{ DOWNLOAD AS PDF }
ABOUT AUTHORS:
V. Sravanthi*1, Mayure vijay kumar1, Donthineni Kalyan2, G.J.Finny1, C.P.Meher1
1Department of pharmaceutical chemistry, Maheshwara College of Pharmacy
2Department of Pharmaceutical Analysis, Saraswathi College of Pharmaceutical Sciences.
Isnapur chitkul ‘X’ road, Patancheru, Hyderabad-502307
*v.sravanthi27@gmail.com
ABSTRACT:
TIA stands for transcient ischemic attack, is a temporary blockage of blood flow in the brain that causes stroke symptoms. A transient ischemic attack is often called a mini-stroke. It is considered a warning sign that a more serious stoke will happen in the future. They may include weakness on one side of the body, dizziness, blurred vision, confusion, and speech problems. A TIA is a medical emergency. Following the below words cover about transient ischemic attacks (TIA), medication, prevention, diagnosing etc.
INTRODUCTION:
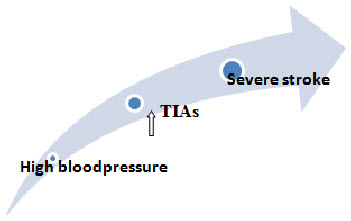
Transient ischemic attack (TIA) isoften labeled “mini-stroke” it is more accurately characterized as a “warning stroke,” a warning you should take very seriously. Ischemia results to the transcient episode of neurogic dysfunction either by focal brain or spinal cord. symptoms of TIAs preferred as contra lateral paralysis, sudden weakness or numbness etc., it also causes a sudden dimming or loss of vision, aphasia, slurred speech and mental confusion. But it lasts for less than 24hrs. TIA’s relates to the strokes which frequently referred as “mini-stroke”. Brain injury may be the chance with the presence of TIAs.1,2 A silent stroke differs from a TIA in that there are no immediately observable symptoms. A silent stroke often occurs before or after a TIA or major stroke.3
MEDICATION:
ASPIRIN + DIPYRIDAMOLE4:
|
S.NO |
STAGE |
DRUG |
CATEGORY |
SIDE EFFECTS |
|
1 |
primary |
ASPIRIN + dipyridamole (combination used for 2 years) |
anti-platelet |
Dipyridamole: headaches ,dizziness, nausea |
|
2 |
secondary |
Aspirin: (reduce TIA by 25%) |
anti-platelet |
Aspirin: stomach irritation, indigestion, nausea |
CLOPIDOGREL4:
|
S.NO |
DRUG |
USED |
CATEGORY |
SIDE EFFECTS |
|
1 |
CLOPIDOGREL |
severe side effects from taking aspirin |
Antiplatelet |
Diarrhoea ,Indigestion, Bruising, Bleeding |
TICLOPIDINE4:
|
S.NO |
DRUG |
USED |
CATEGORY |
NOTE |
|
1 |
TICLOPIDINE |
Used for patients who cannot tolerate or do not respond to aspirin therapy. |
Second-line Antiplatelet
|
Alternative to clopidogrel |
ANTI-COAGULANT MEDICATION4:
WARFARIN:
|
S.NO |
DRUG |
DESCRIPTION |
CATEGORY |
SIDE EFFECTS |
|
1 |
Warfarin |
Need regular (INR) tests. |
Anti-coagulant |
Bleeding, blood in your vomit, coughing up blood, unusual headaches |
|
Medication options for secondary prevention of ischemic stroke:4 |
||||
|
CARDIO-EMBOLIC: |
||||
|
DRUG |
DOSE |
NOTES |
||
|
Warfarin |
5 mg oral daily |
For atrial fibrillation titrate INR to 2-3 |
||
|
Aspirin |
325 mg oral daily |
Only appropriate if warfarin contraindicated |
||
|
NON-CARDIOEMBOLIC: |
||||
|
DRUG |
DOSE |
NOTES |
||
|
Aspirin/ ER dipyridamole |
25mg / 200mg oral daily |
Headache is common |
||
|
Clopidigrel |
75mg oral daily |
Preffered agent for aspirinallergy |
||
|
Aspirin |
50-325 mg oarl daily |
Least expensive antiplatelet agent |
||
BLOOD PRESSURE MEDICATION4:
CHOLESTEROL MEDICATION:
- High cholesterol à increase risks of having a TIA.
- lower cholesterol by making certain lifestyle changes, such as eating a healthy, balanced diet can avoid TIA.
- Statins are used to lower the cholesterol level.
- Statins help reduce the production of cholesterol in liver5.
