instability Arthritis Tennis Elbow Triceps Tendonosis Golfers elbow |
KNEE Arthritis Ligament instability and tears Peripheral meniscal tears Runners Knee(Tendonosis) Osgood-Schlatters Disease Pes Anserine Tendonosis |
|
|
WRIST/HAND Thumb Arthritis and instability Carpal Bone instability Carpal tunnel syndrome TFCC tears Finger Arthritis |
|||
|
ANKLE/ FOOT Arthritis Instability/ Chronic Sprains Sinus Tarsi Syndrome Achilles Tendonosis/ Tears Plantar Faciitis |
|||
|
SHOULDER Instability, Recurrent Sublaxations Impingement syndrome, Arthritis of GH joint, Scalp injuries |
HIP/PELVIS Instability Arthritis Pelvis Tendonosis and pain Hip stabilizing muscles/tendons Chronic IT band Tendonosis Chronic Hamstring strains/tears |
Complications
The most common side effects related to prolotherapy are a temporary (12–96 hours) increase in pain, stiffness, and bruising at the injection site. Other possible side effects include headache, nausea, diarrhea, and minor allergic reaction to the medication. Rare injuries include lung collapse, disc injury, meningitis, hemorrhage, and nerve damage.(10)(11)
Contraindications
Active infection, cancer, non-reduced dislocations, or known allergy to any prolotherapy ingredients are contraindications to treatment, as is any known underlying illness which would interfere with healing. Acute gout or rheumatoid arthritis in the knee joint are also contraindications. Relative contraindications include current and long term use of high doses of narcotics as these medications can lower the immune response. Current use of systemic corticosteroids or NSAIDS are also relative contraindications as these are counter-productive to the inflammatory healing process.(3)
SIDE EFFECTS OF PROLOTHERAPY:
* In now over four decades, no serious side effects from Prolotherapy have been reported in the medical literature despite millions of Prolotherapy treatments given. Prolotherapy is not dangerous, Prolotherapy cures chronic pain.
* The most common prolotherapy side effect is muscle soreness around the injection site. Prolotherapy causes inflammation, so there may be bruising, pain, stiffness and swelling.
* Inflammation from prolotherapy typically lasts up to a week, but sometimes longer. Lingering pain is not viewed as a worrisome side effect and may be a sign of healing.
* Massage therapy and moist heat can relieve pain associated with prolotherapy. Anti-inflammatory medications should be avoided, but others such as acetaminophen (Tylenol) are allowed.
* Other possible serious side effects include spinal headache, hemorrhaging, collapsed lung and disk injury.
* Patient experiencing severe pain after prolotherapy may indicate an infection. (11)(12)(13)
CONCLUSION
Hence it can be concluded that prolotherapy is a technique which uses the natural healing process to strengthen the damaged ligaments and tendons. It can be easily used in the treatment of Osteoarthritis, joint pain, gout, sciatica and in all such painful conditions related to joint pain and damage. It uses only the natural solutions or irritants to activate the body’s natural healing mechanism. This technique can be widely used in today’s world as it can cause the permanent treatment of the osteoarthritis and other joint pain. This therapy appears safe and effective when performed by an experienced clinician. Prolotherapy also known as regenerative injection therapy involves the injection at the enthesis (attachment site) of a damaged ligament or tendon with a substance that either directly or indirectly stimulates the body’s own inflammatory process, or a substance that directly or indirectly acts as a growth factor with the goal of producing the repair of the ligament or tendon with new healthy collagen tissue.
REFERENCES
1.VanItallie T.B."Gout: epitome of painful arthritis". Metab. Clin. 2010;Exp. 59 : S32–6.
2.Torland Paul D, Kozar Albert J, Zannotti Chad M, Ewing Shannon E. Regenerative injection Therapy, Valley sports physicians and orthopedic medicine, Valley Sports Physicians 54 West Avon Road,Suite 202
3.Alderman Donna. Prolotherapy for Knee pain. Practical pain management. 2007;70-79
4.Goswami Amitabh. Patient education and self-Advocacy: Questions and responses on pain management. Journal of Pain & Palliative Care Pharmacotherapy. 2012;26:376–378.