CAROTID ENDARTERECTOMY:
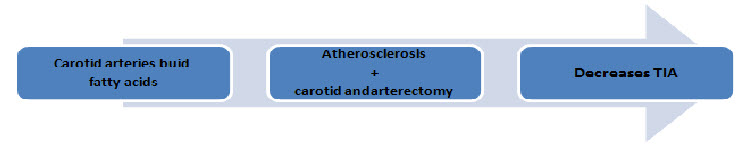
CAUSES:
- Atherosclerotic plaque
- Thrombus
- Excessive narrowing of large vessels
- Increased blood viscosity.
- Hypertension,
- Heart disease(especially atrial fibrillation),
- Migraine,
- Hypercholesterolemia, and
- Diabetes mellitus6.
INITIAL WORK-UP FOR SUSPECTED TIA:
The first step in evaluating a patient with symptoms of TIA is to confirm the diagnosis7.
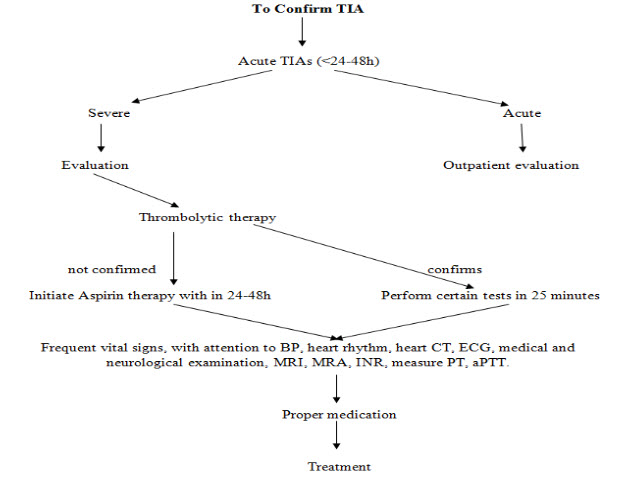
Pt= prothrombin time, aPTT= activated partial thromboplastin time, INR= International Normalized Ratio, MRI= magnetic resonance imaging, MRA= magnetic Resonance angiography
TYPICAL CHARACTERISTICS OF ISCHEMIC SYNDROMES INVOLVING THE ANTERIOR AND POSTERIOR CIRCULATIONS 8:
|
ISCHEMIC SYNDROME: |
SIGNS |
SYMPTOMS |
|
CIRCULATION |
||
|
Anterior circulation
Posterior circulation |
Visual-field cut |
Inability to see well (i.e., difficulty reading or driving) |
|
Language dysfunction (left hemisphere most often affected): aphasia |
Difficulty finding or understanding words, inability to read, garbled or slurred speech |
|
|
Motor dysfunction: contralateral face, arm, or leg weakness |
Dropping objects; depending on severity, inability to lift or move a body part or objects |
|
|
Sensory dysfunction: contralateral increased or decreased sensation to pain, heat, or cold
Behavior dysfunction (right hemisphere): inattention to surrounding environment, particularly to one side; if severe, patient may deny deficits or even his or her own body parts
Nystagmus |
Tingling (paresthesias), numbness, or pain
The patient usually reports no symptoms, but family members or others report that the patient has difficulty dressing, ignores half of food on a plate, or has poor attention to one side of the room or to someone speaking to the patient on one side versus the other (most often, the left side is ignored).
Vertigo (spinning sensation) |
|
|
Disconjugate gaze |
If subtle, blurry or double vision |
|
|
Bilateral signs |
Abrupt weakness of both legs, falling |
MISCELLANIOUS DRUGS:
COUMADIN:
(Warfarin sodium) is used to treat blood clots and to lower the chance of blood clots forming in your body. Blood clots can cause a stroke, heart attack, or other serious conditions if they form in the legs or lungs9.
STATINS:
Statins are used to lower LDL cholesterol. Statins can help lower the risk of heart attack, stroke, and death in people who are at high risk of a heart attack or stroke.
Statins and statin combinations can:
- Decrease the level of heart attack. 10
- Decrease in stroke level.
- Reduce LDL by 18%-55%.
- Increase HDL by 5% to 15%.
- Reduce triglycerides by 7% to 30%.11
RISK FACTORS12:
|
RISK FACTORS FOR TIA |
|
|
Hypertension |
Current smoking |
|
Hypercholesterolaemia |
High waist-to-hip ratio |
|
High dietary risk score |
Lack of regular exercise |
|
Diabetes mellitus |
Excess alcohol consumption |
|
Psychological stress |
Cardiac causes (AF or previous MI) |
RISK OF STROKE:
More than 20% of strokes are preceded by a TIA, Reliable estimations of this risk are necessary for educating the population and planning effective service provision and appropriate follow-up by specialist services. The early risk of stroke after TIA varies widely between 3% and 11% at seven days; a significant difference, with the lowest risk being when emergency treatment has been given by specialised stroke services.13
DIAGNOSTIC TESTS:
Brain Imaging:
(CT) Computed tomographic scanning of the head without contrast medium should be performed to identify sub-arachnoid hemorrhage, intracranial hemorrhage, or subdural hematoma. In hemorrhage, anticoagulants worsen the central nervous system bleeding should be avoided.
Patient with hypertension-mediated intracranial hematoma, and further testing may be required if the patient is found to have subarachnoid hemorrhage (e.g., cerebral angiography to rule out aneurysm).
It can identify conditions that mimic TIA, including tumors and other masses, as well as conditions that are associated with seizures or auras. A head CT scan can identify signs of early brain damage or evidence of old strokes.14,15 Finally, CT scanning of the head with contrast medium should be performed in the febrile patient to rule out an infectious cause or in the patient with a suspected mass (e.g., metastatic carcinoma, abscess).
Electro physiologic Testing:
The patient with cardiac disease, echocardiography should be performed EPT15,16. Atrial fibrillation and left ventricular hypertrophy are important risk factors for stroke. In patients with untreated atrial fibrillation, echocardiography may identify a thromboembolic source or left ventricular systolic dysfunction, both of which are common predictors of ischemic stroke.17
Transesophageal echocardiography is superior to transthoracic echocardiography to evaluate the possiblility dysfunction of the left atrium (including thrombus), atrial septal defects (including aneurysm), and aortic plaque. Recent clinical trials18,19 suggest that transesophageal echocardiography should be considered in patients without an identifiable cause of TIA or known cardiac disease, because it may detect a condition requiring therapeutic intervention (e.g., anticoagulation for thrombus). Aortic plaque, which has been associated with stroke, can be visualized well on transesophageal echocardiography.
FOLLOW-UP EVALUATION:
LIPID PROFILE:
Treatment with statins (3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors) reduces the risk of stroke by about 30 percent in patients with CHD.20,21 Therefore, a fasting lipid profile reflective of the patient's normal eating habits should be obtained, and statin therapy should be initiated if indicated.
HYPERCOAGULABLE STATES:
Patients with stroke, migraine, spontaneous abortion, pulmonary emboli, or deep venous thrombosis, should be evaluated for hyper coagulable states. Initial tests include ESR, antinuclear antibody test, rapid plasma reagent test, and antiphospholipid antibody tests. Referral to a hematologist or neurologist can ensure cost-effective evaluation of the multiple coagulation-factor abnormalities and conditions that can cause embolic stroke.
TESTING FOR ARTERIAL PATENCY AND BLOOD FLOW:
Carotid duplex ultra sonography should be performed in a reliable laboratory, preferably one with validation against the results of cerebral angiography. Alternatively, cerebral and cervical vessels can be evaluated by magnetic resonance angiography (MRA) with contrast medium or by CT angiography. If the work-up demonstrates carotid or other large-vessel atherosclerotic disease in the patient with TIA and unrecognized CHD, coronary artery testing is recommended.22
MRI: (Magnetic Resonance Imaging)
Advantages of MRI of the brain over CT scanning of the head include:
- Better imaging of tissues (i.e., greater sensitivity for early edema),
- Superior imaging within the posterior fossa (including the brainstem and cerebellum),
- Additional planes of imaging (sagittal, coronal, and oblique),
- No exposure to radiation.
Disadvantage of brain MRI: Inidentifying hemorrhage.
When cerebro vascular malformation, aneurysm, cerebral venous thrombosis, or arteritis is suspected, MRI or MRA is preferred. Diffusion-weighted imaging detects cellular edema as early as 10 to 15 minutes after symptom onset. However, this technique is not yet widely available.
MRA: (Magnetic Resonance Angiography)
Current MRA techniques use intravenously administered contrast medium (gadolinium) to visualize the vessels. MRA with the administration of contrast medium also is effective in identifying vertebra basilar stenosis,23 Depending on the MRA acquisition technique, the percentage of intracranial vessel stenosis can be overestimated24. Therefore, if accuracy is therapeutically important, cerebral angiography is necessary.
When near occlusion of the carotid artery cannot be distinguished from complete occlusion on MRA or carotid Doppler ultrasound studies, cerebral angiography should be considered. Surgery generally cannot be performed on completely occluded vessels.
Patients with carotid artery dissection can present with acute or subacute unilateral neck, head, or jaw pain. These symptoms may be associated with visual or language deficits, or with sensory motor deficits, particularly in the opposite arm. More typically, patients with carotid artery dissection present with only some of these features, such as temporal headache with lateral neck pain and, possibly, transient visual obscuration (amaurosis fugax) because of thromboemboli in the ophthalmic artery. Both carotid and vertebral artery dissections have been described after trauma, If the MRI or MRA study is inconclusive, cerebral angiography should be used to rule out arterial dissection or better define the percentage of vessel narrowing.
CT Angiography:
CT angiography also is becoming a useful imaging modality for identifying carotid or vertebral artery dissection. Conventional CT scanning in combination with CT angiography currently is being evaluated as an addition to the diagnostic imaging tools for use in patients with TIA or stroke. This combination can provide useful information about vascular anatomy and the extent and location of infarction. It may allow rapid evaluation of patients with TIA or stroke in hospitals or institutions that do not have MRI capability.
Cerebral Angiography:
It is the gold standard technique for complete evaluation of intracranial and extra cranial vessels. With cerebral angiography, both arterial and venous phases of cerebral blood flow can be visualized (dynamic study). However, cerebral angiography is an invasive technique that can result in neurologic complications (total incidence rate: 1.3 to 4.6 percent),25,26 including major stroke or death in 0.1 to 1.3 percent of patients, depending on the study.27,28
Relative indications for cerebral angiography include suspected carotid dissection unconfirmed on a noninvasive neuroimaging study, subarachnoid hemorrhage (to identify bleeding source), intracerebral hemorrhage in the absence of hypertension, and vasculitis. If one of these conditions is suspected, referral to a neurologist can be helpful in obtaining and interpreting the angiogram.
CONCLUSION:
“Transcient ischemic attack” as it is mentioned as a temporary blockage of blood supply to the brain. It can cause the severe chronic effects to the brain when untreated. Named as “mini-stroke”. The medications used in this review are helpful for the treatment of the temporary blood disorder. According to the high blood pressure and cholesterol levels the chances in increase of TIA are in higher states. The review included a theoretical literature on the medication of the TIA. Conformation can be done by performing the specified diagnostic tests followed by disease profile.
REFERENCES:
1)Ferro, J. M.; et al., I.; Rodrigues, G.; Canhao, P.; Melo, T.P.; Oliveira, V.; Pinto, A.N.; Crespo, M.; Salgado, A.V. "Diagnosis of transient ischemic attack by the nonneurologist. A validation study", Stroke 1996; 27 (12): 2225–2229.
2)Easton, J. D.; et al., J. L.; Albers, G. W.; Alberts, M. J.; Chaturvedi, S.; Feldmann, E.; Hatsukami, T. S.; Higashida, R. T.; Johnston, S. C. "Definition and evaluation of transient ischemic attack: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association Stroke Council; Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing; and the Interdisciplinary Council on Peripheral Vascular Disease. The American Academy of Neurology affirms the value of this statement as an educational tool for neurologists", Stroke 2009; 40 (6): 2276–2293.
3)Coutts, S. B.; et al., M. D.; Simon, J. E.; Sohn, C. -H.; Scott, J. N.; Demchuk, A. M.; "Silent ischemia in minor stroke and TIA patients identified on MR imaging", Vision Study, Group, Neurology 2005; 65 (4): 513–517.
4) nhs.uk/Conditions/Transient-ischaemic-attack/Pages/Treatment.aspx
5)What is a TIA or transient ischemic attack? American Heart Association. Retrieved on 2010-03-07.
6) Transient Ischemic Attack MedLine Plus. Retrieved on 2010-03-07
7)NINA J. SOLENSKI, M.D., University of Virginia Health Sciences Center, Charlottesville, Virginia Am Fam Physician. 2004, Apr 1; 69 (7):1665-1674.
8)Johnston CS, Gress DR, Browner WS, Sidney S. Short-term prognosis after emergency department diagnosis of TIA. JAMA. 2000; 284:2901–6.
9)2013 Bristol-Myers Squibb Company, All Rights Reserved
10)Drugs for lipids. Treatment Guidelines From The Medical Letter, 2011; 9(103): 13–20.
11)Grundy SM, et al. Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III), Executive summary of the third report of the National Cholesterol Education Program (NCEP) Expert Panel, JAMA, 2001; 285(19): 2486–2497.
12)NICE. Stroke: diagnosis and initial management of acute stroke and transient ischaemic attack (TIA). London, NICE, 2008.
13)Pendlebury ST, Rothwell PM. Risk of recurrent stroke, other vascular events and dementia after transient ischaemic attack and stroke. Cerebrovasc Dis 2009; 27 Suppl 3: 1-11.
14)Albers GW, Hart RG, Lutsep HL, Newell DW, Sacco RL. AHA scientific statement. Supplement to the guidelines for the management of transient ischemic attacks: a statement from the Ad Hoc Committee on Guidelines for the Management of Transient Ischemic Attacks, Stroke Council, American Heart Association. Stroke. 1999; 30:2502–11.
15)Culebras A, Kase CS, Masdeu JC, Fox AJ, Bryan RN, Grossman CB, et al. Practice guidelines for the use of imaging in transient ischemic attacks and acute stroke. A report of the Stroke Council, American Heart Association. Stroke. 1997;28:1480–97.
16)Elkins JS, Sidney S, Gress DR, Go AS, Bernstein AL, Johnston SC. Electrocardiographic findings predict short-term cardiac morbidity after transient ischemic attack. Arch Neurol. 2002; 59:1437–41.
17)Echocardiographic predictors of stroke in patients with atrial fibrillation: a prospective study of 1066 patients from 3 clinical trials. Arch Intern Med. 1998; 158:1316–20.
18) O'Brien PJ, Thiemann DR, McNamara RL, Roberts JW, Raska K, Oppenheimer SM, et al. Usefulness of trans-esophageal echocardiography in predicting mortality and morbidity in stroke patients without clinically known cardiac sources of embolus. Am J Cardiol. 1998; 81:1144–51.
19)Labovitz AJ. Transesophageal echocardiography and unexplained cerebral ischemia: a multicenter follow-up study. The STEPS Investigators. Significance of Transesophageal Echocardiography in the Prevention of Recurrent Stroke. Am Heart J. 1999; 137:1082–7.
20)Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Lancet. 1994; 344:1383–9.
21)Plehn JF, Davis BR, Sacks FM, Rouleau JL, Pfeffer MA, Bernstein V, et al. Reduction of stroke incidence after myocardial infarction with pravastatin: the Cholesterol and Recurrent Events (CARE) study. The CARE Investigators. Circulation. 1999; 99: 216–23.
22)Adams RJ, Chimowitz MI, Alpert JS, Awad IA, Cerqueria MD, Fayad P, et al. Coronary risk evaluation in patients with transient ischemic attack and ischemic stroke: a scientific statement for healthcare professionals from the Stroke Council and the Council on Clinical Cardiology of the American Heart Association/American Stroke Association. Circulation. 2003; 108: 1278–90.
23)Bhadelia RA, Bengoa R, Gesner L, Patel SK, Uzun G, Wolpert SM, et al. Efficacy of MR angiography in the detection and characterization of occlusive disease in the vertebrobasilar system.J Comput Assist Tomogr. 2001; 25: 458–65.
24)Korogi Y, Takahashi M, Nakagawa T, Mabuchi N, Watabe T, Shiokawa Y, et al. Intracranial vascular stenosis and occlusion: MR angiographic findings. AJNR Am J Neuroradiol. 1997; 18: 135–43.
25) Hankey GJ, Warlow CP, Sellar RJ. Cerebral angiographic risk in mild cerebrovascular disease.Stroke. 1990; 21:209–22.
26)Willinsky RA, Taylor SM, Ter Brugge K, Farb RI, Tomlinson G, Montanera W. Neurologic complications of cerebral angiography: prospective analysis of 2, 899 procedures and review of the literature. Radiology. 2003; 227:522–8.
27) Dion JE, Gates PC, Fox AJ, Barnett HJ, Blom RJ. Clinical events following neuroangiography: a prospective study. Stroke. 1987; 18:997–1004.
28) Young N, Chi KK, Ajaka J, McKay L, O'Neill D, Wong KP. Complications with outpatient angiography and interventional procedures. Cardiovasc Intervent Radiol. 2002; 25:23–126.
REFERENCE ID: PHARMATUTOR-ART-2216
|
PharmaTutor (ISSN: 2347 - 7881) Volume 2, Issue 8 Received On: 30/05/2014; Accepted On: 02/06/2014; Published On: 01/08/2014How to cite this article: V Sravanthi, VK Mayure, D Kalyan, GJ Finny, CP Meher; Mini-Stroke (TIA): A Review; PharmaTutor; 2014; 2(8); 87-94 |
NOW YOU CAN ALSO PUBLISH YOUR ARTICLE ONLINE.
SUBMIT YOUR ARTICLE/PROJECT AT articles@pharmatutor.org
Subscribe to Pharmatutor Alerts by Email
FIND OUT MORE ARTICLES AT OUR DATABASE