5.Baumgartner Joel. Prolotherapy and PRP(Platelet Rich Plasma). Rejuvmedical orthopedic & sports medicine; (320), 217-8480.
6.Banks Allen R. A rational for prolotherapy. Journal of Orthopaedic Medicine .1991;13:3.
7.Judson C.H, Wolf J.M., Lateral Epicondylitis: A Review of Injection Therapies. The Orthopedic Clinics of North America. 2013;4:615-623.
8.Distal LM, Best TM. Prolotherapy: a clinical review of its role in treating chronic musculoskeletal pain. PM&R. 2011;3:S78–S81.
9.Reeves KD. Prolotherapy: Basic Science, Clinical Studies, and Technique. In Lennard TA (Ed) Pain Procedures in Clinical Practice. Hanley and Belfus. Philadelphia. 2000: 172-190.
10. Laura Johannes. A Pinch of Sugar for pain. Wall Street Journal.2012
11.Dagenais S. Intraligamentous injection of sclerosing solutions: prolotherapy for spine pain: a critical review of the literature. Spine J. 2005;5:310–328.
12.Reeves Dean K. Prolotherapy: basic science, clinical studies and technique. 172-190. Felson DT. Clinical practice. Osteoarthritis of the knee. N Engl J Med. 2006;354(8):841-848.
13.Felson DT. Epidemiology of osteoarthritis. In: Brandt KD DM, Lohmander LS, eds. Osteoarthritis. Oxford, England: Oxford University Press; 2003:9-16.
14.Rabago D, Slattengren A, Zgierska A. Prolotherapy in primary care practice. Prim Care. 2010;37:65-80.
15.Reeves KD, Hassanein K. Randomized prospective double-blind placebo-controlled study of dextrose prolotherapy for knee osteoarthritis with or without ACL laxity. Altern Ther Health Med. 2000;6(2):68-74,77-80.
16.Fleming S, Rabago DP, Mundt MP, Fleming MF. CAM therapies among primary care patients using opioid therapy for chronic pain. BMC Complement Altern Med. 2007;7:15.
17.Rabago D, Best T M, Zgierska A E, Zeisig E, Ryan M, Crane D. A systematic review of four injection therapies for lateral epicondylosis: prolotherapy, polidocanol, whole blood and platelet-rich plasma. Br J Sports Med 2009;43:471–481.
18.Gombotz H, Gries M, Sipurzynski S, Fruhwald S, Rehak P. Preoperative treatment with recombinant human erythropoietin or predeposit of autologous blood in women undergoing primary hip replacement. Acta Anaesthesiol Scand. 2000 ;44:737-747.
19.Matsuda S, Kondo M, Mashima T, Hoshino S, Shinohara N, Sumida S. Recombinant human erythropoietin therapy for autologous blood donation in rheumatoid arthritis patients undergoing total hip or knee arthroplasty. Orthopedics. 2001; 24:41-44
20.Bishop MR, Tarantolo SR, Geller RB, et al. A randomized, double-blind trial of filgrastim (granulocyte colony-stimulating factor) versus placebo following allogeneic blood stem cell transplantation. 2000;96:80-85.
21.Garcia Carbonero R, Mayordomo JI, Tornamira MV. Granulocyte colony-stimulating factor in the treatment of high-risk febrile neutropenia: a multicenter randomized trial. J Natl Cancer Inst. 2001;93:31-38.
22.Reeves K. Dean, Hassanein Khatab M., Long Term Effects Of Dextrose Prolotherapy For Anterior Cruciate Ligament Laxity. Alternative Therapies, 2003; 9: 58-62
REFERENCE ID: PHARMATUTOR-ART-2207
|
PharmaTutor (ISSN: 2347 - 7881) Volume 2, Issue 7 Received On: 16/04/2014; Accepted On: 19/05/2014; Published On: 01/07/2014How to cite this article: R Joshi, S Jain, K Jatwa, M Thakur, A Shaikh; Prolotherapy for Arthritis- A Review; PharmaTutor; 2014; 2(7); 54-62 |
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE









